Diverticulitis and Colon Cancer
Diverticulitis and Colon Cancer: Understanding the Link Between
- What Is Diverticulitis and How Does It Develop?
- What Is Colon Cancer and Why Is It Serious?
- Shared Symptoms Between Diverticulitis and Colon Cancer
- Can Diverticulitis Turn Into Colon Cancer?
- Diagnostic Challenges: When Diverticulitis Masks Cancer
- Imaging Tests: What They Can and Can’t Show
- Risk Factors: Who Is More Vulnerable to Both Conditions
- How Age and Diet Impact Both Conditions
- Preventive Screening After Diverticulitis
- Long-Term Outlook: Managing Risk After Recovery
- Role of Colonoscopy in Both Conditions
- Misdiagnoses: How Often Diverticulitis Hides Tumors
- Diet, Fiber, and Lifestyle in Prevention
- Understanding Your Pathology Report
- Diverticulitis vs. Colon Cancer in Clinical Records
- Summary: What to Do If You’re Diagnosed with Either
- 15+ Frequently Asked Questions (FAQ)
What Is Diverticulitis and How Does It Develop?
Diverticulitis is an inflammatory condition that affects the large intestine (colon), specifically when small pouches called diverticula become inflamed or infected. These pouches form over time, especially in the sigmoid colon, due to pressure on weakened areas of the bowel wall. When these pouches remain silent, the condition is referred to as diverticulosis. When they become inflamed, it is called diverticulitis.
The exact cause of diverticula formation isn’t fully understood, but aging, lack of fiber in the diet, and chronic constipation are key contributors. Episodes of diverticulitis can range from mild inflammation to severe infections requiring hospitalization or even surgery.
Understanding diverticulitis is crucial because its long-term consequences may include complications such as abscesses, perforations, fistulas — and a debated connection to colorectal cancer.
What Is Colon Cancer and Why Is It Serious?
Colon cancer, or colorectal cancer when it also includes the rectum, occurs when abnormal cells form tumors in the colon lining. It typically begins as small, benign polyps that gradually transform into cancer if not detected and removed early.
This form of cancer is one of the most common and deadly worldwide. According to the American Cancer Society, colon cancer is the second leading cause of cancer deaths in the United States for both men and women. However, with early detection, it is often highly treatable.
Because both colon cancer and diverticulitis affect the same organ and can share similar symptoms, understanding how they differ — and sometimes overlap — is essential for accurate diagnosis and treatment planning.
Shared Symptoms Between Diverticulitis and Colon Cancer
Many patients with diverticulitis fear it might lead to or mask colon cancer. This concern is justified, as both conditions can present with:
- Abdominal pain, often in the lower left quadrant
- Changes in bowel habits
- Rectal bleeding
- Unexplained fatigue
- Bloating or feeling of fullness
These overlapping symptoms can make it difficult to distinguish between a diverticular flare-up and early-stage colon cancer without proper imaging and tests.
Below is a comparison of their typical presentations:
| Symptom | Diverticulitis | Colon Cancer |
| Abdominal pain | Sudden, sharp, localized | Gradual, dull, sometimes cramp-like |
| Bowel habit changes | Constipation or diarrhea | Long-term changes, narrow stools |
| Blood in stool | Often bright red | Can be dark or mixed with stool |
| Fever | Common during flares | Rare in early stages |
| Weight loss | Rare unless complications arise | Common in advanced stages |
This symptom overlap is one reason doctors often recommend follow-up colonoscopies after a diverticulitis episode.
Can Diverticulitis Turn Into Colon Cancer?
Current research indicates that diverticulitis does not cause colon cancer, but the two conditions may coexist. One reason is that chronic inflammation, especially if left untreated, can alter the cellular environment of the colon, possibly contributing to changes in the tissue that resemble or mask early malignancy.
Moreover, patients who experience complicated or recurrent diverticulitis are more likely to undergo diagnostic imaging and colonoscopies — during which asymptomatic cancers may be discovered.
