Disease X: Preparing for the Unknown
- Part One — Introduction (Narrative Rewrite)
- Part Two — Potential Origins
- Part Three — Surveillance and Detection
- Part Four — Preparedness Strategies
- Part Five — Ethical and Social Considerations
- Part Six — Recent Developments (2025–2026)
- FAQ: Disease X — The Questions We Keep Asking
- Seven — Conclusion: What It Really Means to Be Ready
Introduction
In a quiet corner of the World Health Organization’s strategic planning documents sits a name that doesn’t belong to any known virus. It isn’t Ebola. It isn’t influenza. It isn’t COVID-19. It’s simply called Disease X—an ominous placeholder for a future pandemic that hasn’t yet arrived but almost certainly will.
At first glance, the name sounds like something plucked from science fiction. But there’s nothing fictional about the thinking behind it. Disease X isn’t meant to frighten. It’s meant to focus. It stands for the unknown—a virus or pathogen that will emerge from somewhere we weren’t expecting, at a time we aren’t prepared for, and move faster than we think possible.
And we know this isn’t just speculation. History is full of once-unknown diseases that arrived quietly, then exploded across the world. SARS in 2003. H1N1 in 2009. Ebola’s West African outbreak in 2014. And, of course, COVID-19, which reshaped the world with stunning speed and brutality. None of these were predicted in advance, and each caught systems off guard. Disease X is a way of saying: Next time, let’s not be surprised.
In fact, the rationale behind Disease X echoes closely with how virologists have begun treating silent threats like HKU5-CoV-2 — viruses not yet in humans, but evolving in real time across bat populations. These pathogens serve as molecular blueprints for the kind of surprise Disease X might be.
But preparing for the unknown? That’s no easy task. How do you build vaccines for a virus you haven’t discovered? How do you organize healthcare systems for an outbreak that doesn’t yet exist? It’s like trying to solve a puzzle without knowing what image you’re assembling. And yet, there are things we can do. Technologies that let us respond faster. Infrastructure that can flex and scale. Systems that can spot strange patterns before they become catastrophic.
Most importantly, there’s a mindset we need to adopt. One that treats preparedness not as a luxury, but as a moral obligation. Because Disease X isn’t just a medical concern—it’s a human one. It affects families, communities, economies. It transcends borders and ideologies. And it forces us to ask difficult questions: Are our institutions nimble enough? Is our science fast enough? Is our communication clear enough?
If the past few years have taught us anything, it’s this: pandemics don’t reward optimism. They reward readiness.
And so, the story of Disease X begins not with a specific microbe, but with a choice. A choice to take the unknown seriously. To study the systems that failed. To invest in the ones that worked. And above all, to remember that the next crisis won’t wait until we’re comfortable again.
Potential Origins
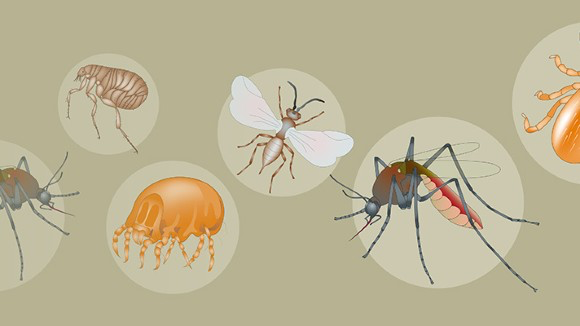
To understand how Disease X might emerge, we have to begin in the places we usually don’t think about—dense forests, live animal markets, factory farms, or even the carefully controlled environment of a high-security laboratory. It’s in these quiet, often overlooked corners of the world where something small—something invisible—could quietly make its leap into human life.
Most likely, it will start with nature. But nature doesn’t act alone. It reacts to pressure — ecological disruption, urban expansion, global travel. That’s why viruses that once felt local can now circle the world in weeks. It’s why pathogens like Oropouche Fever are now expanding their range, urbanizing, and pressing against new borders. Disease X could follow the same trajectory: quiet at first, then suddenly everywhere.

