Complete Blood Count and Cancer Detection: Innovations in 2025
- Part One — Introduction
- Part Two — Understanding CBC Parameters
- Part Three — CBC in Cancer Screening
- Part Four — Technological Advancements
- Part Five — Case Studies and Clinical Trials
- Part Six — Implementation in Clinical Practice
- Part Seven — Recent Developments (2025–2026)
- Part Eight — Future Prospects
- Frequently Asked Questions (FAQ)
- Conclusion
Introduction
Have you ever paused to think about what a simple blood test can tell us? Many of us have had blood drawn during a doctor’s visit, but the results often feel like a mystery—a string of numbers and abbreviations that don’t quite reveal their full story. One of the most common blood tests is the Complete Blood Count, or CBC, and it’s quietly one of the most informative snapshots of our health.
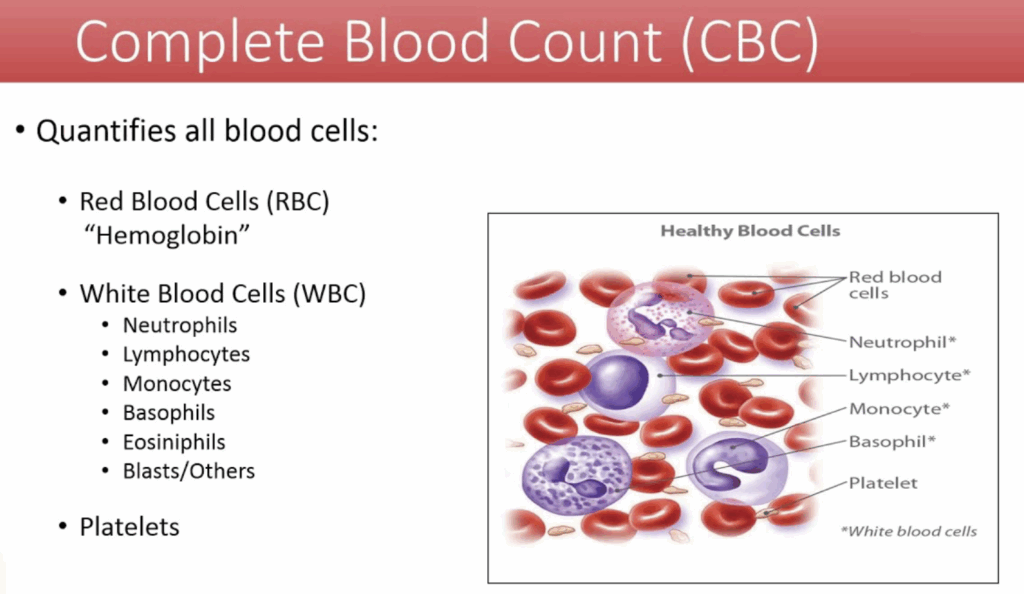
At its core, a CBC measures the different types and quantities of cells in your blood. These cells—red blood cells, white blood cells, and platelets—each serve vital functions. Red blood cells ferry oxygen throughout your body, white blood cells defend against infection, and platelets help blood clot when you get injured. The balance and levels of these cells tell doctors a lot about how your body is functioning.

Traditionally, CBC tests have been used to diagnose anemia, infections, and blood disorders. But in 2025, the role of the CBC is expanding dramatically, especially in the realm of cancer detection. Why does that matter? Because cancer doesn’t just create tumors—it can subtly alter your blood long before symptoms show up or imaging scans pick anything up.
You might wonder: can a routine blood test really help catch cancer early? The answer lies in understanding that many cancers affect blood cells or the bone marrow where they’re produced, causing changes that can be detected through CBC parameters. Blood cancers like leukemia and lymphoma often cause dramatic shifts in white blood cells, making CBC a natural part of diagnosis. But even solid tumors—think lung, colon, or breast cancers—can influence blood cell counts indirectly, through inflammation or bone marrow impact.
What’s exciting about 2025 is how technology is amplifying this potential. Advances in artificial intelligence and machine learning allow us to see patterns in CBC data that were invisible before—patterns that could signal cancer risk much earlier than traditional methods.
