Early Symptoms of Colon Cancer
- Understanding Transverse Colon Cancer
- Symptoms and Early Warning Signs
- Diagnostic Approaches
- Staging and Prognosis
- How Transverse Colon Cancer Differs from Other Colorectal Tumors
- Diagnosis Techniques Used in Detecting Transverse Colon Cancer
- Stages of Transverse Colon Cancer: From Local to Advanced
- Treatment Strategies Tailored to Transverse Colon Cancer
- Prognostic Factors Affecting Transverse Colon Cancer Outcomes
- Understanding Genetic and Molecular Markers in Tumor Progression
- Surgical Techniques and Their Role in Curative Treatment
- Challenges in Detecting Early Symptoms of Transverse Colon Cancer
- Imaging and Diagnostic Tests for Confirming Transverse Colon Cancer
- Treatment Options Based on Cancer Stage and Tumor Biology
- Chemotherapy Regimens and Potential Side Effects
- Transverse Colon Cancer and Other Colon Subtypes
- Patterns of Metastasis in Transverse Colon Cancer
- Prognosis and Life Expectancy by Stage
- Emotional and Psychological Impact of Diagnosis
- Surgical Techniques and Lymph Node Evaluation Standards
- FAQ
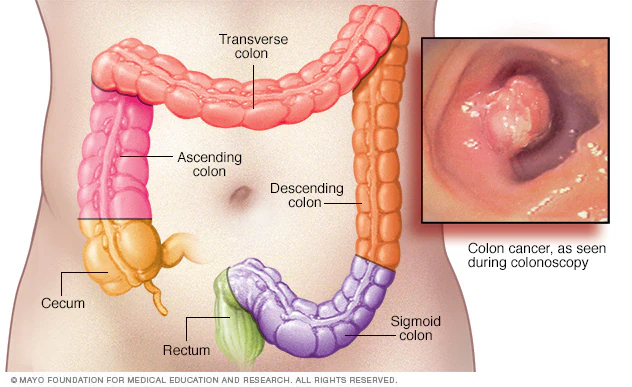
Understanding Transverse Colon Cancer
Transverse colon cancer is a malignancy that arises in the transverse section of the colon, which runs horizontally across the abdomen. This segment connects the ascending colon on the right side to the descending colon on the left. Due to its central location, tumors in this area can be challenging to detect early, often leading to delayed diagnoses.
The transverse colon is suspended by the transverse mesocolon, allowing for a degree of mobility within the abdominal cavity. This anatomical feature can influence the presentation and progression of cancer in this region. Additionally, the blood supply and lymphatic drainage of the transverse colon are derived from both the superior and inferior mesenteric arteries, which has implications for surgical planning and the potential spread of cancer cells.
Symptoms and Early Warning Signs
Early-stage transverse colon cancer often presents with nonspecific symptoms, making it difficult to distinguish from other gastrointestinal disorders. Common symptoms include intermittent abdominal discomfort, bloating, and changes in bowel habits such as alternating constipation and diarrhea. As the tumor grows, it may lead to more pronounced symptoms like unexplained weight loss, fatigue, and iron-deficiency anemia due to occult bleeding.
Given the overlap of these symptoms with conditions like irritable bowel syndrome (IBS), it’s crucial to seek medical evaluation for persistent or worsening gastrointestinal issues. A recent article highlighted the importance of differentiating between IBS and colon cancer, emphasizing that while IBS is a functional disorder, colon cancer involves malignant cell growth requiring prompt treatment.
Diagnostic Approaches
Diagnosing transverse colon cancer typically involves a combination of endoscopic and imaging techniques. Colonoscopy remains the gold standard, allowing direct visualization of the colon’s interior and the opportunity to obtain biopsy samples. However, due to the transverse colon’s mobility and position, complete visualization can sometimes be challenging.
In such cases, imaging studies like computed tomography (CT) scans or magnetic resonance imaging (MRI) are employed to assess the extent of the disease and identify any metastases. These imaging modalities are crucial for accurate staging, which guides treatment decisions.
Staging and Prognosis
The staging of transverse colon cancer follows the TNM classification system, which evaluates the tumor’s size and extent (T), involvement of regional lymph nodes (N), and presence of distant metastases (M). Accurate staging is essential for determining the most appropriate treatment strategy and providing prognostic information.
According to the American Cancer Society, the five-year relative survival rate for localized colorectal cancer is approximately 90.9%. However, this rate decreases significantly with regional spread (73.4%) and distant metastases (15.6%).