Importantly, some studies have noted that in rare cases, what appears to be diverticulitis on a CT scan is later diagnosed as colon cancer upon further investigation. This highlights the importance of follow-up exams to confirm the original diagnosis.
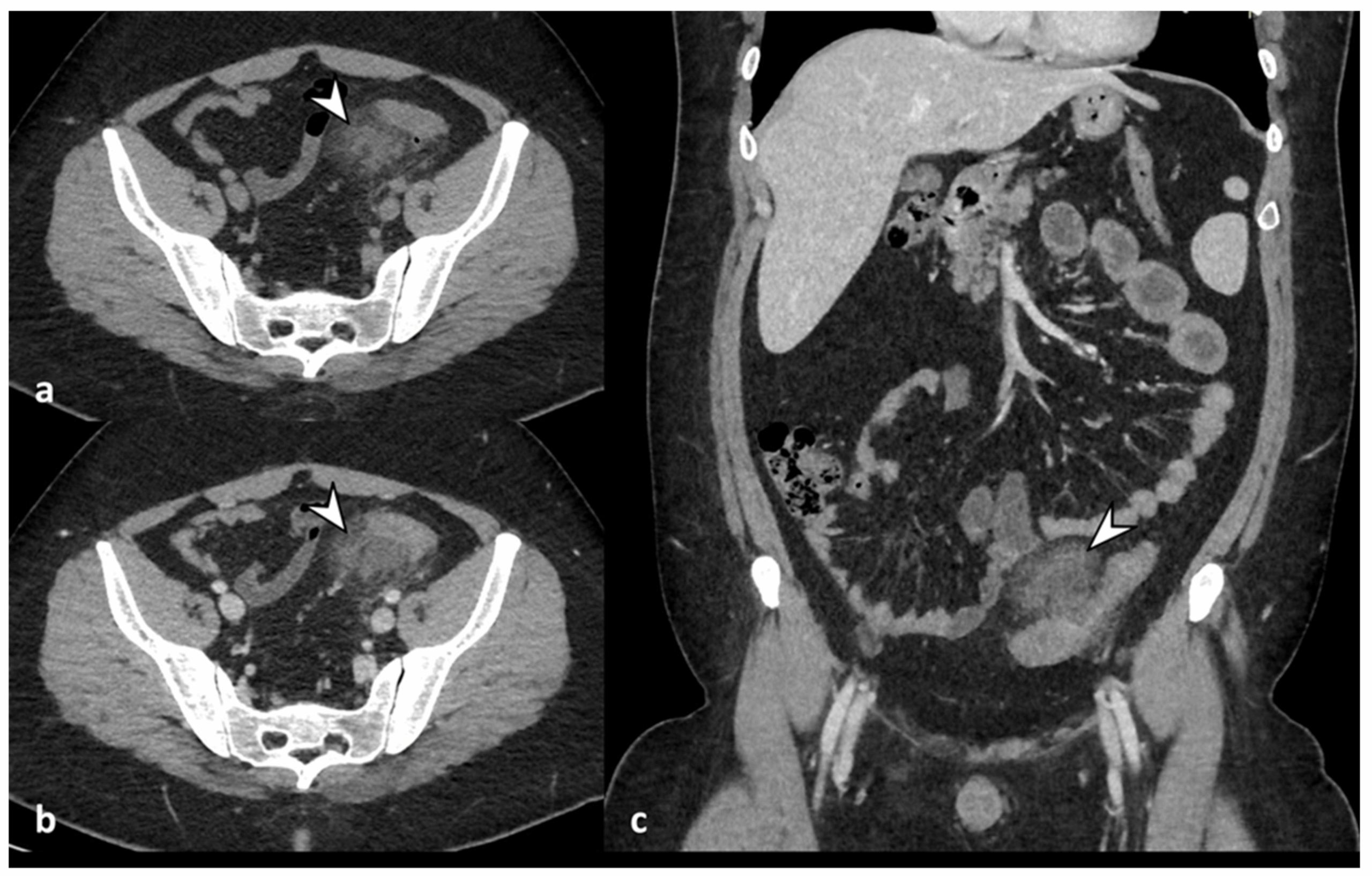
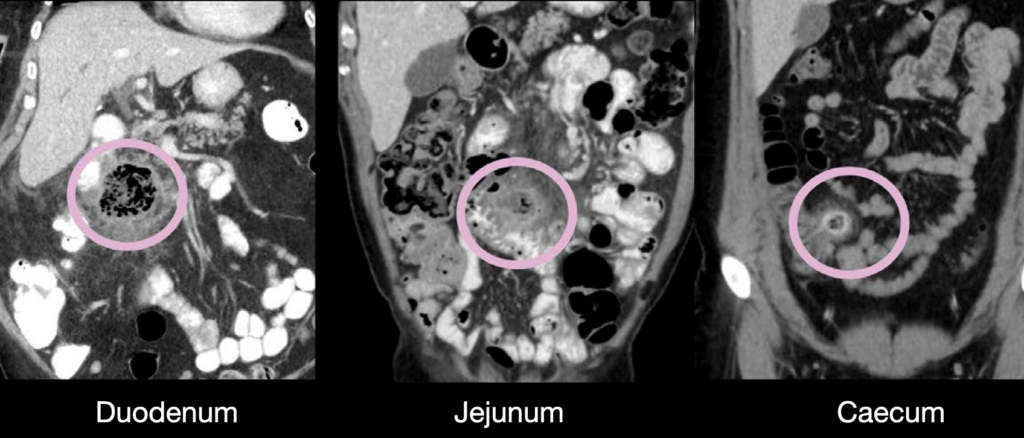
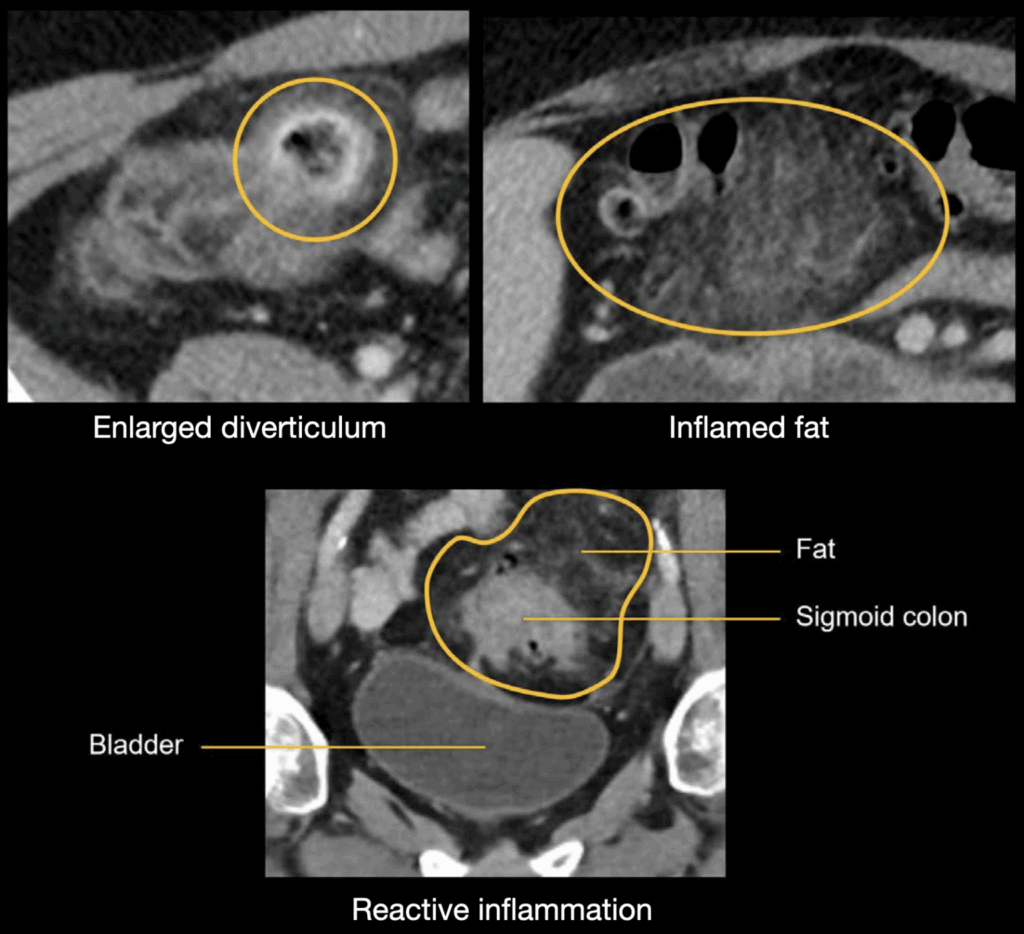
Diagnostic Challenges: When Diverticulitis Masks Cancer
One of the most complex issues in clinical practice is the diagnostic overlap between diverticulitis and early-stage colon cancer. Because both can produce thickened bowel walls and surrounding inflammation, radiologists may misinterpret a CT scan as diverticulitis when in fact a malignant tumor is present.
In such cases, the inflammation caused by cancer itself may mimic infection, leading to delayed or missed diagnosis. This is especially concerning in older patients or those with no prior history of diverticulitis, where an atypical pattern of pain or bleeding is observed.