We’ve seen it before. A virus that once lived in bats begins to circulate in another animal, perhaps pigs or civets or monkeys. One day, that animal comes into contact with a human—maybe through hunting, trade, deforestation, or agriculture—and the virus crosses over. That process is called zoonotic spillover, and it’s how many of our most dangerous diseases began.
HIV made the leap from primates. SARS was traced back to civet cats. Ebola is suspected to have spilled over from bats. COVID-19? Still debated, but it fits the pattern: animal, human, global crisis. When we disturb ecosystems—by cutting down forests, trafficking wildlife, or crowding animals into high-stress industrial farming systems—we don’t just disrupt the environment. We create perfect conditions for viruses to jump species.
But nature isn’t the only suspect.
Some believe that Disease X could emerge from inside a laboratory. Not as a weapon, necessarily—but as an accident. The history of science is full of breathtaking discoveries—and the occasional terrifying mistake. Influenza strains have leaked before. SARS has too. Most were caught early. None spiraled into a pandemic. But what if one had?
The more labs work on high-risk pathogens—especially in the absence of clear international oversight—the higher the chance of an accidental release. And if you think that sounds too far-fetched, remember that the closer science gets to mastering viral behavior, the more fragile the line between research and risk becomes.
And then, beyond accidents or animals, there’s a darker possibility: deliberate intent. Bioterrorism.
It sounds cinematic, and in some ways it is. But in the real world, the tools to engineer or enhance a virus are increasingly accessible. You don’t need a nation-state anymore—just knowledge, funding, and the wrong kind of ambition. Whether it’s modifying a known virus or creating something entirely new, the technology exists. The threat is real.
So what does that leave us with?
Nature. Negligence. Malice. Disease X could come from any of these. Maybe even from all three at once, in ways we haven’t yet imagined. That’s why preparedness doesn’t mean betting on a single theory—it means designing systems that are ready for complexity. For ambiguity. For surprise.
Just months before the first COVID-19 cases appeared, health experts ran a simulation called Event 201. They imagined a fictional coronavirus pandemic that spread rapidly across the globe. It was an eerie, almost prophetic exercise—not because it predicted the exact virus, but because it proved that the idea wasn’t so far off.
Disease X is built from that same unsettling truth: that the next global outbreak might not emerge clearly or cleanly. It could arrive in pieces. In signals. In silences.
And when it does, the world will want to know: were we watching closely enough?
Surveillance and Detection
If Disease X is out there—lurking in the lungs of a wild animal, or mutating quietly in a crowded slum, or drifting unseen through a population—then the first and most urgent task is simply this: to notice.
But how do you recognize a threat that doesn’t have a name?
That’s the challenge of surveillance. And not the dystopian kind that imagines cameras on every corner. This is a different kind of vigilance. A kind that requires microscopes, field notebooks, wastewater samples, digital algorithms, and—perhaps most importantly—an open mind. Because the first sign of Disease X might not look like much. A strange cough in an ER. A small uptick in fever cases in a rural clinic. A viral sequence that doesn’t quite match anything known.
Surveillance, in this context, is a kind of global listening. A network of laboratories, hospitals, public health agencies, and researchers quietly tracking patterns in real time. Looking for the moment when the expected becomes weird. When the seasonal flu doesn’t act like seasonal flu. When a virus shows up in a place it shouldn’t. When animal deaths signal something more than an ecological blip.
And yet, this system is far from perfect.
In some countries, detection happens at the genomic level—labs capable of sequencing entire viral genomes in a day. In others, disease reporting still relies on handwritten charts and fax machines. There are gaps—gaping ones. Whole regions where data is sparse, where outbreaks can smolder for weeks before the rest of the world takes notice. Pathogens love those blind spots.
