Colon Cancer in Women: Recognizing the 7 Early Symptoms That Could Save Your Life
- Why Colon Cancer Symptoms in Women Are Often Overlooked
- Symptom 1: Unexplained Changes in Bowel Habits
- Symptom 2: Blood in the Stool or Rectal Bleeding
- Symptom 3: Persistent Abdominal Discomfort or Pain
- Symptom 4: Unexplained Fatigue and Weakness
- Symptom 5: Unexplained Weight Loss
- Symptom 6: A Feeling of Incomplete Evacuation After Bowel Movements
- Symptom 7: Nausea and Vomiting Unrelated to Infection
- How These Symptoms Differ From Other Female Health Issues
- Importance of Early Detection in Women
- Gender-Specific Challenges in Diagnosing Colon Cancer
- Risk Factors Specific to Women
- When to Talk to Your Doctor
- Misdiagnosis and Delayed Diagnosis in Women
- Diagnostic Tools and Screening Recommendations
- Prognosis and Survival Outlook
- Prevention and Lifestyle Measures
- FAQ: 7 Symptoms of Colon Cancer in Women
Why Colon Cancer Symptoms in Women Are Often Overlooked
Colon cancer in women is often misdiagnosed or ignored in early stages due to the subtlety of its symptoms and how easily they can be mistaken for menstrual, hormonal, or gastrointestinal changes. Unlike some other cancers with more apparent warning signs, colorectal malignancies can develop silently and progress before being caught. This delayed recognition has serious implications for survival, as early-stage colon cancer is far more treatable than later-stage disease.
Women may not associate changes in bowel habits or abdominal discomfort with something as serious as cancer. Many symptoms mimic conditions like irritable bowel syndrome (IBS), endometriosis, or even menopause. The purpose of this article is to break down the seven most critical symptoms of colon cancer in women, explain how they manifest, and help readers understand when to seek medical evaluation.
Symptom 1: Unexplained Changes in Bowel Habits
When Normal Patterns Become Irregular
One of the earliest and most commonly missed symptoms is a noticeable, unexplained change in bowel movements. Women might experience persistent constipation, diarrhea, or a change in the consistency or frequency of stools. These changes may occur gradually and often do not cause immediate alarm, especially if attributed to diet, stress, or hormonal fluctuations.
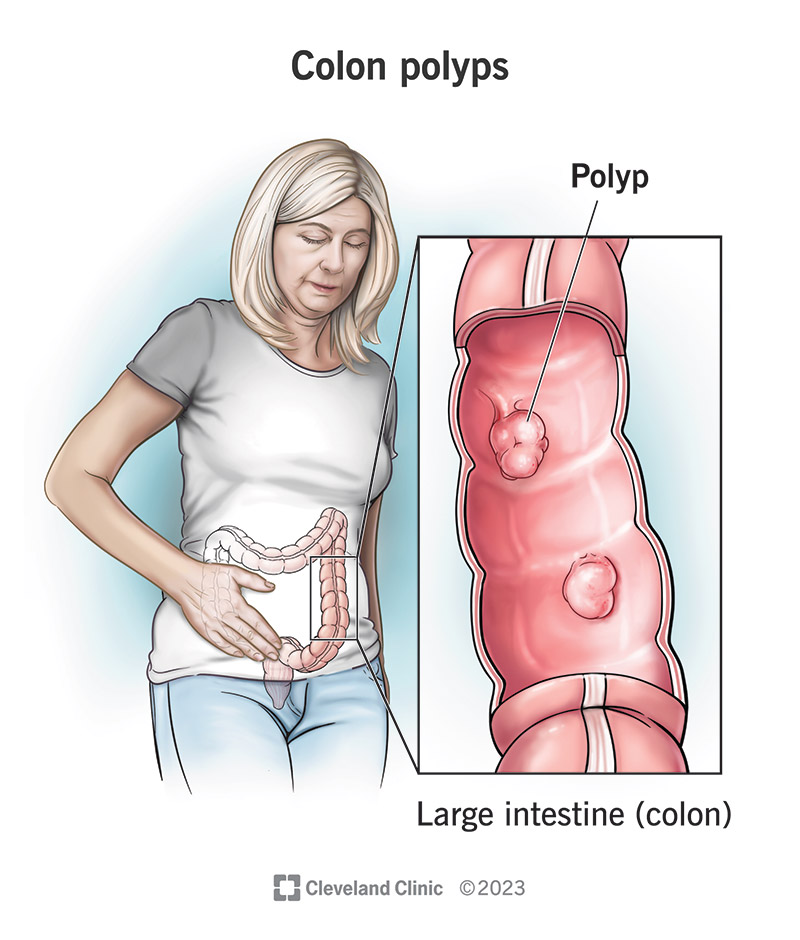
What distinguishes cancer-related changes is their persistence. A sudden onset of looser stools that lasts several weeks or new difficulty passing stools without an identifiable cause may signal that a mass is obstructing or interfering with normal bowel function. This is especially concerning if accompanied by other symptoms such as fatigue or abdominal pain. Persistent changes should always be evaluated with a colonoscopy or other diagnostic testing.