Follow-up is essential. Medical guidelines now recommend that patients over 40 who experience an episode of diverticulitis should undergo colonoscopy 6–8 weeks after recovery, especially to rule out hidden malignancies.
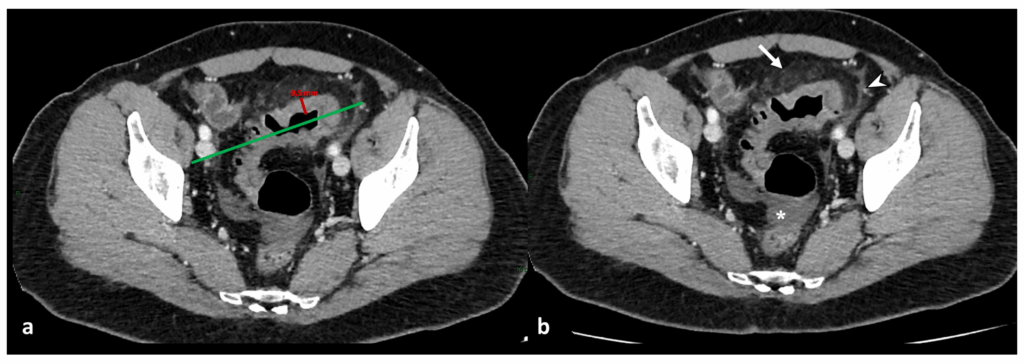
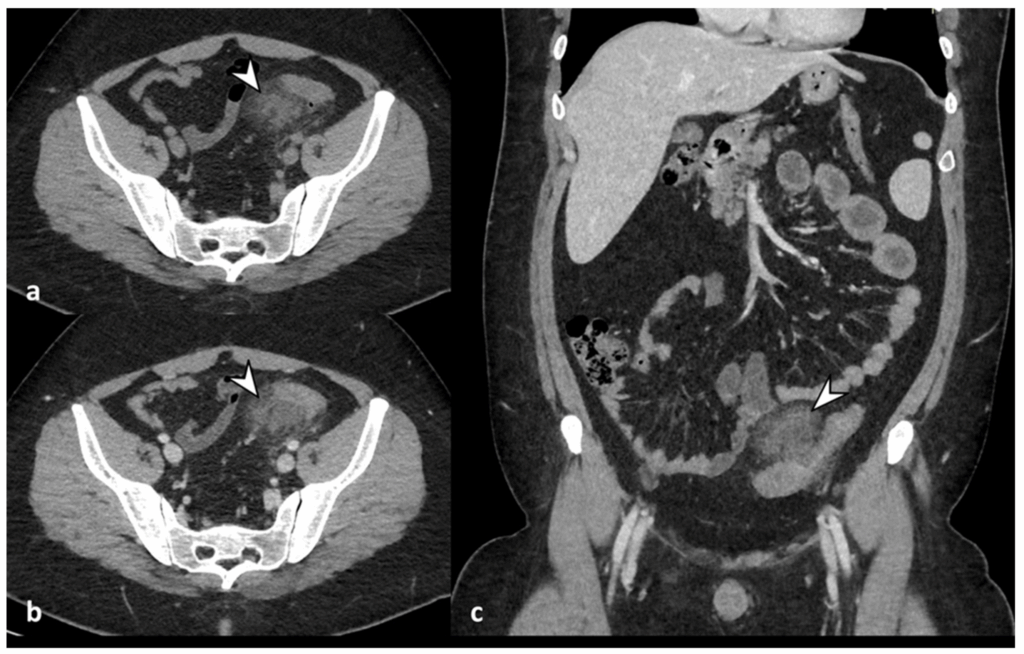
Imaging Tests: What They Can and Can’t Show
A key tool in diagnosing both diverticulitis and colon cancer is the CT scan, particularly with contrast enhancement. CT scans are highly sensitive for identifying acute inflammation, abscesses, fistulas, and even perforations of the bowel wall.
However, while CT is excellent for detecting complications of diverticulitis, its ability to distinguish between benign and malignant masses is limited. That’s why colonoscopy remains the gold standard for visual confirmation and biopsy of abnormal tissue.
| Test Type | Usefulness for Diverticulitis | Usefulness for Colon Cancer | Limitations |
| CT Scan | High | Moderate | Cannot definitively rule out small tumors |
| Colonoscopy | Moderate (if acute resolved) | High | Invasive, requires bowel prep |
