Understanding the Differences Between Vitamin B12 Deficiency and Tongue Cancer
- What Is Vitamin B12 Deficiency?
- What Is Tongue Cancer?
- Early Symptoms: Key Differences in Presentation
- Risk Factors and Underlying Causes
- Diagnostic Pathways: Blood vs. Biopsy
- Prognosis and Disease Trajectory
- Response to Treatment: Speed and Scope
- Potential Complications if Left Untreated
- Visual and Textural Tongue Changes
- Oral and Systemic Pain Profiles
- Misdiagnosis and Self-Medication Pitfalls
- Overlapping Risk Populations and Age Factors
- Nutritional Recovery vs. Oncological Rehabilitation
- Psychological Impact and Patient Perception
- Public Health Messaging and Awareness
- Summary of Core Differences
- FAQ

What Is Vitamin B12 Deficiency?
Vitamin B12 deficiency, also known as cobalamin deficiency, is a medical condition in which the body does not have enough vitamin B12 to support essential physiological functions. This water-soluble vitamin is crucial for red blood cell formation, neurological function, and DNA synthesis. Without sufficient B12, the body cannot produce healthy blood cells or maintain proper nerve communication, leading to systemic consequences.
Deficiency can develop slowly and subtly over months or even years, which often delays diagnosis. It may present with non-specific symptoms such as fatigue, dizziness, mood changes, and pale skin. In more severe cases, neurological symptoms like tingling in the hands and feet or memory problems emerge, indicating progressive nerve damage. Because oral tissues regenerate quickly, the tongue often shows early signs, including redness, inflammation, or a burning sensation — collectively referred to as glossitis.
This condition is frequently reversible if detected early. However, prolonged deficiency may result in irreversible nerve damage, making timely diagnosis and treatment essential.
What Is Tongue Cancer?
Tongue cancer is a malignant condition originating in the squamous cells lining the tongue. It is classified as a type of head and neck cancer and can involve either the anterior two-thirds (oral tongue) or the posterior third (base of tongue, part of oropharyngeal cancer). Most cases are squamous cell carcinoma, which tends to spread locally and, in advanced stages, to lymph nodes and distant organs.
Risk factors for tongue cancer include tobacco use, heavy alcohol consumption, chronic oral irritation, and infection with high-risk strains of human papillomavirus (HPV). It can start as a small, persistent sore or ulcer that fails to heal, or as a red or white patch (erythroplakia or leukoplakia). Over time, patients may experience increasing pain, difficulty speaking, or problems with swallowing.
Unlike nutritional deficiencies, tongue cancer requires aggressive treatment. This often involves surgery, radiation, and chemotherapy, depending on the stage. The prognosis varies — early-stage cancers have high cure rates, while advanced cases like Stage 4 appendix cancer tend to require multimodal therapy and carry a more guarded outlook.
Early Symptoms: Key Differences in Presentation
While both vitamin B12 deficiency and tongue cancer may affect the tongue, their presentations are markedly different in quality, onset, and systemic impact. Glossitis caused by B12 deficiency typically appears as a smooth, swollen, and red tongue, often accompanied by a burning or tingling sensation. The entire oral mucosa may feel sensitive, and patients frequently report taste disturbances or dry mouth. These symptoms tend to fluctuate and may improve with rest, dietary changes, or supplementation.
In contrast, tongue cancer presents as a localized lesion — a non-healing ulcer, lump, or area of induration (firmness) on the tongue. It is usually unilateral and may be painful when touched or when eating spicy foods. As the tumor grows, symptoms such as bleeding, jaw stiffness, or referred ear pain may emerge. Unlike nutritional issues, these lesions persist and gradually worsen despite local care.
The timing of symptom evolution also differs: B12 symptoms develop over weeks to months with waxing and waning intensity, whereas tongue cancer lesions persist continuously and progress unless medically treated.
