Early Skin Metastases in Breast Cancer: Identification, Diagnosis, and Management
- Introduction to Skin Metastases in Breast Cancer
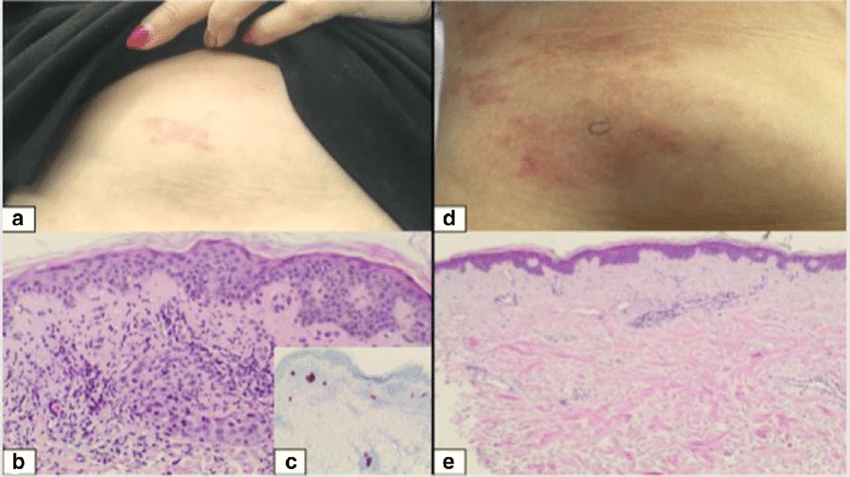
- Clinical Appearance of Early Cutaneous Metastases
- Pathophysiology Behind Skin Spread in Early Disease
- Diagnostic Workup: Imaging and Biopsy Considerations
- Histological Features and Subtype Correlation
- Prognostic Implications of Early Cutaneous Spread
- Treatment Modalities for Early Skin Metastases
- Common Clinical Features vs. Histologic Subtype
- Role of Imaging in Detecting Cutaneous Metastases
- Skin Biopsy Techniques and Diagnostic Yield
- Systemic Disease Monitoring and Recurrence Patterns
- Symptom Management and Palliative Considerations
- Impact of Hormone Receptor Status on Skin Metastasis Behavior
- Cutaneous Metastases vs. Benign Dermatologic Conditions
- Treatment Response Expectations and Timelines
- Prognosis and Long-Term Outcomes with Cutaneous Involvement
- FAQ
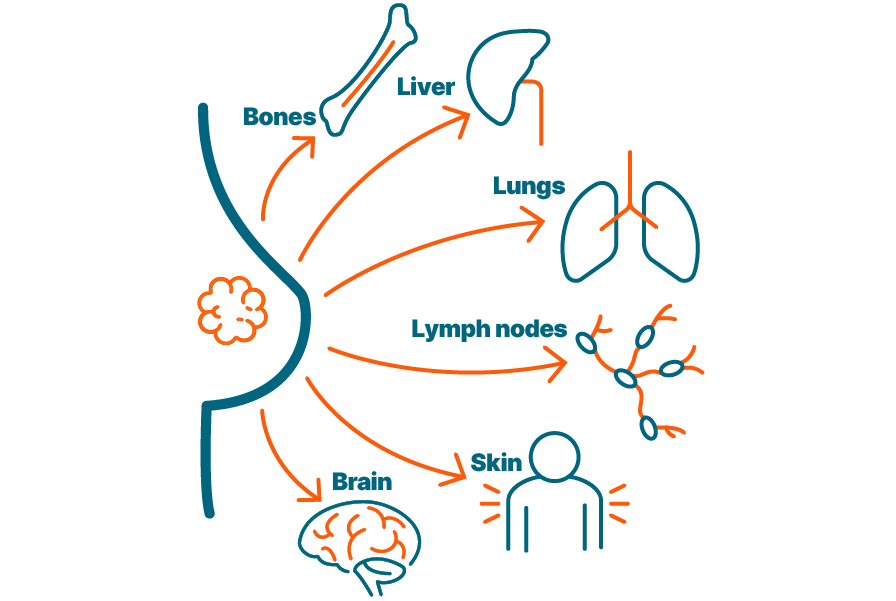
Introduction to Skin Metastases in Breast Cancer
Skin metastases from breast cancer occur when cancer cells spread from the original tumor site to the skin, often signaling progression or recurrence. In early breast cancer, these cutaneous manifestations are rare but clinically significant, requiring immediate attention. While breast cancer commonly spreads to bones, lungs, liver, and brain, skin metastases offer a visible and often early external clue. These lesions can mimic benign conditions such as dermatitis or infections, making early diagnosis challenging without clinical suspicion and biopsy confirmation. Understanding the presentation and pathology of these metastases allows clinicians and patients to act promptly, possibly improving outcomes even in the context of disease spread.
