Dense Dose Doxorubicin and Cyclophosphamide for Effective Breast Cancer Treatment
- What Is Dense Dose Chemotherapy?
- How the Regimen Is Administered
- Timeline and Duration of Treatment
- Benefits and Risks Compared to Standard Chemotherapy
- Understanding Chemotherapy Dose Density in Breast Cancer
- Treatment Schedule and Administration Protocol
- Understanding Side Effects of Dense Dose AC Therapy
- Impact on Blood Counts and Immune Function
- Long-Term Risks and Cardiac Toxicity
- Monitoring Schedule and Lab Tests: Dense Dose AC Protocol
- Assessing Effectiveness of Dense Dose AC in Breast Cancer Subtypes
- Psychosocial and Emotional Impact on Patients
- Comparison with Other Chemotherapy Regimens
- Role of Growth Factor Support in Dense Dose Therapy
- Patient Selection Criteria for Dose-Dense Chemotherapy
- Real-World Application and Modifications in Community Settings
- Comparing Dense Dose AC with Other Regimens
- Clinical Trial Data Supporting Dense Dose AC
- FAQ
What Is Dense Dose Chemotherapy?
The Concept Behind Dose-Dense Schedules
Dense dose chemotherapy refers to giving standard chemotherapy drugs more frequently, usually every two weeks instead of every three. The goal is to minimize tumor regrowth between cycles. This approach is grounded in mathematical tumor modeling, which shows that shortening the interval between doses can increase the cytotoxic impact on cancer cells.
Why Doxorubicin and Cyclophosphamide Are Used Together
Doxorubicin (an anthracycline) and cyclophosphamide (an alkylating agent) work synergistically. Doxorubicin interferes with DNA replication, while cyclophosphamide causes cross-linking of DNA strands, effectively halting cancer cell division. Used in tandem, these drugs have shown increased efficacy, especially in aggressive and triple-negative breast cancers.
Clinical Evidence Supporting Dense Dose Schedules
Several clinical trials, including CALGB 9741, demonstrated that dose-dense schedules improve disease-free survival and overall survival in high-risk, node-positive breast cancer. A 2021 review comparing weekly vs bi-weekly administration also indicated better outcomes for younger patients under 50.
How the Regimen Is Administered
Typical Protocol for Dose-Dense AC
Patients typically receive doxorubicin at 60 mg/m² and cyclophosphamide at 600 mg/m² every 14 days for four cycles. Growth factor support (commonly filgrastim or pegfilgrastim) is administered to help maintain white blood cell counts and reduce the risk of neutropenia.
Role of Pegfilgrastim in Supporting Blood Counts
Without granulocyte colony-stimulating factor (G-CSF) support, the bone marrow may not recover quickly enough between cycles. Pegfilgrastim (Neulasta) is given approximately 24 hours post-infusion and dramatically reduces hospitalization due to febrile neutropenia.
Adjustments for Age or Comorbidities
Older patients or those with pre-existing heart conditions may require reduced doses or longer intervals. Monitoring with echocardiograms is essential when using doxorubicin due to its cardiotoxic potential.
Timeline and Duration of Treatment
Standard Course and Milestones
The entire dose-dense AC regimen spans roughly 8 weeks. After completion, many protocols include paclitaxel-based continuation, either weekly or every 14 days. Milestones are assessed via imaging, tumor markers, and clinical exams after every two cycles.
Time Between Cycles and Recovery Markers
Patients must maintain ANC (absolute neutrophil count) >1500/μL and platelet count >100,000/μL to proceed with the next cycle. If blood counts fall below these thresholds, treatment may be delayed, or G-CSF doses adjusted.
How Patients Should Prepare for Each Cycle
Hydration, antiemetics, and heart monitoring are vital before each infusion. Long-term use of a port-a-cath is often recommended to reduce vein damage and improve drug delivery.
Benefits and Risks Compared to Standard Chemotherapy
Improved Disease-Free Survival
Data from meta-analyses indicate a ~30% reduction in recurrence for patients receiving dose-dense regimens, particularly in ER-negative subtypes. For premenopausal women, the gains are even more pronounced.