Risk Factors and Underlying Causes
Vitamin B12 deficiency and tongue cancer originate from completely different physiological disturbances, and understanding these differences helps clinicians target the appropriate diagnostic path.
Vitamin B12 deficiency is most often caused by poor absorption rather than insufficient dietary intake. Conditions such as pernicious anemia (autoimmune destruction of gastric parietal cells), post-gastrectomy status, Crohn’s disease, and chronic use of acid-suppressing medications can all impair B12 absorption in the stomach or small intestine. Dietary deficiency is seen in strict vegans or those with highly restrictive eating patterns.
Tongue cancer, on the other hand, is rooted in cellular mutation due to chronic exposure to carcinogens. Smoking and alcohol act synergistically to increase DNA damage, while HPV-related tongue cancer tends to affect younger individuals without traditional risk factors. Genetics, age, and long-standing oral irritation (e.g., sharp teeth, poorly fitting dentures) may further contribute.
Both conditions can develop insidiously, but one stems from a reversible nutritional imbalance, while the other reflects uncontrolled cellular proliferation requiring immediate oncologic evaluation.
Diagnostic Pathways: Blood vs. Biopsy
The diagnostic approach for vitamin B12 deficiency is predominantly biochemical. Physicians typically order a complete blood count (CBC), which may reveal macrocytic anemia — large red blood cells with low hemoglobin. Serum vitamin B12 levels confirm deficiency, and in ambiguous cases, methylmalonic acid and homocysteine levels may be tested, as they rise before serum B12 drops. If absorption issues are suspected, additional tests like anti-intrinsic factor antibodies or Schilling tests (rarely used today) may be needed.
Diagnosis of tongue cancer follows a different pathway. The primary method is physical examination of the oral cavity, often during routine dental or ENT check-ups. Any suspicious lesion that does not heal within two weeks warrants a biopsy. Imaging techniques such as MRI, CT, or PET scans are used to assess tumor size, local invasion, and spread to lymph nodes or distant sites.
In short, vitamin B12 deficiency is confirmed with lab tests, while tongue cancer requires tissue sampling and imaging to stage the disease. The diagnostic urgency for tongue cancer is significantly higher due to its malignant potential.
Prognosis and Disease Trajectory
The prognosis of vitamin B12 deficiency is generally excellent with prompt diagnosis and treatment. Neurological symptoms often improve over weeks to months, and hematologic abnormalities usually normalize within 6–8 weeks of therapy. However, delayed intervention — particularly in elderly patients — may lead to irreversible neuropathy.
Tongue cancer prognosis depends on the stage at diagnosis, tumor size, and lymph node involvement. Early-stage disease has a favorable outcome, often exceeding 80% five-year survival. However, advanced cases with regional or distant metastasis carry a much poorer prognosis, sometimes below 50%, even with aggressive treatment. The tumor’s grade, location (oral vs. base of tongue), and HPV status also influence survival.
Just like in breast cancer with skin mets, where visible lesions reflect systemic disease and prompt complex decision-making, visible tongue lesions should never be dismissed as benign. Their presence often signals the need for multidisciplinary cancer management and a structured treatment timeline.

Response to Treatment: Speed and Scope
Vitamin B12 deficiency responds rapidly to treatment in most cases. Injections of cyanocobalamin (usually 1000 mcg intramuscularly) are given weekly or biweekly initially, followed by maintenance therapy. Oral supplementation may suffice for dietary-related deficiencies. Symptoms such as fatigue and glossitis often improve within days, and neurological improvement typically begins within weeks.
In contrast, tongue cancer requires more invasive and time-intensive management. Localized tumors may be surgically excised, but patients often require radiation therapy and chemotherapy, particularly for larger or node-positive lesions. Treatment may be curative but comes with potential side effects: changes in taste, difficulty swallowing, speech alterations, and dry mouth.
The quick response to vitamin B12 therapy provides diagnostic confirmation in uncertain cases. Tongue cancer, however, demands a long-term treatment plan with clear milestones for surgery, radiation, and follow-up.