| MRI | Low (not first-line) | Occasionally used | Expensive, mostly for rectal cancer |
In clinical settings, it’s common for patients recovering from diverticulitis to ask, “Will a CT scan show colon cancer if I had one during my flare?” The answer is: not reliably. CT may detect mass effect or irregularities, but early tumors may be missed without direct visualization and biopsy.
Risk Factors: Who Is More Vulnerable to Both Conditions
While diverticulitis and colon cancer are separate conditions, they share many overlapping risk factors, particularly those related to lifestyle, age, and genetic predisposition.
Age is the strongest predictor for both. People over the age of 50 have a sharply increased risk of developing both diseases. A low-fiber, high-fat diet, sedentary lifestyle, and obesity contribute to both diverticular disease and neoplastic changes in the colon lining.
Certain inherited conditions also predispose individuals to both complications of diverticulosis and colon malignancies. These include:
| Risk Factor Category | Examples |
| Lifestyle-related | Low fiber intake, smoking, sedentary habits |
| Age-related | Over 50 years old |
| Genetic or familial | Lynch syndrome, familial adenomatous polyposis (FAP) |
| Metabolic conditions | Obesity, type 2 diabetes |
| Chronic inflammation | Longstanding diverticulitis or IBD |
Understanding these risk factors allows clinicians to individualize screening recommendations, especially for patients with a history of recurrent diverticulitis or other bowel disorders.
How Age and Diet Impact Both Conditions
Both colon cancer and diverticulitis are profoundly affected by diet and aging physiology. As we age, colonic motility slows, and the connective tissue of the colon wall weakens, predisposing to the formation of diverticula and the development of slow-growing polyps that may become cancerous.
Diet plays a dual role: insufficient fiber leads to harder stools and increased intraluminal pressure, while diets high in red and processed meats are associated with higher rates of colon cancer.