Still, progress is being made. Genomic sequencing is faster and cheaper than ever. AI models are now being trained to scan global news, social media, even Google search trends, looking for linguistic fingerprints of disease. There are even early experiments in using air sampling and ambient biosensors to detect viral particles before a single case is diagnosed.
But surveillance is only half the battle. The other half? Response.
History shows us how fragile that handoff can be. In the early weeks of COVID-19, signals were picked up—labs knew something was wrong. But the systems weren’t fast or decisive enough to act. Bureaucracy slowed the alarms. Fear of economic or political fallout muffled early warnings. The world had the information. It just didn’t listen fast enough.
To prepare for Disease X, we need more than clever machines and better data. We need a new kind of reflex—a readiness to believe the early signs, to mobilize when the smoke first rises, not when the fire is already spreading.

Imagine a world with a true global detection system: health workers equipped with rapid diagnostics, communities trained to report anomalies, real-time data flowing into coordinated hubs. A world where a fever in one country becomes a concern for every country—not in panic, but in partnership.
Because surveillance isn’t just about catching something dangerous. It’s about making sure we’re not caught by surprise.
And in the end, Disease X won’t wait for us to agree it’s real. By the time we’re certain, it may already be too late.
Preparedness Strategies
Preparing for something you can’t name, can’t see, and don’t fully understand might sound like a losing battle. How do you defend against a threat that hasn’t arrived yet? How do you build defenses when you don’t even know where the attack will come from?
And yet—that’s exactly what preparedness demands.
We’re not starting from zero. If the world has learned anything from recent history, it’s that pandemics are not isolated events. They are systemic shocks. They tear through healthcare systems, governments, supply chains, families. And if our defenses aren’t already in place when the next shock hits, it won’t matter how much we want to respond. It’ll already be too late.
So what does real preparedness look like?
Let’s start with vaccines. The old model—designing a vaccine from scratch for each new disease—simply isn’t fast enough anymore. In a world where a virus can cross continents in hours, we need vaccine platforms that are as agile as the pathogens they target.
That’s where technologies like mRNA come in. Instead of building a vaccine from the ground up, mRNA platforms allow scientists to drop in the genetic blueprint of a new virus and begin production almost immediately. It’s not magic—but it’s close. The first COVID-19 mRNA vaccines were designed within days of sequencing the virus. Now, the goal is to make that kind of speed the norm.
But a formula isn’t enough. The best vaccine in the world won’t help if there’s no way to manufacture it, store it, ship it, and administer it widely and fairly. Preparedness also means investing in distribution infrastructure: regional factories, cold chain logistics, local clinics, trained personnel. It means making sure that a breakthrough in one part of the world doesn’t arrive too late for the rest.
And here’s where things often break down—equity.
In 2021, while wealthier nations were debating booster shots, vast regions of the world were still struggling to access first doses. The virus exploited that inequality, mutating into more dangerous variants in places where it could spread unchecked. Disease X won’t behave any differently. If we don’t prepare globally, we’re not really prepared at all.
Preparedness also extends beyond vaccines. It’s about surge capacity in hospitals. Rapid diagnostics that can identify new pathogens at the point of care. Protective equipment stockpiles that don’t expire in warehouses. And crucially, it’s about training—not just for doctors, but for frontline workers, teachers, local officials. People who will be the first to respond when something strange starts to happen.
And let’s not forget the social dimension.
Public health lives and dies on trust. If communities don’t believe the information they’re receiving—or don’t trust the people delivering it—preparedness falls apart. That means we can’t just build supply chains and laboratories. We have to build relationships. We have to get better at communicating uncertainty, admitting what we don’t know yet, and including communities in the conversation—not just when things go wrong, but all the time.
Some of this work is already happening. Public-private partnerships are creating pandemic response funds. Global alliances are developing “prototype vaccines” for virus families we haven’t seen yet. AI is being trained to run global simulations, testing our weaknesses before nature does. These are promising steps—but they need to be sustained.