Potential Complications if Left Untreated
Untreated vitamin B12 deficiency can lead to irreversible neurological damage, including peripheral neuropathy, ataxia, and even dementia-like symptoms. Severe deficiency may also result in megaloblastic anemia, glossitis, and increased risk of cardiovascular complications due to elevated homocysteine.
Untreated tongue cancer poses a more immediate threat to life. As tumors enlarge, they may infiltrate the floor of the mouth, jawbone, or lymph nodes. Patients experience progressive pain, feeding difficulty, airway compromise, and often visible disfigurement. At later stages, metastasis to the lungs or other organs becomes likely.
These complications illustrate how vastly different the clinical urgency is between the two. While B12 deficiency is serious but largely reversible, tongue cancer becomes life-threatening if not promptly addressed.
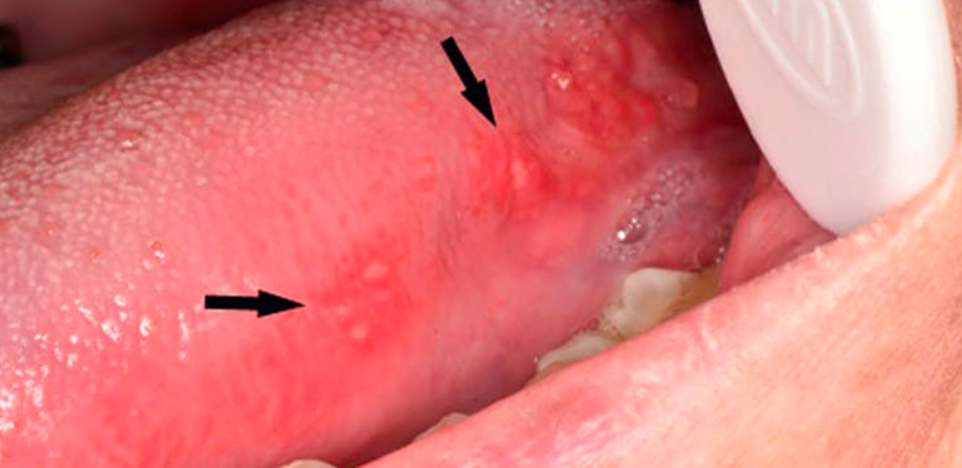
Visual and Textural Tongue Changes
One of the most helpful distinguishing features between vitamin B12 deficiency and tongue cancer lies in the visual appearance and texture of the tongue. In B12 deficiency, the tongue often becomes smooth, swollen, and erythematous — known as “atrophic glossitis.” The papillae (small bumps on the surface of the tongue) may disappear, leading to a shiny or “bald” appearance. Patients frequently complain of burning sensations or increased sensitivity to spicy foods.
In contrast, tongue cancer typically appears as a localized abnormality — a single ulcer, red or white patch, or a firm mass. The lesion may have raised or irregular borders, and over time it may become ulcerated, hardened, or bleed. Surrounding tissues may remain unaffected, and unlike B12-related glossitis, the lesion does not resolve or improve without intervention.
This visual distinction is critical in practice: diffuse smoothness suggests nutritional deficiency, while a focal mass, ulcer, or non-healing sore strongly suggests malignancy.

Oral and Systemic Pain Profiles
Pain is another diagnostic differentiator. In vitamin B12 deficiency, pain is usually described as a burning or tingling sensation on the tongue or within the mouth. This discomfort is often diffuse, mild to moderate in intensity, and may worsen with certain foods or mouthwashes. It is more neuropathic in nature — related to nerve irritation rather than physical damage to tissue.
In tongue cancer, pain tends to be localized and often sharp or persistent. It may worsen while chewing, speaking, or drinking acidic liquids. Patients may also experience referred pain to the ear or jaw, and in advanced stages, pain becomes constant, affecting sleep and eating.
Importantly, pain from tongue cancer often progresses steadily, whereas B12-related discomfort may fluctuate depending on dietary intake or general health status.