Clinical Appearance of Early Cutaneous Metastases
The presentation of skin metastases in early breast cancer can vary widely, both in location and form. Typically, the lesions develop near the original tumor or surgical scar, but distant cutaneous sites are also possible. Early manifestations may appear as firm, painless nodules, slightly raised or flat, and skin-colored, pink, or purplish. Some may ulcerate or cause localized inflammation. These characteristics can be deceptive, particularly in women undergoing or recently finishing treatment, where skin changes are expected due to radiation or chemotherapy. Proper differentiation from inflammatory breast cancer or recurrence at the scar line requires dermatological and oncological collaboration.
Pathophysiology Behind Skin Spread in Early Disease
The mechanism by which breast cancer spreads to the skin involves lymphatic and hematogenous routes. Early metastasis may be facilitated by tumor cells gaining access to dermal lymphatics, especially if prior surgery or radiation therapy altered normal lymphatic drainage. Some subtypes, such as HER2-positive and triple-negative breast cancers, are more aggressive and prone to distant or cutaneous spread even at early stages. Tumor cell plasticity, epithelial-mesenchymal transition (EMT), and molecular signaling pathways such as VEGF and CXCR4 are involved in the migration and anchoring of malignant cells in the skin. Research on immune evasion and exhaustion, similar to what’s observed in lewis lung cancer and t cell exhaustion, further deepens the understanding of how early metastases may occur.
Diagnostic Workup: Imaging and Biopsy Considerations
Once skin changes are noted in a breast cancer patient, especially post-treatment, an urgent diagnostic approach is essential. Clinical examination is followed by dermoscopy or high-resolution photography for documentation. A skin biopsy—either punch or excisional—is performed to obtain histologic confirmation. The pathology typically reveals malignant epithelial cells in the dermis, sometimes forming glandular structures. Immunohistochemical staining helps distinguish skin metastases from primary skin tumors, showing markers like cytokeratin 7, estrogen receptor (ER), progesterone receptor (PR), and HER2. Imaging modalities such as PET-CT or breast MRI may be required to rule out systemic spread, especially if cutaneous metastases appear isolated. As seen in broader staging processes, technologies like PET scans, which are often questioned for their role in gastrointestinal cancers, remain highly valuable in breast cancer evaluation.

Histological Features and Subtype Correlation
The histopathological assessment of skin metastases in breast cancer provides critical insights into the tumor’s behavior and subtype. Metastatic lesions usually demonstrate infiltration of the dermis or subcutaneous tissue by malignant epithelial cells. These cells may be arranged in cords, nests, or gland-like structures, depending on the primary tumor’s histology. Certain subtypes—such as invasive ductal carcinoma—tend to maintain their original architecture, making recognition more straightforward. However, lobular carcinoma can be more insidious, with cells infiltrating singly and mimicking benign dermatoses. Immunohistochemistry plays an essential role in confirming the breast origin of metastases, particularly when the patient has a history of multiple primaries or when the presentation is ambiguous. Markers such as GATA3, mammaglobin, and GCDFP-15 help establish breast origin in conjunction with traditional hormone receptors and HER2. Understanding this correlation enhances accuracy in subclassifying disease and tailoring treatment.
Prognostic Implications of Early Cutaneous Spread
The presence of skin metastases, even in early breast cancer, typically suggests a more aggressive or treatment-resistant disease course. However, prognosis depends heavily on the extent and context of spread. Isolated skin metastases in a patient with no visceral involvement may have a more favorable outlook compared to those with concurrent systemic disease. In some cases, early skin involvement serves as the first indicator of an undetected local recurrence or minimal residual disease post-surgery. The molecular subtype also greatly influences outcomes—triple-negative cancers with skin spread tend to recur more rapidly and respond poorly to conventional therapies. HER2-positive cases, while aggressive, often respond well to targeted agents. Overall survival and disease-free intervals tend to shorten with cutaneous involvement, but aggressive multidisciplinary treatment can still improve quality of life and symptom control.