How Transverse Colon Cancer Differs from Other Colorectal Tumors
Although all colorectal cancers share a common origin in the epithelial lining of the large intestine, transverse colon cancer behaves differently in terms of progression, surgical management, and symptom patterns. Its anatomical placement means that tumors often grow into the mesocolon and adjacent structures, which can obscure early symptoms. Compared to cancers in the rectum or sigmoid colon, transverse colon malignancies more frequently present with systemic symptoms like fatigue and anemia rather than obvious rectal bleeding.
Moreover, because it receives dual vascular supply from both the middle colic branch of the superior mesenteric artery and the left colic branch of the inferior mesenteric artery, tumor resection may require more extensive surgical planning. These differences underscore the need for highly individualized approaches to diagnosis and treatment.
Diagnosis Techniques Used in Detecting Transverse Colon Cancer
Diagnosis typically begins with a physical exam and symptom assessment, but the cornerstone is imaging and endoscopy. A colonoscopy allows for direct visualization of the inner colon lining and tissue biopsy, even though accessing the transverse section can be technically more challenging than other parts of the colon. In some cases, a complete colonoscopy may fail to reach the transverse colon, leading to reliance on CT colonography or a double-contrast barium enema.
Cross-sectional imaging, such as CT scans and MRI, is crucial for staging and assessing local invasion or lymph node involvement. PET scans may be used when metastasis is suspected, especially in evaluating distant spread to the liver or lungs. Additionally, blood tests such as carcinoembryonic antigen (CEA) levels can help monitor treatment response or detect recurrence.

Stages of Transverse Colon Cancer: From Local to Advanced
The staging of transverse colon cancer follows the standard TNM system—Tumor size and invasion (T), lymph Node involvement (N), and distant Metastasis (M). Below is a breakdown of the stages and their implications:
| Stage | Tumor Characteristics | Lymph Node Involvement | Metastasis | Clinical Implication |
| Stage 0 | Cancer is confined to the inner lining (in situ) | None | None | Often removed during polyp excision |
| Stage I | Grown into submucosa or muscularis propria | None | None | Good prognosis with surgery |
| Stage II | Penetrated outer layers or nearby organs | No nodes involved | None | May require chemo post-surgery |
| Stage III | Any depth, but with regional lymph node spread | Yes | None | Standard chemo plus surgery |
| Stage IV | Spread to distant organs (commonly liver) | Yes/No | Yes | Complex, palliative or aggressive therapy |
Treatment Strategies Tailored to Transverse Colon Cancer
Treatment usually starts with surgical resection, which involves removing the affected section of the colon (extended right or left hemicolectomy depending on tumor location) and nearby lymph nodes. Because of its position, achieving clear margins and maintaining healthy bowel function requires careful planning.
Chemotherapy is often recommended post-surgery for stage II cases with high-risk features and almost always for stages III and IV. The commonly used regimens include FOLFOX (5-FU, leucovorin, oxaliplatin) and CAPOX (capecitabine and oxaliplatin). Targeted therapies such as bevacizumab may be added depending on genetic profiling.
For advanced-stage cases or those with metastasis to the liver—a common site—treatment might also include hepatic resection, radiofrequency ablation, or stereotactic body radiation therapy (SBRT). This is particularly relevant when comparing how different types of cancers behave in the liver, as discussed in our guide on stage 4 neuroendocrine cancer spread to liver life expectancy.
Prognostic Factors Affecting Transverse Colon Cancer Outcomes
Several variables significantly influence the prognosis of transverse colon cancer. The most important among these are tumor stage at diagnosis, lymph node involvement, molecular markers, and the patient’s general health. For example, Stage I patients often experience over 90% five-year survival, while those with Stage IV disease and liver metastases may see less than 15% survival depending on treatment response.
Molecular and genetic testing can also reveal mutations such as KRAS, NRAS, or BRAF, which may predict resistance to certain biologics. Tumor grade—whether well, moderately, or poorly differentiated—also correlates with aggressiveness. Patient-specific factors such as age, comorbidities, and immune status further modulate prognosis, and postoperative complications or incomplete resections reduce survival chances significantly.
Understanding Genetic and Molecular Markers in Tumor Progression
Modern oncology emphasizes the role of molecular profiling in customizing cancer treatment. In transverse colon cancer, microsatellite instability (MSI) and mutations in genes like KRAS, APC, and TP53 are frequently observed. MSI-high tumors, for example, may be less responsive to conventional chemotherapy but more susceptible to immune checkpoint inhibitors like pembrolizumab.