Elevated Toxicity and Management Strategies
While outcomes may improve, the dense schedule can lead to more acute toxicities — notably fatigue, mucositis, and anemia. Integrative strategies including diet adjustments, iron supplementation, and careful dental hygiene play a key role.
Is It Always the Best Option?
Not all patients benefit equally. Those with HR-positive/HER2-negative cancers may not gain as much from intensified dosing. In such cases, genomic assays like Oncotype DX can help determine the need for chemotherapy intensity.
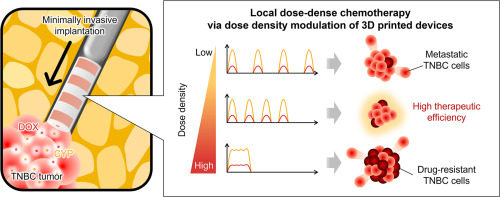
Understanding Chemotherapy Dose Density in Breast Cancer
Chemotherapy dose density refers to the frequency at which chemotherapeutic agents are administered. In dense-dose regimens, medications like doxorubicin and cyclophosphamide are given in shorter intervals, typically every two weeks, rather than the standard three. This approach aims to limit the time cancer cells have to recover between treatments, thereby improving tumor control. While it can be more effective in aggressive breast cancers, such as triple-negative or node-positive types, it may increase the risk of hematological toxicity. Medical teams usually counter this by administering growth factors like filgrastim to support white blood cell recovery.
Mechanism of Action of Doxorubicin and Cyclophosphamide
Doxorubicin is an anthracycline that works by intercalating DNA strands and inhibiting topoisomerase II, leading to apoptosis of rapidly dividing cells. Cyclophosphamide, on the other hand, is an alkylating agent that cross-links DNA, ultimately impeding DNA replication. When combined, these drugs have a synergistic cytotoxic effect on breast cancer cells. However, their toxicity profiles must be monitored closely, especially cardiac toxicity from doxorubicin and potential bladder damage from cyclophosphamide. Patients undergoing this regimen are often required to undergo routine cardiac evaluations and hydration protocols to minimize long-term side effects.
Eligibility Criteria for Dense Dose Regimens
Dense dose AC chemotherapy is typically considered for early-stage but high-risk breast cancer patients. Candidates often include those with lymph node involvement, HER2-negative status, or triple-negative receptor profiles. However, age, cardiac function, bone marrow reserve, and performance status play critical roles in determining a patient’s suitability. This is especially relevant for older adults or individuals with preexisting conditions, as the aggressive nature of dose-dense therapy may lead to higher toxicity. Clinical decisions are often guided by genomic testing tools like Oncotype DX, which help determine recurrence risk and chemotherapy benefit.
Treatment Schedule and Administration Protocol
| Component | Standard Regimen | Dose-Dense Regimen |
| Doxorubicin | 60 mg/m² every 3 weeks | 60 mg/m² every 2 weeks |
| Cyclophosphamide | 600 mg/m² every 3 weeks | 600 mg/m² every 2 weeks |
| Duration (Cycles) | 4 cycles (12 weeks) | 4 cycles (8 weeks) |
| G-CSF Support | Not routinely required | Required with each cycle |
| Common Use | Low-to-intermediate risk | High-risk, aggressive types |
Some oncologists emphasize that dosed schemes can be particularly effective in aggressive forms – especially when treatment requires a rapid tumor reaction.
Understanding Side Effects of Dense Dose AC Therapy
Dense dose doxorubicin and cyclophosphamide (AC) therapy, while effective, is associated with a range of side effects that can significantly impact quality of life. The accelerated schedule intensifies the typical adverse effects, making it essential to educate patients on what to expect. Commonly reported symptoms include nausea, fatigue, neutropenia, and hair loss. These are more pronounced due to shorter intervals between treatments, leaving the body with less time to recover.