This means that the CBC, once a simple lab test, is evolving into a sophisticated, non-invasive screening tool. It offers a glimpse into your body’s health that’s not only more accessible and affordable but also increasingly precise.
As you read on, you’ll discover how CBC parameters work, how they’re interpreted, and how innovations are transforming this everyday test into a frontline player in cancer detection. Whether you’re a healthcare professional or just curious about medical advances, understanding the CBC’s growing role might change how you view your next blood test—turning a routine procedure into a potential lifesaver.
Understanding CBC Parameters
When you first see a Complete Blood Count report, it might look like a jumble of letters and numbers—RBCs, WBCs, hemoglobin, hematocrit, platelets. It’s easy to overlook how much information those figures hold. But once you understand what each of these parameters actually measures, you begin to see why the CBC is such a cornerstone in health assessment—and why it matters in the context of cancer.
Take red blood cells (RBCs), for instance. They’re the oxygen couriers, traveling tirelessly through your bloodstream to keep every cell in your body nourished. A dip in their numbers could indicate anemia, which sometimes creeps in when cancer interferes with the bone marrow or causes internal bleeding. It’s subtle, but this kind of anemia might be one of the earliest signs that something’s amiss.
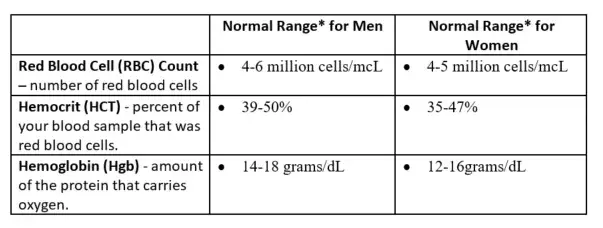
Then there’s hemoglobin, the protein that gives red blood cells their color and their ability to bind oxygen. Alongside hematocrit—which tells us what portion of your blood volume is made up of these cells—these numbers offer insight into your blood’s oxygen-carrying capacity. In cancer patients, changes here can reflect the body’s struggle to maintain balance.
White blood cells (WBCs), on the other hand, are the guardians of your immune system. When you see their count rise or fall, it’s a clue that your body is reacting—sometimes to infection, other times to inflammation or even malignancy. In blood cancers like leukemia, abnormal WBC counts and types can be a direct red flag.
The breakdown of these white blood cells—the differential—adds even more nuance. The specific types of WBCs fluctuating can suggest very different things: an increase in lymphocytes might hint at certain lymphomas, while a decrease in neutrophils could point to bone marrow suppression. Platelets, those tiny blood fragments that help clotting, also tell a story. Too few or too many platelets might signal an underlying issue affecting blood production.
But here’s the key: no single number tells the whole story. It’s patterns and changes over time that catch attention. Imagine reading the CBC as listening to an orchestra rather than a solo instrument. One off note might go unnoticed, but several out-of-tune instruments together create a melody that demands a closer look.
This interplay of subtle signals is not unlike what we observe in mental health diagnostics, as discussed in Mental Health Trends 2025, where longitudinal tracking and contextual interpretation are essential to understanding nuanced physiological changes.
And this is why doctors rarely make decisions based on just one CBC test. They want to see trends, symptoms, patient history. The CBC gives hints, but understanding what those hints mean requires a bigger picture—a puzzle where every piece matters.
What’s really fascinating is how these routine parameters, which have been measured the same way for decades, now serve as the foundation for revolutionary approaches in cancer detection. We’re learning to interpret these clues more deeply than ever before, which is opening up exciting possibilities for earlier diagnosis and better outcomes.
CBC in Cancer Screening
With a clearer understanding of what a CBC measures, it’s natural to wonder how this test fits into cancer screening. After all, can a blood test really help catch cancer before symptoms appear? The answer lies somewhere between “not always” and “increasingly yes,” depending on the cancer type and context.
Cancers that involve the blood and bone marrow—like leukemias and lymphomas—often produce clear abnormalities visible in a CBC. Because these diseases directly affect the cells counted in this test, changes tend to be more obvious and informative. This makes the CBC a valuable tool not only for diagnosis but also for monitoring how well treatment is working.