Because there’s a pattern: we react strongly after a crisis, then grow complacent. The memory of suffering fades. Budgets are cut. Preparedness becomes a line item, not a mission.
Disease X will take advantage of that cycle if we let it.
So we have a choice: wait, and scramble again. Or plan—not for one scenario, but for any scenario. Not with fear, but with urgency.
Preparedness isn’t glamorous. It doesn’t make headlines until it fails. But when it works, you don’t even notice it. And that, in the case of Disease X, might be the most powerful defense of all.
Ethical and Social Considerations
It’s one thing to talk about science. It’s another to talk about people.
Pandemics don’t just challenge our immune systems—they test our values, our trust, and the fragile bonds that hold societies together. When Disease X arrives, it won’t just confront hospitals and laboratories. It will confront democracy, culture, and belief. And how we respond won’t be shaped by virology alone. It will be shaped by ethics.
One of the first dilemmas? Freedom versus safety. It happens every time.
The moment a dangerous pathogen begins to spread, public health authorities reach for tools that have saved lives in the past: lockdowns, contact tracing, quarantine. These are powerful interventions—but they also carry heavy social costs. Shutting down cities might slow transmission, but it also shutters livelihoods. Mandating vaccines might protect communities, but it can provoke backlash. When governments act quickly and forcefully, they’re often accused of overreach. When they act too slowly, they’re blamed for negligence.
The truth is, there’s no perfect balance. But we must still try to find one.
And part of that balance means looking at who pays the price for protection. A stay-at-home order may be manageable for a salaried office worker. For a gig worker, a caregiver, or someone living in a crowded home, it might mean losing income, independence, even safety. Policies that appear neutral on paper often land hardest on the most vulnerable. If we want equitable outcomes, we must design equitable strategies—from the start.
Then there’s the invisible virus behind every pandemic: misinformation.
In an outbreak, rumors move faster than pathogens. One poorly edited video, one misleading headline, one influential skeptic—and suddenly, truth is drowning in noise. During COVID-19, the World Health Organization began using a new word: infodemic. A tidal wave of false or misleading information that spreads confusion, fuels division, and undermines public trust.
Preparedness, then, must include more than logistics and supplies. It must include a communication strategy that earns trust before it needs to. That means transparency—being honest even when we’re unsure. It means listening—not just broadcasting messages, but responding to the fears and questions people actually have. And it means engaging with communities long before the first cases appear.
There’s also a darker pattern we can’t ignore: scapegoating. Every major outbreak has been accompanied by fear-driven discrimination. During the early HIV crisis, entire communities were demonized. During COVID-19, hate crimes surged against Asian populations. When people are afraid, they look for someone to blame—and that can be deadly.
If Disease X emerges, we’ll have to choose our words carefully. We’ll have to protect privacy even as we track contacts. We’ll have to fight the urge to point fingers across borders or within them. Otherwise, we risk turning a health crisis into a social one.
And what if people simply refuse to cooperate? What if they ignore health orders, reject vaccines, dismiss expert advice?
That’s not just a matter of ignorance. Often, it’s a reaction to being excluded, patronized, or burned by systems that didn’t listen before. If people don’t trust authorities, it’s not enough to scold them or call them “anti-science.” We have to earn back that trust. That starts with inclusion—inviting local voices into national plans, treating communities not as obstacles but as partners.
Ethics, in the context of Disease X, is not an afterthought. It’s the scaffolding that holds everything else up.
Because the pandemic response we build will shape more than just the outcome—it will shape what kind of society we become.
Recent Developments (2025–2026)
Disease X hasn’t arrived. Not yet. But signs are gathering.
A mysterious tick-borne virus in Europe. A lab incident involving H5N1. A disinformation wave triggered by a fabricated outbreak video. Each event feels unrelated, but they all point in the same direction: the margin for error is shrinking.