Misdiagnosis and Self-Medication Pitfalls
Because early symptoms of both conditions can be vague, misdiagnosis is common. Many patients with B12 deficiency are initially treated for oral thrush or iron-deficiency anemia, especially if oral changes dominate the clinical picture. Similarly, persistent ulcers on the tongue are sometimes mistaken for canker sores, traumatic bites, or geographic tongue — delaying proper cancer evaluation.
Over-the-counter remedies like vitamin supplements, mouth rinses, or antifungals may temporarily soothe symptoms but can mask the progression of underlying disease. Patients may also delay seeking help, especially if they associate oral changes with recent dental work, stress, or nutritional lapses.
This diagnostic delay is particularly dangerous in malignancies. Just as in nasal cancer in dogs, where non-specific signs like sneezing or nasal discharge can obscure a serious underlying condition, oral lesions that persist beyond two weeks — especially with risk factors like smoking — should prompt immediate referral.
Overlapping Risk Populations and Age Factors
Both vitamin B12 deficiency and tongue cancer are more prevalent in older adults, though for different reasons. B12 absorption tends to decline with age due to reduced gastric acid production, and older individuals are more likely to be on medications that impair absorption, such as metformin or proton pump inhibitors.
Tongue cancer is also more common after age 50, particularly among individuals with a history of tobacco use or alcohol consumption. However, the rising prevalence of HPV-associated oropharyngeal cancers has led to increasing incidence in younger, non-smoking populations as well.
In clinical practice, this age overlap can complicate diagnosis — especially when a 60-year-old patient presents with glossitis and fatigue. Without thorough history-taking and targeted diagnostic tests, there’s a risk of attributing malignant symptoms to a benign nutritional cause or vice versa.
Nutritional Recovery vs. Oncological Rehabilitation
Patients recovering from vitamin B12 deficiency typically experience a full return to health, especially when the cause is identified early and corrected effectively. Oral symptoms such as glossitis and mouth pain usually resolve within days to weeks after treatment begins. Neurological improvements may take longer — several weeks or months — but most cases stabilize with consistent supplementation.
Rehabilitation for tongue cancer is far more complex. After tumor resection, patients often require reconstructive surgery, which may involve grafts or flaps to restore tongue function. Speech therapy, swallowing therapy, and dietary modifications are essential for regaining quality of life. Some patients develop chronic dysphagia or altered speech due to partial tongue removal or radiation-induced fibrosis.
This stark contrast underscores the importance of correct diagnosis. A treatable nutritional issue must not be mistaken for malignancy — and cancer must not be mistaken for a minor irritation.
Psychological Impact and Patient Perception
Emotionally, vitamin B12 deficiency can cause significant distress, especially when symptoms mimic serious neurological or psychiatric conditions. Patients often feel anxious about unexplained fatigue, memory lapses, or numbness, fearing conditions like dementia or multiple sclerosis. Fortunately, once the cause is identified, treatment provides rapid reassurance and symptom reversal.
In tongue cancer, the psychological burden is heavier and often prolonged. Patients face uncertainty about survival, visible disfigurement, fear of recurrence, and treatment side effects. Eating and speaking — two deeply human acts — are disrupted, leading to frustration, isolation, or depression. Access to mental health services, support groups, and long-term survivorship care is vital for emotional healing.
The patient journey in both conditions demands empathy and patient-centered communication — from diagnosis to recovery or palliative support.
Public Health Messaging and Awareness
From a public health perspective, increasing awareness about vitamin B12 deficiency is crucial — particularly in elderly, vegan, or chronically medicated populations. Educational campaigns should emphasize dietary sources, signs of deficiency, and the importance of routine blood tests for high-risk individuals. B12 testing is inexpensive, widely available, and easily actionable.
Tongue cancer awareness, on the other hand, is less prevalent in the public domain despite its severity. Early signs are often missed because people expect cancer to be painful or visible. Oral screenings during dental checkups, anti-smoking education, and HPV vaccination all play roles in prevention and early detection.