Fatigue is often cumulative and may peak during the final cycles. Nausea is typically managed with premedication using antiemetics, but breakthrough nausea can still occur. Neutropenia, or low white blood cell count, may lead to infections, which is why granulocyte colony-stimulating factors (G-CSFs) like filgrastim are commonly co-administered. While these side effects are challenging, understanding them in advance allows for proactive management and better patient outcomes.
Impact on Blood Counts and Immune Function
One of the hallmark concerns with dose-dense chemotherapy regimens is hematological toxicity. Both doxorubicin and cyclophosphamide suppress bone marrow activity, leading to decreases in red and white blood cells and platelets. The dense scheduling intensifies this effect, raising the risk of anemia, infections, and bleeding episodes.
Weekly complete blood count (CBC) monitoring is mandatory during treatment. The most dangerous complication is febrile neutropenia—a condition requiring immediate medical attention due to the risk of sepsis. Supportive care such as erythropoiesis-stimulating agents (ESAs) may be considered in certain cases, although these carry their own risks and are used selectively.
Importantly, patients undergoing dense dose AC are often educated to recognize signs of infection early, including fever, chills, or unusual fatigue. Infection prevention protocols, including hand hygiene and food safety, are emphasized throughout the regimen.
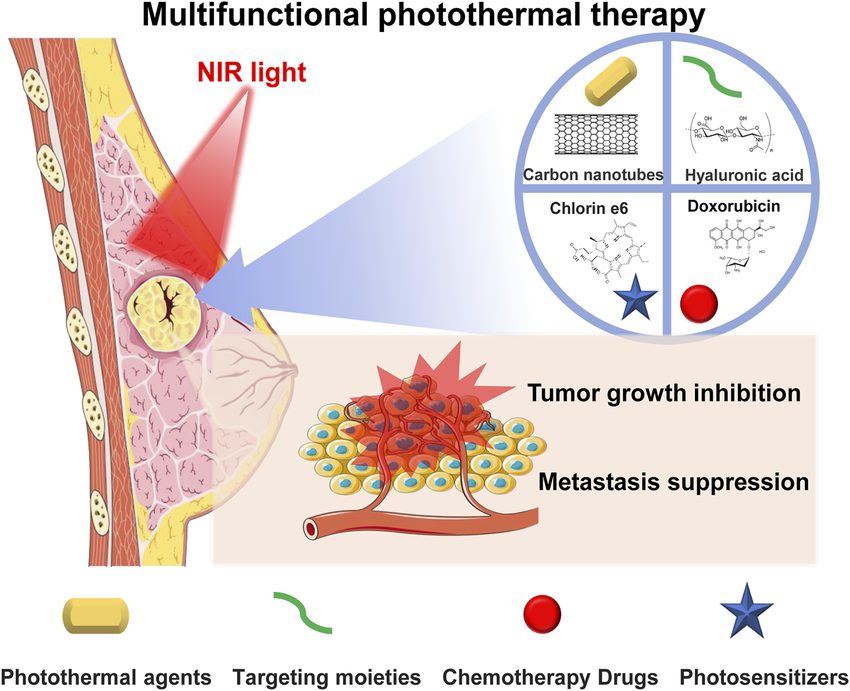
Long-Term Risks and Cardiac Toxicity
While dense dose AC therapy is a cornerstone of aggressive breast cancer management, it carries significant long-term risks, particularly cardiac toxicity. Doxorubicin is known for its cumulative dose-dependent cardiotoxic effects. Patients with pre-existing cardiac conditions, or those receiving concurrent radiotherapy to the chest, are at elevated risk.
Cardiac monitoring with echocardiograms or MUGA scans is essential before and during therapy, especially if the cumulative doxorubicin dose approaches 400–450 mg/m². Symptoms like shortness of breath, fluid retention, or irregular heartbeat warrant immediate cardiological evaluation.
These long-term complications must be weighed against the aggressive control of metastatic disease, particularly in cases where breast cancer has progressed to skin metastases—a clinical situation that may benefit from dose-intensified regimens.