Treatment Modalities for Early Skin Metastases
Managing skin metastases in early breast cancer requires a multimodal approach. Local therapies include surgical excision of small, well-circumscribed lesions, especially when they are isolated. Radiation therapy remains a powerful option for localized or symptomatic cutaneous involvement, helping reduce lesion burden and alleviate discomfort. Systemic therapy is critical, especially in patients with multiple lesions or high-risk histologic features. Hormonal therapy, chemotherapy, HER2-directed agents, and more recently, immunotherapy, are used based on the receptor status and disease burden. For patients with ER-positive disease, agents like tamoxifen or aromatase inhibitors may control cutaneous spread. In HER2-positive cases, trastuzumab or pertuzumab-based regimens offer both local and systemic control. When discussing complementary interventions, it’s worth comparing how these strategies align with alternative cancer treatments for dogs, where integrative medicine is also becoming more accepted.
Common Clinical Features vs. Histologic Subtype
| Clinical Presentation | Likely Histologic Subtype | Receptor Status | Treatment Sensitivity |
| Firm nodular lesions | Invasive Ductal Carcinoma | ER+/PR+/HER2– | Hormonal Therapy |
| Multiple inflamed plaques | Inflammatory Breast Cancer | Variable (often HER2+) | Chemotherapy + HER2-Targeted |
| Diffuse erythema with edema | Lobular Carcinoma | ER+/PR+/HER2– | Hormonal ± Chemotherapy |
| Ulcerated skin nodules | Triple-Negative Breast Cancer | ER–/PR–/HER2– | Chemotherapy ± Immunotherapy |
| Peri-surgical scar nodules | Local Recurrence (Any Subtype) | Subtype-dependent | Local + Systemic as indicated |
This table illustrates how clinical appearances may offer diagnostic clues that correspond with specific breast cancer subtypes, aiding in quicker therapeutic decision-making and patient counseling.
Role of Imaging in Detecting Cutaneous Metastases
While skin metastases from breast cancer are often visible or palpable on physical examination, imaging plays a crucial role in confirming their extent, underlying tissue involvement, and relation to the primary tumor or surgical scars. High-resolution ultrasound is particularly valuable for evaluating subcutaneous nodules, especially in dense breast tissue or in regions with previous surgeries where fibrosis may mask recurrence. Mammography may not detect cutaneous lesions unless they extend into deeper layers. MRI, with contrast enhancement, provides superior delineation of the dermal and subdermal spread, especially in complex anatomical zones such as the chest wall. PET/CT scans help evaluate metabolic activity of skin lesions and determine whether systemic spread is also present. In fact, this imaging modality is often used when other subtle symptoms suggest recurrence, as seen in some colon cancers evaluated by PET, where minimal signs turn out to have clinical significance.
Skin Biopsy Techniques and Diagnostic Yield
When skin metastasis is suspected, performing a skin biopsy is essential for diagnosis. Punch biopsy is the most commonly employed technique due to its ability to retrieve full-thickness dermal and subdermal tissue while maintaining minimal patient discomfort. Incisional biopsy may be needed for larger or more infiltrative lesions. Shave biopsies are generally avoided because they may not reach the metastatic layer and can yield inconclusive results. Histologic evaluation should be followed by immunohistochemical staining to confirm the breast origin and determine receptor status. The diagnostic yield is generally high if an appropriate technique is used and a representative lesion is sampled. Accurate biopsy not only confirms the diagnosis but also guides treatment planning, distinguishing between recurrence, second primaries, or benign inflammatory conditions.
Systemic Disease Monitoring and Recurrence Patterns
The appearance of skin metastases, particularly in early-stage or post-surgical patients, may represent either the first sign of recurrence or coexist with other systemic lesions. Monitoring protocols must therefore include periodic full-body evaluations. Blood work, imaging studies, and physical examination of skin and lymph node basins become integral to follow-up. Recurrence may follow a pattern—often beginning locally around surgical scars, then extending to dermal lymphatics, and finally manifesting in other organ systems. Surveillance strategies may be adjusted based on risk stratification. For instance, HER2-positive or triple-negative patients typically undergo more frequent monitoring. Understanding recurrence behavior can also help draw parallels with other aggressive skin-involving malignancies, such as those seen in lewis lung cancer with T-cell exhaustion mechanisms, which similarly bypass local immune responses.