At the same time, the tools are improving. Senegal’s genomic network. South Korea’s AI outbreak sensors. Bangladesh’s investment in mRNA capacity. These may not be headline news — but they are the scaffolding of future response.
And in the background, researchers continue to develop prototype vaccines for virus families we’ve never seen. They’re mapping genomes. Running simulations. Preparing for the jump. It’s not glamorous work. But it’s the only kind that matters when the world is quiet.
Just like the quiet we had before COVID-19. Or SARS. Or H5N9.
It’s easy to talk about preparedness as a future goal—something distant, theoretical, always just over the horizon. But in truth, the story of Disease X has already begun. Not as a single outbreak, not yet, but as a series of quiet warnings and unfinished experiments. A pattern of close calls. A glimpse of what might come.
Over the past two years, the world has taken some meaningful steps forward.
The most visible change has been the rise in global cooperation—at least, in principle. The World Health Organization has pushed hard for its new Pandemic Accord, an international framework that aims to standardize how countries report outbreaks, share resources, and respond to threats. It’s a vision of solidarity: one planet, one plan.
But progress has been bumpy. Some nations are on board. Others worry the agreement threatens their sovereignty or imposes costs they can’t afford. It’s one thing to sign a treaty. It’s another to live by it when the next crisis tests your borders.
Meanwhile, vaccine manufacturing has become more distributed, especially across the Global South. Countries like Rwanda and Bangladesh are now investing in mRNA production capacity—making it more likely that when Disease X appears, they won’t be at the back of the line waiting for Western shipments. These are quiet revolutions in health independence, and they matter.
In terms of surveillance, real-time dashboards are becoming the norm in many places. In South Korea, AI-integrated systems track outbreaks across airports, hospitals, and even wastewater in real time. Senegal has launched a regional genomics lab network that can identify new viral strains within 48 hours. These tools aren’t universal yet—but they’re spreading.
Still, not all the news is encouraging.
In mid-2025, a tick-borne virus emerged in Central Europe with genetic markers unfamiliar to researchers. It wasn’t highly transmissible between humans—but it was just transmissible enough to set off alarm bells. The virus never went global. But it exposed lingering weaknesses in cross-border data sharing, especially between animal health and human health agencies. A familiar crack in the system.
Then there was the lab incident—a modified H5N1 strain, improperly handled in a secure facility in East Asia. The virus didn’t escape the building. There were no infections. But it reignited the long-simmering debate around gain-of-functionresearch and underscored how easily accidents could turn into disasters.
And in early 2026, something different: not a virus, but a deepfake.
A video claiming to show a government coverup of a fictional “Disease X” outbreak went viral—millions of views within two days. It was convincing enough that even some health professionals were unsure. Panic spread. Public trust wavered. By the time officials clarified the hoax, the damage was done. It was a test run for the next infodemic—and we failed it.
All of these events point to the same truth: we are not guessing anymore.
Disease X isn’t a hypothetical exercise in a think tank. It’s already shaping policy, budget allocations, international diplomacy. It’s being discussed in Cabinet meetings, simulated in military strategy games, anticipated by researchers designing “prototype vaccines” for entire viral families.
The world has moved. But has it moved fast enough?
We’re building better tools, yes. And in some places, we’re building better systems. But too often, these efforts remain uneven, reactive, fragile. We surge during crisis. Then we slip into complacency. Funding dries up. Headlines move on.
Disease X is watching that rhythm. And it’s learning from it.
So the real question isn’t “Have we done something?” Of course we have. The real question is: Have we done enough to make a difference before the next outbreak begins?
Because readiness, like a parachute, only works if it’s packed before you fall.
FAQ: Disease X — The Questions We Keep Asking
What exactly is Disease X?
Disease X is a placeholder term used by the World Health Organization to represent a hypothetical future infectious disease with pandemic potential. It’s not a specific pathogen—it’s a warning label for the unknown.