Monitoring Schedule and Lab Tests: Dense Dose AC Protocol
| Monitoring Type | Frequency | Purpose |
| CBC (Complete Blood Count) | Weekly | Monitor for neutropenia, anemia, thrombocytopenia |
| Renal Function (Creatinine, BUN) | Bi-weekly | Ensure kidney clearance of cyclophosphamide |
| Hepatic Panel (AST, ALT, ALP, Bilirubin) | Bi-weekly | Check liver function due to drug metabolism |
| Cardiac Imaging (Echocardiogram or MUGA) | Before start and every 2–3 cycles | Assess left ventricular ejection fraction (LVEF) |
| Symptom Assessment (Fatigue, Nausea, Infections) | Each visit | Adjust supportive care and medications |
| Oncology Consultation | Every cycle | Evaluate treatment response and adjust dose if needed |
Occasionally, symptoms such as oral discomfort or glossitis may raise concerns about tongue cancer versus vitamin B12 deficiency, highlighting the importance of comprehensive assessment during treatment.
Assessing Effectiveness of Dense Dose AC in Breast Cancer Subtypes
Dense dose AC has shown particular benefit in treating high-risk breast cancer subtypes such as triple-negative and HER2-positive tumors. Its accelerated dosing enhances cell kill by minimizing tumor repopulation between cycles. Several studies have demonstrated improved disease-free survival (DFS) and overall survival (OS) rates compared to standard scheduling in specific cohorts.
However, the response varies significantly depending on tumor biology. In estrogen receptor-positive (ER+) cancers, the benefit may be less pronounced compared to hormone therapy or targeted agents. Genomic assays like Oncotype DX and MammaPrint are often used to stratify patients based on recurrence risk before initiating such an intensive regimen.
Real-world data confirm that patients with high-grade, node-positive disease derive the most benefit. For this reason, oncologists personalize treatment protocols to match the aggressiveness of the tumor with the intensity of the chemotherapy.
Psychosocial and Emotional Impact on Patients
Undergoing dense dose chemotherapy can be emotionally taxing for patients. The compressed treatment schedule leaves less time for physical and psychological recovery. Common emotional responses include anxiety, depression, and feelings of isolation. These may be exacerbated by physical symptoms like alopecia or fatigue, which can affect self-image and daily functioning.
Support services such as counseling, peer groups, and psycho-oncology referrals play a critical role. It is important to normalize these reactions and proactively address them within the care plan. Patients often benefit from continuity of care with the same oncology team, which fosters trust and psychological stability during difficult phases.
Additionally, the anxiety about potential recurrence and long-term effects can persist after treatment ends. Structured survivorship programs are essential to help patients transition from active treatment to recovery.
Comparison with Other Chemotherapy Regimens
Dense dose AC is one of several options in the adjuvant and neoadjuvant treatment landscape for breast cancer. Alternatives include standard-dose AC, TC (docetaxel and cyclophosphamide), and combination protocols such as AC-T (followed by paclitaxel). Each has its own efficacy and toxicity profile, and choice often depends on staging, biomarkers, and patient comorbidities.
For example, older patients or those with cardiac risk may be steered toward regimens without anthracyclines due to their cardiotoxicity. Conversely, patients with aggressive features might be escalated to a dose-dense approach for better outcomes.
It is worth noting that in cancers with more complex metastatic presentations, such as nasal cancer in dogs, treatment protocols are also tailored based on progression and systemic tolerance—illustrating the broader oncology principle of balancing efficacy with patient burden.
Role of Growth Factor Support in Dense Dose Therapy
A crucial enabler of dense dose chemotherapy is the co-administration of growth factor support, primarily granulocyte colony-stimulating factors (G-CSFs). Without these agents, the risk of severe neutropenia would make dose-dense scheduling impractical for most patients.
Filgrastim (Neupogen) and pegfilgrastim (Neulasta) are commonly used. Filgrastim is given daily for several days post-chemotherapy, while pegfilgrastim is a single injection per cycle. These agents stimulate the bone marrow to produce white blood cells faster, reducing infection risk and hospitalization rates.