Interestingly, many of the early symptoms of colon cancer — such as irregular bowel movements, occasional bleeding, and bloating — are often mistaken for dietary upset or a minor diverticular flare-up. This is why it’s critical to know what subtle signs may signal something more serious.
Preventive Screening After Diverticulitis
After an acute episode of diverticulitis, especially if it’s the first, many patients assume recovery is the final step. However, medical guidelines now urge routine colonoscopy 6–8 weeks post-recovery to rule out hidden colorectal abnormalities.
This screening is not just precautionary. Studies show that in about 1 in 10 cases, what appears to be uncomplicated diverticulitis may mask a tumor, particularly in the sigmoid colon. A colonoscopy can visually inspect the mucosa, biopsy suspicious lesions, and assess for polyp growth.
Failure to follow up with appropriate screening may result in delayed diagnosis of colon cancer, a potentially curable condition in early stages. For high-risk individuals, repeat colonoscopies may be advised at shorter intervals.
| Patient History | Colonoscopy Recommendation |
| First episode of diverticulitis | Within 6–8 weeks of recovery |
| Recurrent diverticulitis | Every 3–5 years, depending on severity |
| Family history of colon cancer | Earlier and more frequent screening |
| Abnormal imaging findings | Immediate follow-up via colonoscopy |
Long-Term Outlook: Managing Risk After Recovery
Once acute inflammation subsides, the next phase is long-term management. Patients who’ve had diverticulitis are at higher risk for recurrent episodes, and they may also carry a slightly increased risk of concurrent or future colon cancer, especially if other risk factors are present.
Lifestyle interventions are central to both recurrence prevention and colon health. These include adopting a fiber-rich diet, increasing physical activity, and maintaining a healthy weight.
More aggressive strategies may be needed for patients with chronic or complicated diverticulitis, such as those who experience strictures, abscesses, or fistulas. In some cases, elective surgery is performed to remove the affected bowel segment.
Medical follow-up typically includes:
- Monitoring for return of symptoms
- Periodic imaging in complex cases
- Colonoscopy based on personalized risk
- Dietary counseling and GI referral if needed
In patients over 60, managing diverticulitis becomes part of broader efforts to reduce overall colorectal cancer risk, especially with age-related vulnerability.
Role of Colonoscopy in Both Conditions
Colonoscopy is the most definitive tool for diagnosing both diverticular disease and colon cancer. While CT scans are useful for acute inflammation, only colonoscopy allows direct visualization, polyp removal, and biopsy — all crucial in cancer prevention and early detection.
For patients with diverticulitis, the scope may reveal:
- Areas of previous inflammation
- Presence of strictures or fistulas
- Polyps that may require removal
- Suspicious lesions suggesting malignancy
Colonoscopy is typically deferred until acute inflammation resolves, as introducing a scope during active diverticulitis increases the risk of perforation and poor visibility.
| Colonoscopy Purpose | In Diverticulitis | In Colon Cancer Screening |
| Visual exam | Healed areas, diverticular pouches | Polyps, tumors, mucosal changes |
| Biopsy | Of abnormal healing tissue if suspicious | Of any mass or polyp |
| Preventive role | Detects concurrent neoplasms | Removes pre-cancerous growths |
| Timing recommendation | 6–8 weeks post-recovery | Based on age or family history |
Misdiagnoses: How Often Diverticulitis Hides Tumors
One of the most alarming clinical realities is that colonic adenocarcinomas are sometimes misdiagnosed as diverticulitis during initial imaging. This is not a reflection of poor care — rather, it reflects the biologic and radiologic similarity between these two conditions.
Tumors can cause focal inflammation, bowel wall thickening, and even local abscesses — all features typical of diverticulitis on CT. Because of this, studies have shown that in 5–10% of cases, patients initially treated for diverticulitis are later diagnosed with colon cancer during follow-up.