Why prepare for something that doesn’t exist?
Because the unknown is inevitable. History shows us that the next outbreak likely won’t look like the last. Disease X is a concept that reminds us to expect surprises—and build systems that can adapt.
Where could Disease X come from?
Potential sources include zoonotic spillover from animals, laboratory accidents, and bioterrorism. Each origin route has precedent—and each presents unique challenges.
Can a virus really jump from animals to humans?
Absolutely. HIV, SARS, Ebola, and COVID-19 all originated this way. Increased human-wildlife contact makes zoonotic spillover more likely.
Should we take lab leaks seriously?
Yes. While rare, lab accidents have occurred. Pathogens don’t care about good intentions—only about opportunities to escape and spread.
Is bioterrorism still a real threat?
Yes. Advances in synthetic biology make it technically possible to engineer or release novel pathogens. It’s not common—but the risk is non-zero.
How do we catch a threat we haven’t seen before?
Through global surveillance systems, genomic sequencing, wastewater testing, AI monitoring, and frontline health data. The key is spotting weirdness before it turns into a wave.
Who’s actually watching for Disease X?
Organizations like WHO, CDC, national health agencies, and academic labs. But surveillance quality varies widely depending on geography and funding.
What kind of vaccines will work for an unknown virus?
Flexible platforms like mRNA and viral vectors can be quickly adapted to new pathogens, making rapid-response vaccines more viable than ever.
What does preparedness really mean?
It means having fast diagnostics, strong supply chains, trained personnel, public trust, and equitable access to care and vaccines—before a crisis begins.
What happens when public health measures clash with personal freedoms?
Tensions arise. Effective responses must balance safety with ethics, and respect individuals while protecting the collective.
How does misinformation affect our ability to respond?
It erodes trust, delays action, and amplifies harm. Fighting misinformation is now a central part of pandemic preparedness.
Have there been any Disease X “close calls” recently?
Yes—several outbreaks, lab incidents, and disinformation surges in 2025–2026 have highlighted gaps in current systems and sparked reforms.
Are we actually learning from past mistakes?
We’re learning—but not consistently. Some nations are innovating; others are falling back into complacency. It’s a mixed but evolving picture.
Conclusion: What It Really Means to Be Ready
Maybe the hardest part of preparing for something like Disease X is that it doesn’t feel real. Not yet. We’re not responding to a crisis—we’re trying to stay ahead of one. And humans aren’t great at that. We’re built to react to things we can see, not abstract risks that sit somewhere in the future.
But we’ve been here before. Not just with COVID-19, but with SARS, H1N1, Ebola. Each time, we were caught off guard in different ways. And each time, once the immediate threat passed, a lot of the urgency faded. That’s the pattern we have to break.
This isn’t about predicting the next virus. We won’t. It’ll be something different—a new host, a new mutation, a new set of circumstances. The point isn’t to get the details right. It’s to build systems that don’t fall apart when something unexpected shows up.
That means having diagnostics that can pick up weird patterns early, even when we don’t know what we’re looking at yet. It means building vaccine platforms that can be adapted quickly—not after six months of scrambling, but in weeks. It means making sure health systems aren’t running at full capacity on a normal day, so they don’t collapse when the pressure comes.
And yeah, it also means talking to the public like adults. Not waiting until things are bad to communicate, and not pretending we have all the answers when we don’t. People can handle uncertainty. What they can’t handle is confusion layered on top of fear.
Some of this is already happening. Some countries are building real-time surveillance systems. mRNA manufacturing is expanding. There’s talk about new global agreements. But it’s uneven. And it’s fragile. Without consistent funding, political will, and public trust, all of it risks being temporary.
The window for acting is open now—because there’s no emergency demanding attention. But that’s also when it’s easiest to do nothing. No headlines, no pressure. Just a quiet opportunity to prepare. Or not.
What we do with that quiet—that’s what matters.