Symptom Management and Palliative Considerations
Even in early-stage disease, cutaneous metastases may cause significant discomfort, both physical and psychological. Lesions can ulcerate, bleed, or become infected, necessitating local wound care and sometimes systemic antibiotics. Pain management may involve topical agents, oral analgesics, or even nerve blocks if deeper tissue involvement is present. Itching, burning, or tightness from skin infiltration may severely affect quality of life. Emotional distress, body image concerns, and anxiety are common and should not be underestimated. Multidisciplinary teams including oncologists, dermatologists, palliative care specialists, and counselors are essential in comprehensive care. Early symptom intervention can drastically improve daily functioning and mental well-being, even before disease-modifying therapies show results.
Impact of Hormone Receptor Status on Skin Metastasis Behavior
Hormone receptor status—namely estrogen receptor (ER), progesterone receptor (PR), and HER2/neu—plays a pivotal role in determining the behavior of breast cancer, including its metastatic tendencies and treatment response. In skin metastases, ER-positive tumors tend to present later and may be more indolent, while triple-negative subtypes often manifest earlier with more aggressive dermal involvement. HER2-positive tumors, although historically aggressive, now benefit from targeted therapies that may reduce cutaneous recurrence. Understanding receptor dynamics is crucial, as skin lesions may differ in expression from the original tumor, especially in recurrent or previously treated cases. Biopsy of the skin lesions with repeated receptor profiling helps refine systemic treatment and better predict progression. Receptor heterogeneity in skin mets is a known phenomenon and may warrant therapy adjustment even in early cutaneous spread.
Cutaneous Metastases vs. Benign Dermatologic Conditions
| Feature | Cutaneous Metastases | Benign Skin Conditions |
| Onset | Often rapid | Typically gradual |
| Appearance | Firm nodules, erythematous or violaceous | Variable—can be scaly, flat, or cystic |
| Distribution | Often near surgical scars or chest wall | Anywhere, often symmetric |
| Symptoms | May be painful, ulcerated, non-pruritic | Often itchy, rarely painful |
| Biopsy findings | Malignant epithelial cells in dermis | Benign epidermal or inflammatory features |
| Response to treatment | Requires systemic oncology-directed therapy | Often resolves with topical or oral dermatologic treatment |
This differentiation is critical as misdiagnosis can delay appropriate cancer care. Dermatologists and oncologists must work together to distinguish between post-radiation dermatitis, infections, inflammatory dermatoses, and true metastasis, especially when changes are subtle or appear years after initial treatment.
Treatment Response Expectations and Timelines
Patients with early breast cancer skin metastases often ask what outcomes to expect once treatment begins. The response to therapy—be it systemic chemotherapy, hormone therapy, targeted agents, or immunotherapy—varies depending on tumor biology, disease extent, and prior treatments. In some cases, skin lesions regress visibly within weeks of initiating therapy. In others, particularly hormone receptor-positive lesions, response may be slower and require months to become evident. Continued skin changes despite therapy may suggest resistance or need for treatment modification. It’s essential to monitor both the visible lesions and underlying systemic markers to assess full response. Patients must be educated to understand that visible resolution is one component of disease control, and long-term remission often depends on sustained systemic therapy.
Prognosis and Long-Term Outcomes with Cutaneous Involvement
The prognosis of patients with skin metastases from breast cancer varies greatly. When such lesions appear early and in isolation, they may represent a manageable recurrence with targeted systemic treatment. However, in many cases, skin involvement reflects broader systemic disease and is associated with reduced overall survival. That said, new therapies—such as CDK4/6 inhibitors, trastuzumab-based regimens, and checkpoint inhibitors—have improved outcomes significantly, even in patients with dermal spread. A multidisciplinary care plan including medical oncologists, dermatologists, palliative teams, and mental health professionals can greatly impact quality and duration of life. Patients should also be informed that early detection of skin mets may offer a treatment window that delays progression—highlighting the same proactive diagnostic approach used in identifying metabolic changes in colon cancers through advanced scans.
FAQ
What are skin metastases from breast cancer?
Skin metastases occur when cancer cells from the original breast tumor spread to the skin, either near the initial tumor site or elsewhere on the body. These metastatic lesions are not new primary skin cancers but rather an extension of breast cancer that has traveled through the lymphatic system or bloodstream. They may appear months or years after the initial diagnosis and can signal recurrence or progression of disease.
How do early skin metastases from breast cancer typically appear?
In the early stages, skin metastases often manifest as small, firm, flesh-colored or reddish nodules, usually near surgical scars, the chest wall, or mastectomy sites. These lesions may grow slowly or quickly and often lack symptoms like itching or pain in the beginning. Their appearance can mimic benign skin conditions, making clinical evaluation and biopsy essential for accurate diagnosis.