Such misdiagnoses highlight the importance of not dismissing an acute flare as merely benign. Especially in older adults or those with atypical presentation (such as right-sided pain, systemic symptoms, or rectal bleeding), physicians are increasingly urged to maintain a high index of suspicion.
Follow-up colonoscopy and repeat imaging, when indicated, are not optional — they are lifesaving.
Diet, Fiber, and Lifestyle in Prevention
One of the most powerful tools for both preventing diverticulitis flare-ups and reducing the risk of colon cancer is diet. A fiber-rich diet helps normalize bowel movements, reduce colonic pressure, and prevent the formation of new diverticula. At the same time, it is associated with a significantly lower risk of colon cancer.
In contrast, diets high in red meats, saturated fats, and processed foods are linked to a higher incidence of both diverticular disease complications and colorectal tumors. Hydration is another critical factor: insufficient fluid intake can worsen constipation and lead to harder stool, aggravating symptoms.
Beyond diet, regular physical activity, maintaining a healthy weight, and avoiding tobacco and excessive alcohol further reduce risks.
| Lifestyle Element | Impact on Diverticulitis | Impact on Colon Cancer |
| High-fiber intake | Reduces flares and constipation | Decreases cancer risk |
| Physical activity | Improves digestion and motility | Lowers inflammation and cancer likelihood |
| Smoking cessation | Reduces vascular complications | Strongly decreases cancer incidence |
| Alcohol moderation | Prevents GI irritation | Lowers risk of rectal cancer |
A dietary shift isn’t just therapeutic — it’s preventive medicine for your colon.
Understanding Your Pathology Report
After a colonoscopy or surgical intervention, you may receive a pathology report — a document summarizing the microscopic findings of any tissue samples taken. This report is critical for determining whether a patient has diverticulosis, inflammation, precancerous polyps, or cancer itself.
The pathology report might mention:
- Hyperplastic polyps: Generally benign
- Adenomatous polyps: Pre-cancerous, requiring removal and follow-up
- Inflammation: Indicative of active or resolving diverticulitis
- Dysplasia: Abnormal cell growth that may precede cancer
- Invasive adenocarcinoma: A diagnosis of colon cancer
Reading this report can be intimidating, but your gastroenterologist will walk you through each term. If cancer is found, staging and grading will follow, determining the appropriate treatment plan.
Diverticulitis vs. Colon Cancer in Clinical Records
While symptoms and imaging can overlap, careful medical review and testing help distinguish diverticulitis from colon cancer. Here is a comparison table often used in clinical education:
| Feature | Diverticulitis | Colon Cancer |
| Onset | Sudden, often with fever | Gradual, often silent in early stages |
| Pain location | Lower left abdomen (sigmoid colon) | Can vary — right, left, or generalized |
| Response to antibiotics | Rapid improvement | Little to no improvement |
| Stool characteristics | May have bright red blood | Blood mixed in, dark or tar-like |
| Scope/colonoscopy findings | Pouches (diverticula), redness | Polyps, mass lesions, ulcers |
This table is used to guide decisions on further testing or surgery, especially when imaging is inconclusive.
Summary: What to Do If You’re Diagnosed with Either
Being diagnosed with diverticulitis or colon cancer can feel overwhelming. But understanding what each condition means — and how it can be managed — provides a powerful sense of control.
If you’re diagnosed with diverticulitis, focus on:
- Completing antibiotic therapy
- Dietary adjustments for healing and prevention
- Following up with a colonoscopy
- Monitoring for signs of complication or recurrence
If you’re diagnosed with colon cancer, early detection offers excellent survival outcomes. Your care will involve:
- Staging (via scans and pathology)
- Surgical consultation
- Oncology review (for chemotherapy or radiation)
- Nutritional and psychological support
Importantly, if you’ve had diverticulitis, it doesn’t mean you’re destined to develop cancer — but it does mean you should be proactive with screening and self-monitoring.