However, when it comes to solid tumors, things get trickier. These cancers don’t usually flood the bloodstream with abnormal cells, so they don’t always cause dramatic changes in blood counts early on. Yet, they can create more subtle effects—such as chronic inflammation that nudges white blood cell or platelet levels—or anemia caused by hidden bleeding or interference with bone marrow function.
This subtlety is both a challenge and an opportunity. The CBC alone cannot diagnose most solid tumors, but it can be an early signal that prompts further investigation. It’s like a canary in a coal mine—something that raises the alarm so doctors know where to look next.
Of course, this usefulness comes with limitations. Blood count changes aren’t unique to cancer; infections, autoimmune diseases, and even stress can cause similar shifts. This overlap means doctors have to interpret CBC results very carefully, always considering the broader clinical picture. The CBC is a piece of the diagnostic puzzle, but it’s rarely the whole picture.
Still, the value of the CBC in screening lies in its accessibility and cost-effectiveness. It’s a routine test, available almost anywhere, and when combined with other diagnostic methods and patient information, it enhances the likelihood of catching cancers earlier.
One of the most exciting developments today is how CBC data is being integrated with advanced analytics and artificial intelligence. Instead of flagging individual abnormal values, these tools look at complex patterns and subtle changes over time. This approach improves specificity, reducing false alarms and identifying those who might benefit most from additional testing.
While a CBC won’t replace specialized cancer screening tools like mammograms or colonoscopies anytime soon, its evolving role as a supportive screening measure is undeniable. Especially in settings where access to advanced imaging is limited, a sophisticated analysis of CBC could be a game-changer.
As you reflect on this, consider how something as routine as a blood count is gradually transforming from a basic snapshot into a powerful early detection tool—one that could help tip the scales in favor of timely cancer diagnosis.
Technological Advancements
By now, you’ve seen how the CBC offers important clues about our health and even cancer risks. But the real excitement in 2025 is how technology is revolutionizing the way we read and understand these clues. What used to be a straightforward report with a handful of numbers is now becoming a complex, data-rich insight powered by artificial intelligence and machine learning.
Imagine the old CBC test as a basic map — showing major landmarks but missing the intricate roads, alleys, and hidden paths. Today, AI acts like a sophisticated GPS, able to analyze patterns in ways that the human eye or traditional methods simply can’t. This technology isn’t just about spotting obvious abnormalities; it can detect subtle, complex changes across multiple blood parameters that together may hint at cancer far earlier than before.
This leap forward is not accidental. Over the past decade, advances in computing power and algorithms have made it possible to sift through enormous amounts of blood data collected from millions of patients. The patterns that emerge are often invisible to clinicians working alone but become clear when seen through the lens of machine learning.
And it’s not just about spotting cancer. The integration of AI with CBC data helps predict patient outcomes, guide treatment decisions, and even monitor responses to therapy in real-time. It’s like having a virtual assistant who continuously learns and adapts, providing doctors with smarter tools to make life-saving decisions faster.
In addition to AI, the test itself is evolving. New techniques are being developed to make CBC more sensitive and specific. For example, researchers are exploring how to analyze not only the quantity of blood cells but also their physical and biochemical properties—like shape, size, and protein markers on their surface. These details can add another layer of information, making the test even more powerful in detecting early-stage cancers that don’t yet cause obvious blood count changes.
All of this progress raises important questions about accessibility and implementation. How soon will these technologies be available in everyday clinics? What will it mean for healthcare costs? And how can clinicians be trained to effectively use these new tools without overwhelming them? The answers are still unfolding, but one thing is clear: the future of CBC in cancer detection is no longer just a lab test; it’s a convergence of medicine and cutting-edge technology working hand in hand.
This transformation also challenges us to rethink how we view routine blood tests. What was once considered a simple screening tool is now becoming a dynamic, evolving diagnostic powerhouse — and that’s a thrilling prospect for patients and providers alike.
Case Studies and Clinical Trials
When you hear about new medical tests or technologies, it’s natural to wonder: how do we really know they work? That’s where case studies and clinical trials come in. These real-world and controlled investigations help us see the CBC’s evolving role in cancer detection not just as theory, but as tested, evidence-based practice.