Are early skin metastases painful or itchy?
In the early phase, these metastases are usually not painful or itchy. They may feel firm or rubbery to the touch and remain asymptomatic for some time. However, as the disease progresses or inflammation increases, they can become tender, ulcerated, or cause discomfort. Pruritus is less common unless there is secondary irritation or infection.
How are skin metastases from breast cancer diagnosed?
Diagnosis typically begins with a physical examination followed by a skin biopsy. This involves removing a small sample of the suspicious skin lesion and examining it under a microscope. Immunohistochemical staining may be used to confirm that the cells are indeed of breast cancer origin. In cases where diagnosis is uncertain, additional molecular testing may help determine the tumor profile and appropriate treatment plan.
Can skin metastases be the first sign of breast cancer?
While uncommon, it is possible for skin metastases to be the first noticeable manifestation of breast cancer, especially in cases where the primary tumor is small or missed on imaging. In such cases, biopsy of the skin lesion can lead to the discovery of an underlying, previously undiagnosed breast malignancy. However, more frequently, skin involvement occurs after an initial diagnosis and treatment of the primary breast cancer.
What treatment options are available for early-stage breast cancer skin metastases?
Treatment typically includes systemic therapy such as hormone therapy, chemotherapy, or targeted agents depending on the tumor’s receptor status (ER, PR, HER2). In some cases, localized treatments like radiation therapy or topical agents may be used to relieve symptoms or reduce lesions. The approach is individualized and may evolve as the disease responds or resists treatment.
Do skin metastases always mean advanced cancer?
Not necessarily. While skin involvement indicates that cancer cells have spread beyond the original site, early skin metastases can be limited and treatable, especially if they are the only sites of recurrence. Their presence should prompt thorough restaging to determine if there is additional internal spread, but early detection can offer a more favorable treatment window.
Can skin metastases be surgically removed?
Surgical excision is rarely the primary treatment for skin metastases, as these lesions are usually a sign of systemic disease. However, in select cases with isolated, bothersome, or cosmetically distressing lesions, surgical removal may be considered. This approach is typically reserved for situations where systemic therapy has controlled the rest of the disease or for palliation.
What is the role of radiation in treating breast cancer skin mets?
Radiation therapy can be effective in controlling local skin lesions that are painful, ulcerated, or non-responsive to systemic treatment. It may be used to reduce tumor burden, manage bleeding or discomfort, or prevent further spread in specific areas. The dose and schedule depend on lesion location, size, and overall treatment goals.
Do skin metastases respond to immunotherapy?
Some patients, particularly those with triple-negative breast cancer, may benefit from immunotherapy, especially agents targeting the PD-1/PD-L1 pathway. However, immunotherapy is still under investigation for broader use in breast cancer, and response rates vary. Skin metastases may show visible improvement with systemic immune checkpoint inhibitors in some cases.
Is prognosis worse with early skin involvement?
Skin metastases can indicate a more aggressive or recurrent form of breast cancer, but early detection and modern treatments have improved outcomes. Prognosis depends on multiple factors such as receptor status, response to therapy, and presence of metastases elsewhere. Isolated skin metastases without internal spread can have a more favorable outlook than widespread disease.
Can these lesions spread to deeper tissues or organs?
Yes, while cutaneous metastases begin in the skin, they can signify a potential for deeper invasion or progression to organs if left untreated. The presence of dermal involvement suggests that circulating tumor cells are active, and systemic surveillance is necessary to monitor for further metastatic spread.
How often should skin be monitored after breast cancer treatment?
Patients should conduct regular self-exams and attend all follow-up appointments with their oncology team. Any new skin lesions, especially near the surgical or radiation sites, should be reported promptly. Dermatologic evaluations may be advised in high-risk patients or those with a history of recurrence.
Can skin metastases be mistaken for infections or rashes?
Absolutely. Conditions like cellulitis, dermatitis, or even fungal infections may look similar to early metastatic lesions. This makes accurate diagnosis challenging without biopsy. In patients with a history of breast cancer, persistent or unusual skin changes should always raise suspicion and prompt further investigation.
Are there preventive strategies for skin metastases?
While there is no guaranteed way to prevent skin metastases, staying compliant with systemic treatment, attending regular follow-ups, and addressing recurrence promptly all help reduce the risk. Recognizing warning signs early and seeking timely medical evaluation improves the likelihood of successful management.