Genetic testing of biopsy samples or surgical specimens is now standard in determining eligibility for targeted therapies. This personalized medicine approach enables clinicians to choose regimens that offer the highest chance of remission while minimizing toxicity. It also opens a broader discussion about the possible influence of external or infectious agents in cancer development, such as the hypotheses explored in do parasites cause breast cancer.
Surgical Techniques and Their Role in Curative Treatment
Surgery remains the primary curative modality for localized transverse colon cancer. Depending on tumor location, a right or left extended hemicolectomy is performed. These procedures involve removing the cancerous segment along with surrounding mesocolon and lymph nodes to ensure clean margins.
The anastomosis (joining of the bowel ends) is carefully planned to preserve bowel function and reduce complications like leakage or obstruction. Minimally invasive laparoscopic techniques have become more common, offering quicker recovery and fewer complications, but open surgery remains standard for complex or bulky tumors. In emergency presentations—such as obstruction or perforation—urgent surgery may precede staging.
Challenges in Detecting Early Symptoms of Transverse Colon Cancer
Because of its mid-abdominal location, early-stage transverse colon cancer often remains asymptomatic or mimics benign gastrointestinal issues. Patients may report vague abdominal pain, bloating, or changes in stool shape that are frequently mistaken for irritable bowel syndrome (IBS). This diagnostic confusion delays detection and can lead to more advanced-stage discovery.
Furthermore, systemic symptoms such as unexplained fatigue, mild anemia, or weight loss tend to appear gradually. Blood in the stool is less frequent than in left-sided colon cancers, contributing to under-recognition. These overlaps in early presentation reinforce the need for a detailed differential diagnosis, which is further discussed in What is PTP1B in breast cancer, a marker increasingly explored for its role in tumor progression.
Imaging and Diagnostic Tests for Confirming Transverse Colon Cancer
Accurate diagnosis of transverse colon cancer requires a combination of imaging, endoscopy, and histopathological analysis. Colonoscopy is the gold standard for detecting masses, obtaining biopsies, and assessing synchronous lesions. Lesions in the transverse colon can sometimes be missed if bowel prep is inadequate or the scope cannot be fully advanced, emphasizing the need for experienced endoscopists.
Contrast-enhanced CT scans of the abdomen and pelvis are routinely used for staging, identifying tumor size, lymph node enlargement, and potential metastases. MRI may be helpful for evaluating liver involvement, especially in Stage IV cases. PET-CT is occasionally used when recurrence or distant metastasis is suspected, though not part of initial staging in all cases. Blood tests, including carcinoembryonic antigen (CEA), are not diagnostic alone but support monitoring treatment response and recurrence.
Treatment Options Based on Cancer Stage and Tumor Biology
Treatment for transverse colon cancer varies depending on the disease stage and biological markers. For early stages (I–II), surgical resection may be curative without the need for chemotherapy. Stage III patients, due to lymph node involvement, typically require adjuvant chemotherapy with regimens like FOLFOX (5-FU, leucovorin, and oxaliplatin).
In Stage IV cases, where metastases—often to the liver or lungs—are present, systemic chemotherapy is combined with targeted therapy when possible. Agents like bevacizumab (anti-VEGF) or cetuximab (anti-EGFR) are considered based on molecular profiling. Multidisciplinary teams assess whether metastases are resectable for curative intent or if palliative care is the primary goal.
While discussing treatment response, it’s relevant to note that concerns regarding therapeutic resistance mechanisms have been explored in other cancers.
Chemotherapy Regimens and Potential Side Effects
The most commonly used adjuvant and neoadjuvant chemotherapy regimens include FOLFOX and CAPOX (capecitabine and oxaliplatin). These combinations aim to reduce recurrence and improve survival, especially in Stage III and select high-risk Stage II patients. Duration typically spans six months, but may vary based on patient tolerance and emerging clinical trial data.
Common side effects include neutropenia, neuropathy, nausea, mucositis, and fatigue. Oxaliplatin-induced peripheral neuropathy can persist long after treatment ends and may limit further use. Capecitabine, an oral fluoropyrimidine, causes hand-foot syndrome and requires close dose monitoring. Pre-treatment evaluation of renal function, dihydropyrimidine dehydrogenase (DPD) status, and hepatic function is critical for minimizing toxicity.