15+ Frequently Asked Questions (FAQ)
1. Can stress trigger diverticulitis or increase cancer risk?
Chronic stress does not directly cause diverticulitis or colon cancer, but it can contribute to gastrointestinal dysfunction. Stress alters gut motility and may weaken the immune response, which could increase inflammation in existing diverticula. Additionally, stress can lead to unhealthy lifestyle habits like poor diet or smoking, indirectly elevating cancer risk.
2. Is there a genetic link between diverticulitis and colon cancer?
While diverticulitis itself is not typically inherited, colon cancer has a strong genetic component. If you have a family history of colorectal cancer or certain genetic syndromes like Lynch syndrome, your risk increases. It’s advisable to undergo genetic counseling if multiple relatives have been diagnosed with colon cancer.
3. Can probiotics help prevent diverticulitis flare-ups?
Some studies suggest that certain probiotic strains may reduce the frequency or severity of diverticulitis symptoms by improving gut flora balance. However, evidence is still emerging, and they should not replace fiber intake or prescribed medications.
4. What type of pain differentiates diverticulitis from colon cancer?
Diverticulitis usually causes sharp, localized pain in the lower left abdomen that worsens with movement or pressure. Colon cancer pain is more likely to be dull, crampy, and persistent, sometimes radiating or associated with bloating or changes in stool.
5. Are CT scans enough to rule out colon cancer after diverticulitis?
CT scans are highly useful in identifying inflammation and complications like abscesses or perforations, but they cannot fully rule out colon cancer. A follow-up colonoscopy is still considered the gold standard for definitive evaluation.
6. How long should I wait to get a colonoscopy after diverticulitis?
Most experts recommend waiting 6–8 weeks after recovery from an acute episode before having a colonoscopy. This allows inflammation to subside, reducing the risk of perforation and improving visibility.
7. Can recurrent diverticulitis lead to colon cancer over time?
There is no direct progression from diverticulitis to cancer, but recurrent inflammation may cause changes in the colon lining that can complicate diagnostics. It also increases the chance of uncovering hidden malignancy through frequent surveillance.
8. What are the warning signs that diverticulitis may be masking cancer?
Persistent or worsening symptoms despite treatment, weight loss, anemia, or blood in the stool could suggest an underlying cancer. These symptoms require urgent follow-up and colonoscopy.
9. Does smoking affect both conditions equally?
Yes, smoking is associated with a higher risk of both diverticular complications and colon cancer. Tobacco impairs vascular health, disrupts normal bowel function, and introduces carcinogens into the digestive system.
10. Is it safe to eat seeds and nuts with diverticulitis?
Old guidelines advised against seeds and nuts, fearing they could lodge in diverticula. Recent studies have found no evidence that these foods increase risk — and in fact, they may be protective due to their fiber and nutrient content.
11. How does obesity influence these conditions?
Obesity increases pressure on the colon, contributing to diverticula formation. It also promotes chronic inflammation and insulin resistance, both of which are risk factors for developing colon cancer.
12. Can women experience symptoms differently than men?
Yes, women are more likely to report bloating and generalized abdominal discomfort, especially after menopause. In colon cancer, right-sided tumors (more common in women) may present with anemia and fatigue rather than overt GI symptoms.
13. Are there differences between Western and Eastern diets regarding these diseases?
Western diets, high in red meat, low in fiber, and high in fat, are associated with a greater risk of both conditions. In contrast, diets in many Eastern cultures include plant-based foods, whole grains, and fermented products, which offer protective effects.
14. Can I get both conditions at once?
Yes, some individuals may have diverticulitis and undiagnosed colon cancer simultaneously. This is why medical guidelines recommend a thorough workup after a diverticulitis episode, especially in older adults or those with unexplained symptoms.
15. How often should I be screened for colon cancer after diverticulitis?
If your colonoscopy after diverticulitis is clear, standard screening intervals apply: every 10 years for low-risk individuals, and more frequently if polyps were found or if there’s a family history. Your doctor will tailor a plan based on your full risk profile.