Over the last few years, a growing number of studies have explored how CBC data, especially when combined with AI analysis, can identify cancer at earlier stages. One particularly compelling example involved patients who initially had no symptoms but showed subtle changes in their CBC profiles. Through machine learning algorithms, researchers could detect patterns suggesting the presence of early-stage cancers such as lung, colorectal, and hematologic malignancies—sometimes months before traditional imaging or biopsies caught them.
What’s striking is that these early detections often led to less aggressive treatments and better patient outcomes. In some trials, patients flagged by enhanced CBC screening went on to receive interventions that prevented cancer progression. This is a huge leap from waiting for symptoms to appear or relying solely on more invasive tests.
Another important angle comes from studies assessing the CBC’s limitations and how to overcome them. Researchers have found that while individual CBC parameters can be noisy or nonspecific, analyzing them in combination drastically improves predictive accuracy. These findings reinforce the idea that the whole is greater than the sum of its parts, especially when sophisticated analytics are involved.
Still, no diagnostic method is perfect. Some cancers evade detection by CBC-based approaches, especially those that don’t affect blood cell production or immune response until late stages. Clinical trials continue to explore ways to refine algorithms and combine CBC data with other biomarkers to fill these gaps.
These studies also emphasize the importance of patient diversity. By including participants from varied backgrounds and health statuses, researchers are working to ensure that CBC-based cancer screening tools work well for everyone—not just select populations.
Interestingly, some of these lessons about data diversity and disease presentation parallel findings from outbreaks of diseases like Marburg virus, where rare presentations and atypical profiles challenge standard diagnostic approaches and emphasize the need for adaptable screening models.
Ultimately, these clinical investigations provide the backbone for turning promising concepts into everyday tools. They help clinicians gain confidence in using CBC data in cancer detection, shape guidelines, and inform healthcare policies.
So when you next hear about blood tests aiding early cancer detection, know that this progress is built on rigorous scientific work—careful trials, patient stories, and continuous improvement. It’s not just about technology, but about translating that tech into tangible benefits for real people.
Implementation in Clinical Practice
It’s one thing to develop cutting-edge technology in the lab or prove its value in clinical trials, but quite another to bring it into everyday healthcare. This transition—from research to real-world use—is often where promising tools face their biggest challenges. With CBC-based cancer detection innovations, the question becomes: how do clinics, hospitals, and doctors adopt these advances in a way that truly benefits patients?
First, there’s the practical side. Integrating AI-driven analysis and enhanced CBC testing into busy clinical workflows requires investment in new equipment and software. Health systems need to build infrastructure capable of handling large amounts of data securely and efficiently. This isn’t just about plugging in a new machine; it involves ensuring interoperability with existing electronic health records and laboratory information systems.
Then, there’s the human factor. Doctors and lab technicians must be trained not only to understand these new technologies but also to interpret their outputs effectively. This can feel overwhelming, especially for clinicians who are already juggling a heavy workload. Without proper education and support, the risk is that these sophisticated tools might be underused or misinterpreted, which could lead to missed diagnoses or unnecessary follow-ups.
Another layer involves healthcare policy and reimbursement. For new CBC technologies to become standard practice, insurance providers and national health systems need to recognize their value and cover the associated costs. This requires robust evidence of clinical benefit and cost-effectiveness—something that ongoing studies are striving to provide.
Despite these hurdles, many healthcare organizations are already piloting advanced CBC screening programs. These early adopters serve as testbeds, helping to identify best practices for implementation and to demonstrate real-world benefits. Their experiences will shape how widely and quickly these tools become part of routine care.
From a patient perspective, easier access to these advanced tests could mean earlier detection with less discomfort and fewer invasive procedures. But it also raises questions about communication—how to explain complex risk scores and what they mean for individual health without causing unnecessary anxiety.
The journey from innovation to routine clinical use is rarely straightforward. But with careful planning, investment, and collaboration among researchers, clinicians, policymakers, and patients, CBC-based cancer detection tools have the potential to become a standard part of the healthcare landscape—transforming how we approach early diagnosis and treatment.