Transverse Colon Cancer and Other Colon Subtypes
| Parameter | Transverse Colon Cancer | Right-Sided Colon Cancer | Left-Sided Colon Cancer |
| Typical Symptoms | Vague pain, bloating, anemia | Weight loss, anemia, diarrhea | Bleeding, change in bowel habits |
| Detection Difficulty | Moderate | Often late due to subtle symptoms | Easier due to bleeding |
| Molecular Markers | MSI, KRAS, TP53 | MSI-high more common | Chromosomal instability common |
| Treatment Strategies | Surgery + chemo (if Stage III) | Similar approach | Higher benefit from EGFR therapy |
| Prognosis at Same Stage | Intermediate | Generally worse | Slightly better |
This comparison helps clinicians understand the unique clinical behavior of transverse colon tumors, which are anatomically and biologically distinct from tumors located in other regions of the colon.
Patterns of Metastasis in Transverse Colon Cancer
Transverse colon cancer follows a metastatic pattern typical of colorectal tumors, with the liver being the most common site due to the portal circulation. Lung metastases are the next most frequent, followed by peritoneal carcinomatosis. Less commonly, metastases can involve bone, brain, or distant lymph nodes. The pattern and timing of metastasis often vary based on molecular features such as KRAS mutation or microsatellite instability (MSI).
Synchronous metastases, identified at initial diagnosis, often indicate aggressive disease biology and may prompt simultaneous resection of the primary tumor and metastases if feasible. Metachronous metastases, appearing months or years later, are usually treated with systemic therapy first, followed by local interventions like hepatic ablation or resection. Accurate imaging and regular surveillance are key to detecting these progressions early.
Prognosis and Life Expectancy by Stage
Prognosis in transverse colon cancer is heavily stage-dependent. For Stage I, five-year survival rates exceed 90%, while Stage II patients without high-risk features often achieve 75–85% survival. Stage III survival ranges between 50–65%, reflecting lymph node involvement. Stage IV survival, despite advances, remains significantly lower—typically between 10–20%, depending on metastatic burden and treatment response.
It’s important to emphasize that survival statistics are population-based and cannot precisely predict individual outcomes. Variables such as comorbidities, tumor biology, treatment access, and adherence all impact prognosis. Personalized prognostic tools, including nomograms and molecular assays, are increasingly integrated into care to refine individual expectations and guide follow-up. More about rare factors influencing oncogenesis here.
Emotional and Psychological Impact of Diagnosis
A diagnosis of transverse colon cancer can be psychologically overwhelming, particularly when it occurs at a younger age or in patients without family history. Anxiety, depression, and fear of recurrence are among the most commonly reported emotional responses. The physical impact of treatments such as surgery and chemotherapy can further contribute to distress, often leading to body image issues, fatigue-related withdrawal, or relationship strain.
Support systems, including psycho-oncology services, social workers, and peer support groups, play a vital role in improving mental health outcomes. In some healthcare settings, routine distress screening is conducted at each major phase of treatment to ensure no aspect of the patient’s emotional health is overlooked. This holistic care approach improves quality of life and often translates into better clinical compliance and outcomes.
Surgical Techniques and Lymph Node Evaluation Standards
Surgical resection remains the cornerstone of treatment for resectable transverse colon tumors. The standard procedure is segmental transverse colectomy or extended right/left hemicolectomy, depending on tumor proximity to flexures. High ligation of the middle colic vessels ensures adequate lymphadenectomy, which is essential for accurate staging and oncologic clearance.
Current guidelines recommend that at least 12 lymph nodes be evaluated to consider the surgery oncologically adequate. However, data show that more extensive nodal dissection (20+ nodes) may improve staging accuracy and long-term survival. Enhanced recovery after surgery (ERAS) protocols have also significantly improved postoperative outcomes, reducing complication rates and hospital stay. What is PTP1B in breast cancer — in the context of discussing molecular factors influencing treatment.
FAQ
What are the early symptoms of transverse colon cancer?
Early symptoms of transverse colon cancer are often vague or nonspecific, which can delay diagnosis. Patients may report intermittent abdominal pain, bloating, fatigue, and occasional changes in bowel habits such as constipation or diarrhea. Because the transverse colon spans the upper abdomen, discomfort may be mistaken for indigestion or gastric issues, and visible rectal bleeding is less common in early stages.
How is transverse colon cancer typically diagnosed?
Diagnosis begins with a combination of clinical history, physical examination, and laboratory testing, such as checking for anemia or elevated carcinoembryonic antigen (CEA) levels. However, colonoscopy is the gold standard, allowing direct visualization and biopsy. Imaging studies such as contrast-enhanced CT scans help evaluate tumor spread and lymph node involvement, while MRI or PET-CT may be employed for advanced staging.