Growth factor support is not without side effects—bone pain, injection site discomfort, and rare cases of splenic rupture have been reported. Nevertheless, their inclusion in dense dose AC protocols is considered standard of care due to their clear benefit in maintaining dose intensity and minimizing interruptions.
Patient Selection Criteria for Dose-Dense Chemotherapy
Not every patient with breast cancer is a candidate for dose-dense chemotherapy. The selection process is rigorous and based on clinical staging, tumor biology, and individual risk of recurrence. Generally, it is preferred for node-positive cases, triple-negative tumors, and HER2-negative cancers with high proliferation indices.
Patients must also demonstrate sufficient bone marrow reserve and adequate organ function. Age is a factor, but not an absolute exclusion—fit older adults may still tolerate dense schedules with appropriate supportive care.
An oncologist’s evaluation often includes genomic assays such as Oncotype DX to gauge recurrence risk and decide whether the intensity of dense dosing is justified. In contrast, when symptoms of fatigue or oral pain occur, differential diagnosis is crucial, as these could point to other underlying issues.
Real-World Application and Modifications in Community Settings
In practice, dose-dense chemotherapy protocols often require adjustments based on patient tolerance and logistical limitations. Community oncology clinics, unlike academic centers, may lack the infrastructure for strict two-week cycles. Modifications—such as occasional dose delays or skipped growth factor doses—are common and acceptable within certain parameters.
Physician judgment plays a key role in balancing efficacy with patient experience. Real-world studies show that even with slight deviations, outcomes remain favorable in most cases. Supportive care remains a cornerstone of this regimen, particularly as patients cycle through four intensive infusions over eight weeks.
Patients should be made aware that treatment plans may evolve during the course of therapy, and such changes do not necessarily compromise overall success. This is particularly true in complex cases where supportive care takes precedence—paralleling considerations seen in advanced cancers like Stage 4 appendix cancer, where adaptability is critical.
Comparing Dense Dose AC with Other Regimens
While dense dose doxorubicin and cyclophosphamide is widely used, it is not the only effective regimen for early-stage breast cancer. Alternatives include:
- TC (docetaxel + cyclophosphamide): Often used for HER2-negative, node-negative disease.
- AC followed by paclitaxel: A sequential schedule used frequently for triple-negative subtypes.
- Anthracycline-free regimens: For patients with contraindications to doxorubicin, such as cardiac issues.
Each option has trade-offs in terms of toxicity, efficacy, and scheduling. In head-to-head trials, dose-dense AC often yields better disease-free survival but may carry higher short-term toxicity.
Decision-making should be individualized and based on tumor characteristics, patient preference, and comorbidities. Just as in differential diagnostic decisions—such as distinguishing tongue cancer from B12 deficiency—nuance and clinical judgment are key.
Clinical Trial Data Supporting Dense Dose AC
Multiple randomized controlled trials (RCTs) have validated the benefit of dense dose AC, particularly in high-risk breast cancer patients. The landmark CALGB 9741 trial was among the first to demonstrate a significant survival advantage by compressing the chemotherapy schedule.
In this trial, patients receiving AC followed by paclitaxel every two weeks showed superior overall survival (OS) and disease-free survival (DFS) compared to those on a three-week cycle. The results were most pronounced in node-positive and triple-negative subgroups.
Subsequent meta-analyses confirmed these findings, establishing dose-dense therapy as a standard of care for eligible patients. Ongoing studies continue to assess how best to combine dense dosing with newer therapies such as immunotherapy or PARP inhibitors.
Evidence from trials is essential to justify the use of more toxic and costly regimens. As with any aggressive therapy, the data must support its application, much like how rare presentations of cancer, such as lower eyelid tumors, require specific evidence-based approaches to avoid overtreatment
FAQ
What is dense dose chemotherapy?