Recent Developments (2025–2026)
As we step into the mid-2020s, the landscape of cancer diagnostics based on Complete Blood Count tests is shifting faster than many anticipated. Innovations that once felt futuristic are becoming tangible realities, influencing both clinical practice and healthcare policy.
One of the most exciting breakthroughs involves the refinement of AI algorithms trained on vast, diverse datasets. These enhanced models don’t just flag abnormal CBC values anymore; they identify complex, multidimensional patterns that distinguish cancer-related changes from those caused by infections, chronic diseases, or even temporary stress. This level of sophistication is opening doors to earlier and more accurate detection of a wider range of cancers, including some that have traditionally been difficult to catch early, like pancreatic or ovarian cancer.
At the same time, laboratory techniques have made strides beyond just counting cells. Cutting-edge methods now analyze blood cell morphology in unprecedented detail, including the subtle biochemical and physical changes that precede noticeable shifts in cell numbers. This adds a new layer of sensitivity and specificity to CBC tests, allowing for the detection of cancers at stages when intervention is more likely to be successful.
But breakthroughs in technology don’t happen in isolation. They require parallel advances in healthcare policy to ensure these innovations actually reach patients. Over the past year, we’ve seen several health authorities and professional societies update their screening guidelines to incorporate enhanced CBC analysis, especially for populations at higher risk of cancer. These policy changes acknowledge not only the improved accuracy of modern CBC diagnostics but also their potential to reduce dependence on more invasive or costly screening methods.
Additionally, some countries have begun pilot programs integrating AI-powered CBC screening into routine health checks, aiming to gather real-world data and refine best practices. These initiatives are crucial steps toward broader adoption, helping address questions about cost-effectiveness, patient acceptance, and healthcare system readiness.
One of the challenges policymakers are grappling with is balancing access and equity. As sophisticated CBC testing expands, there’s a concerted effort to ensure it’s available not just in top-tier hospitals but also in community clinics and underserved areas. After all, the promise of early cancer detection only fulfills its potential if these tools are accessible to all who need them.
Looking forward, recommendations for routine screenings are evolving from one-size-fits-all approaches to more personalized strategies. Enhanced CBC analysis, combined with individual risk factors like genetics, lifestyle, and family history, is paving the way for tailored screening schedules that maximize benefits and minimize unnecessary procedures.
In essence, the recent developments of 2025 and 2026 are not just about new technologies; they represent a broader transformation in how we think about early cancer detection—more precise, more patient-centered, and increasingly integrated into everyday healthcare.
Future Prospects
Looking ahead, the potential for Complete Blood Count tests to transform personalized medicine is truly thrilling. We’re moving beyond one-size-fits-all screening toward an era where your unique biology, lifestyle, and genetics shape how we use CBC data to detect and manage cancer.
Imagine a future where your routine blood test isn’t just compared against a generic reference range but analyzed in the context of your individual health profile. This means your CBC results could be interpreted differently than someone else’s, reflecting personal risk factors, previous health history, and even environmental exposures. Such tailored insights could help doctors recommend more precise screening intervals or preventive strategies uniquely suited to you.
This personalized approach is being powered by ongoing research that combines CBC data with other biomarkers and cutting-edge technologies like genomics and proteomics. By integrating multiple layers of information, scientists aim to create comprehensive health profiles that not only flag cancer risk earlier but also predict how a tumor might behave or respond to treatment.
Another exciting frontier lies in the continual refinement of AI algorithms that learn and adapt as they analyze more diverse datasets. These systems will become smarter over time, detecting ever more subtle patterns and improving predictive accuracy. They may even help identify new blood-based biomarkers that current technology can’t yet measure, unlocking further possibilities for non-invasive cancer detection.
Researchers are also exploring how advanced CBC analysis could monitor treatment responses in real-time. Instead of waiting weeks or months for imaging results, doctors might track how your blood parameters shift day-to-day, adjusting therapies dynamically to maximize effectiveness and minimize side effects.