What distinguishes transverse colon cancer from other colon cancers?
Its central anatomical location affects both its presentation and surgical approach. Unlike left-sided cancers, which often cause obstruction, transverse tumors are more likely to cause vague discomfort and anemia due to occult bleeding. Surgically, the transverse colon’s proximity to the middle colic vessels and its variable lymphatic drainage make resections more technically demanding.
Can lifestyle factors influence the development of transverse colon cancer?
Yes, several modifiable lifestyle factors contribute to colorectal cancer risk, including diets high in red or processed meat, low fiber intake, obesity, alcohol use, and smoking. Physical inactivity and chronic inflammation from conditions like inflammatory bowel disease also play a role. Adopting a Mediterranean-style diet and engaging in regular exercise may reduce the risk over time.
Is genetic testing recommended for patients with transverse colon cancer?
Genetic testing is considered if the patient is diagnosed before age 50, has multiple relatives with colorectal or related cancers, or presents with features suggestive of Lynch syndrome or familial adenomatous polyposis. Identifying hereditary cancer syndromes can influence treatment decisions, such as the extent of resection, and guide surveillance strategies for family members.
What role does chemotherapy play in treatment?
Adjuvant chemotherapy is standard for Stage III and selected Stage II cases with high-risk features. It targets microscopic disease and reduces recurrence risk. For Stage IV cases, chemotherapy is the mainstay of treatment, sometimes combined with targeted therapies. The regimen typically includes 5-fluorouracil, oxaliplatin, or irinotecan, and may be personalized based on tumor genetics.
How effective is immunotherapy for transverse colon cancer?
Immunotherapy, particularly immune checkpoint inhibitors, has shown promise in patients whose tumors exhibit microsatellite instability-high (MSI-H) or mismatch repair deficiency (dMMR). These biologic traits are more common in right-sided or proximal colon cancers. While not standard for all patients, testing for MSI status is now routine in colorectal cancer management.
What are common complications after surgery?
Postoperative complications can include infection, bleeding, anastomotic leakage, or bowel obstruction. Less commonly, patients may experience delayed gastric emptying or prolonged ileus due to the transverse colon’s proximity to the stomach. With the use of ERAS protocols, complication rates have declined, and most patients are discharged within 5–7 days post-surgery.
How often should patients undergo follow-up after treatment?
Follow-up protocols vary by stage but generally include CEA testing every 3–6 months, annual CT scans, and colonoscopy at 1 year after surgery, then every 3–5 years. The purpose is to detect recurrences early or monitor for metachronous tumors. High-risk patients may require more intensive surveillance depending on pathology findings and genetic markers.
Can transverse colon cancer return after treatment?
Yes, recurrence is possible, particularly within the first three years after surgery. Local recurrence can occur at the anastomotic site or in regional lymph nodes, while distant recurrence often involves the liver or lungs. Early detection through surveillance imaging and prompt treatment—such as resection or systemic therapy—can significantly impact outcomes.
Does transverse colon cancer affect men and women equally?
While overall colorectal cancer incidence is slightly higher in men, transverse colon cancer does not show a marked gender bias. However, symptom perception and healthcare-seeking behavior may vary between men and women, occasionally resulting in delayed diagnosis in female patients due to symptom overlap with gynecologic conditions.
What is the typical age range for diagnosis?
Most cases are diagnosed in individuals over 60, although rates in younger adults have been increasing over the past two decades. Early-onset colorectal cancer often presents with more aggressive features and is more likely to be associated with genetic syndromes, warranting a different clinical approach to management and family screening.
Is radiation therapy used in transverse colon cancer?
Radiation is not routinely used in colon cancer due to its anatomical mobility and the surrounding sensitive structures. However, in rare cases where tumors invade adjacent organs or recur locally and are not resectable, radiation may be considered for palliation or disease control, usually in conjunction with chemotherapy.
What is the survival rate for patients with metastatic disease?
For patients with Stage IV transverse colon cancer, median overall survival typically ranges from 24 to 36 months with modern therapy. Those eligible for curative metastasectomy—especially of liver metastases—can exceed five-year survival in 20–40% of cases. Response to chemotherapy and access to advanced treatments significantly influence long-term outcomes.
Are tattoo pigments linked to colorectal cancer?
While this is a common concern, there is no direct evidence linking tattoo pigments to colon cancer. However, concerns exist about certain ink components possibly containing carcinogenic substances. Ongoing studies explore these long-term effects, especially in relation to systemic absorption.