Dense dose chemotherapy is an intensified treatment schedule in which chemotherapy drugs are administered more frequently—typically every two weeks instead of the traditional three. The purpose is to reduce the opportunity for cancer cells to recover between cycles, potentially leading to improved long-term outcomes for certain types of breast cancer.
Why are doxorubicin and cyclophosphamide used together in breast cancer?
These two drugs work synergistically: doxorubicin interferes with the DNA inside cancer cells, preventing replication, while cyclophosphamide causes cross-linking in DNA strands, making cell division impossible. Combined, they form a powerful regimen used for early-stage and high-risk breast cancers, improving the chance of remission.
Is dense dose chemotherapy more effective than standard-dose schedules?
For specific patient groups, including those with hormone receptor-negative or triple-negative breast cancers, dense dose chemotherapy has demonstrated modest survival benefits. However, its effectiveness depends on individual tumor biology, patient tolerance, and risk classification.
What are the side effects of this chemotherapy approach?
Patients often experience nausea, vomiting, fatigue, neutropenia (low white blood cells), and hair loss. Doxorubicin in particular poses risks to heart health, while cyclophosphamide may lead to bladder toxicity. Supportive therapies like growth factors are commonly used to manage hematologic side effects.
How long does the treatment typically last?
The dense dose regimen usually consists of four cycles of doxorubicin and cyclophosphamide given every two weeks, totaling about eight weeks. This is often followed by additional chemotherapy agents such as paclitaxel, extending the full course to approximately 16–20 weeks depending on the treatment plan.
Can this treatment affect fertility?
Yes, both drugs are known to carry a risk of temporary or permanent infertility. Women who wish to preserve fertility should consult a reproductive specialist prior to beginning therapy to explore options such as egg or embryo preservation.
How is neutropenia managed during dense dose treatment?
Growth factors like pegfilgrastim or filgrastim are routinely administered to stimulate white blood cell production. These agents reduce the risk of infections and allow the chemotherapy schedule to stay on track without delay due to low counts.
Are there any long-term complications?
Long-term effects may include cardiac issues from cumulative exposure to doxorubicin, early menopause, bone density loss, and even secondary cancers such as leukemia. Monitoring and follow-up are essential after treatment completion to address late toxicities.
Is this regimen suitable for older adults?
Age alone isn’t a barrier, but elderly patients may have additional comorbidities that complicate treatment. Geriatric assessments and individualized treatment plans help determine whether a dense dose regimen is appropriate for older individuals.
Can this treatment be used in metastatic breast cancer?
Dense dose chemotherapy is more commonly used in early-stage or high-risk settings. In metastatic cases, where the goal is disease control rather than cure, less intensive regimens are generally preferred to minimize side effects and preserve quality of life.
How are patients monitored during the course of therapy?
Patients undergo regular blood tests, cardiac assessments (such as echocardiograms), and physical evaluations. Monitoring ensures the patient is tolerating treatment well and that no organ systems are being unduly affected by the drugs’ toxicities.
What should I eat during treatment?
Patients are advised to follow a balanced diet rich in protein, vegetables, and fluids. Bland, soft foods may be helpful during bouts of nausea or mucositis. It’s also crucial to avoid raw or undercooked foods that could introduce bacteria while the immune system is compromised.
Are there alternatives to this approach?
Yes, depending on tumor subtype and stage, patients may be candidates for hormone therapy, HER2-targeted therapy, immunotherapy, or participation in clinical trials. Standard chemotherapy on a 3-week schedule is also a viable option for some individuals.
Does insurance typically cover dense dose chemotherapy?
In most developed healthcare systems, including the U.S., dense dose regimens are part of standard-of-care protocols for eligible patients and are covered by insurance. However, patients should always confirm coverage, particularly for supportive medications like growth factors.
Is dense dose chemotherapy safe?
When administered under close medical supervision, with supportive care and monitoring, dense dose AC chemotherapy is considered safe for appropriately selected patients. Risk-benefit analysis is key, and patients must be thoroughly informed about potential side effects and required follow-up.