Of course, realizing this future depends on overcoming challenges such as data privacy, ensuring equitable access, and maintaining rigorous validation of new tools. But the momentum is undeniable—medical research and technology are converging in ways that make personalized, CBC-based cancer detection more achievable than ever.
For patients, this means earlier diagnoses, fewer unnecessary tests, and treatments that fit their unique situation. For healthcare providers, it opens the door to more informed decision-making and better outcomes.
So, as you consider your next blood test, think about the incredible journey the humble CBC has undergone—from a simple cell count to a potential cornerstone of personalized cancer care. The innovations on the horizon promise to make it not just a routine test but a vital part of your individualized health story.
Frequently Asked Questions (FAQ)
1. What exactly is a Complete Blood Count (CBC), and why is it so commonly used?
A CBC is a fundamental blood test that measures the numbers and qualities of your red blood cells, white blood cells, and platelets. It’s widely used because it provides a quick, broad snapshot of your overall health and can indicate a variety of conditions—from infections and anemia to blood cancers—making it a first-line tool in many clinical settings.
2. How can a CBC help in detecting cancer if it only measures blood cells?
While a CBC doesn’t detect cancer directly like a biopsy or imaging scan, it reveals changes in blood cell counts or characteristics that often occur as a result of cancer’s effect on bone marrow or the immune system. For blood cancers like leukemia, these changes are usually obvious. For solid tumors, CBC changes can be subtle but still provide important early warning signs.
3. Are CBC results reliable for cancer screening?
CBC results are an important piece of the puzzle but not definitive on their own. Many non-cancer conditions can cause similar changes in blood counts, so doctors use CBC data in combination with symptoms, risk factors, and other tests. New AI-powered analyses are improving the accuracy by identifying complex patterns that humans might miss.
4. How is technology improving CBC’s role in cancer detection?
Advances in AI and machine learning allow for deeper analysis of CBC data, detecting subtle patterns across multiple blood parameters. Additionally, new lab methods analyze blood cell morphology and biochemistry to catch early changes before obvious count abnormalities occur. Together, these innovations are making CBC a more sensitive and specific screening tool.
5. Will CBC replace current cancer screening methods like mammograms or colonoscopies?
No, CBC isn’t replacing specialized screening tests anytime soon. Instead, it’s becoming a valuable adjunct tool—especially useful where access to imaging is limited or as a preliminary screen to identify who needs further testing. The goal is to complement existing methods and improve early detection rates overall.
6. What challenges exist in implementing advanced CBC testing in clinical practice?
Challenges include the need for infrastructure upgrades, training for healthcare professionals, and ensuring that AI tools are used appropriately alongside clinical judgment. There’s also the matter of policy and insurance coverage, which must evolve to support widespread adoption without increasing healthcare disparities.
7. What does the future hold for CBC in personalized medicine?
The future is promising. Personalized medicine will use CBC results alongside genetics, lifestyle, and other biomarkers to tailor cancer screening and treatment to the individual. Ongoing research and smarter AI systems will enhance early detection, monitor treatment responses, and improve patient outcomes, making CBC a key component of customized care.
Conclusion
The Complete Blood Count test has long been a staple of routine health checkups, quietly offering a window into our body’s inner workings. But in 2025, this humble test is undergoing a profound transformation. With the fusion of artificial intelligence, advanced laboratory techniques, and personalized medicine, CBC is evolving from a basic snapshot into a dynamic, powerful tool in the fight against cancer.
Its ability to detect subtle changes in blood cells—long before symptoms arise—holds the promise of earlier diagnoses, less invasive screening, and more tailored treatments. While challenges remain in integrating these innovations into everyday practice, ongoing research and policy developments are paving the way for broader, more equitable access.
For patients and providers alike, the enhanced CBC represents hope: hope for catching cancer earlier, improving survival rates, and ultimately, changing lives. As technology and medicine continue to advance hand in hand, the story of the Complete Blood Count reminds us that sometimes, the simplest tests can lead to the most profound breakthroughs.
And as we’ve seen with viral surveillance efforts—such as those detailed in our report on Avian Influenza H5N9—early detection, even through seemingly modest data streams, can dramatically shift outcomes when applied systematically and intelligently.