Clear communication — both at the community and clinical levels — can prevent delays and reduce disease burden in both conditions.
Summary of Core Differences
The core differences between vitamin B12 deficiency and tongue cancer lie in origin, reversibility, urgency, and systemic impact.
Vitamin B12 deficiency:
- Is reversible and usually benign
- Emerges slowly and systemically
- Presents with diffuse oral and neurological symptoms
- Responds rapidly to supplementation
Tongue cancer:
- Is malignant and potentially life-threatening
- Can arise suddenly with localized pain or ulceration
- Requires biopsy, imaging, and multimodal oncological treatment
- Demands long-term physical and emotional rehabilitation
Recognizing these distinctions early is critical to avoid dangerous diagnostic errors. Just as we differentiate skin metastases in breast cancer from dermatitis or appendix cancer from abdominal discomfort, oral lesions demand focused evaluation — not assumptions.
FAQ
How do I know if my tongue pain is from B12 deficiency or something more serious?
If the pain is generalized, burning, or accompanied by fatigue and other systemic symptoms like numbness, it may be from B12 deficiency. However, if there’s a specific sore or mass that doesn’t heal within two weeks, it should be evaluated for tongue cancer.
What does a tongue look like with B12 deficiency?
The tongue often appears smooth, swollen, and red — sometimes described as “bald” or glossy. There may be pain, burning, or sensitivity, particularly when eating acidic or spicy foods.
Can tongue cancer be mistaken for a nutritional deficiency?
Yes, early tongue cancer can mimic benign conditions like glossitis or ulcers. Persistent lesions that don’t respond to nutritional intervention or topical treatment must be biopsied.
Is vitamin B12 deficiency reversible?
In most cases, yes. If treated early with appropriate supplementation (oral or injectable), both hematologic and neurologic symptoms can resolve, often completely.
What causes tongue cancer?
The primary causes include tobacco use, heavy alcohol consumption, HPV infection, and chronic irritation from dental factors. These lead to DNA mutations in the squamous cells of the tongue.
How is B12 deficiency diagnosed?
Doctors typically use a combination of serum B12 levels, complete blood counts, and markers like methylmalonic acid or homocysteine to confirm deficiency.
How is tongue cancer diagnosed?
Diagnosis involves a physical oral exam, biopsy of the lesion, and imaging tests such as MRI or CT to determine spread and staging.
Does B12 deficiency cause ulcers or bleeding in the mouth?
It can cause soreness and ulcers, but spontaneous bleeding is uncommon. Bleeding or rapidly enlarging lesions warrant further investigation.
Can you have both conditions at once?
It’s possible, especially in older adults or those with multiple risk factors. That’s why a full workup is essential if symptoms don’t improve with treatment.
What are the long-term risks of untreated B12 deficiency?
Without treatment, it can lead to irreversible nerve damage, difficulty walking, cognitive decline, and severe anemia.
Is tongue cancer curable?
Yes, if detected early. Localized tumors can often be cured with surgery and radiation. Advanced cases are harder to treat but may still be manageable.
Does B12 deficiency affect speech or swallowing?
Yes, glossitis and tongue inflammation can cause discomfort during speech and swallowing, but this typically resolves with treatment.
How quickly does tongue cancer progress?
Progression can vary. Some tumors are slow-growing, while others are aggressive. Regular monitoring of suspicious lesions is crucial to catch changes early.
Can lifestyle changes prevent these conditions?
A balanced diet can prevent B12 deficiency. Avoiding tobacco and alcohol, maintaining oral hygiene, and receiving the HPV vaccine can reduce tongue cancer risk.
When should I see a doctor for tongue changes?
If you notice a sore, patch, or lump on your tongue that doesn’t heal within two weeks — especially if accompanied by pain or bleeding — consult a healthcare provider immediately.