Symptom 2: Blood in the Stool or Rectal Bleeding
A Warning Sign Often Misattributed
Blood in the stool can appear as bright red streaks, dark maroon clots, or even black, tarry stools depending on where in the colon the bleeding occurs. Unfortunately, many women misattribute this symptom to hemorrhoids, menstruation, or minor gastrointestinal irritation and delay seeking medical help. The problem is particularly concerning in women over 40 or those with a family history of gastrointestinal cancers.
Microscopic bleeding may go unnoticed without testing. Iron-deficiency anemia caused by slow blood loss can be an early sign of colon cancer and often manifests as fatigue, pale skin, and lightheadedness. If blood is visibly present or suspected, further testing such as fecal occult blood testing or colonoscopy should not be postponed. “Is bowel leakage a sign of cancer” is also a symptom that can easily be confused with other intestinal disorders.
Symptom 3: Persistent Abdominal Discomfort or Pain
Differentiating Gas, Bloating, and Tumor Pressure
Abdominal pain is one of the most misinterpreted symptoms of colon cancer in women. Many women experience cyclical bloating, cramping, or discomfort related to menstruation or digestion, and may not recognize these as potential red flags. However, with colon cancer, the discomfort often becomes chronic, unresponsive to typical treatments, and increasingly localized to one side.
A growing tumor may produce feelings of pressure, fullness, or persistent bloating not related to meals or menstrual cycle. Unlike transient gas or indigestion, cancer-related abdominal discomfort does not resolve with antacids or dietary changes. It may worsen over time and become noticeable during sleep or after bowel movements.
Symptom 4: Unexplained Fatigue and Weakness
The Body’s Hidden Signal of Ongoing Blood Loss
Fatigue in women is often dismissed as a result of a busy lifestyle, poor sleep, or hormonal fluctuations. However, when fatigue becomes persistent, impacts daily function, and is accompanied by weakness or lightheadedness, it may point to something more serious. Colon cancer can cause chronic internal bleeding, which slowly depletes the body of iron, resulting in anemia.
This process occurs silently and can go undetected without blood tests. Iron-deficiency anemia in women—especially when not explained by menstruation or diet—should always prompt investigation of potential gastrointestinal blood loss. If fatigue is paired with paleness, shortness of breath, or a drop in exercise tolerance, further evaluation is critical.

Symptom 5: Unexplained Weight Loss
When the Body Burns Energy Without a Known Cause
Weight fluctuations are common in women, particularly around hormonal transitions, stress, or changes in diet and exercise. However, unintentional weight loss—especially when no change in routine or appetite can explain it—may be one of the clearest metabolic warnings of cancer. Colon tumors can alter how the body uses energy, increase inflammation, and disrupt digestion, all of which contribute to rapid, unhealthy weight loss.
This symptom may go unnoticed at first, especially if the individual welcomes the change or attributes it to increased activity. Over time, however, the lack of muscle mass, reduced appetite, and hollow facial features can become more pronounced. If a woman loses more than 5–10% of her body weight over a few months without explanation, a medical workup is essential to rule out cancer as a cause.

Symptom 6: A Feeling of Incomplete Evacuation After Bowel Movements
The Subtle Pressure That Signals Something’s Wrong
This symptom is often difficult to describe and is usually referred to by patients as a “feeling that something’s still there” after using the bathroom. It can result from a tumor partially blocking the rectum or colon, preventing complete passage of stool. The sensation may lead to repeated, unproductive trips to the toilet and persistent abdominal unease.
What makes this warning sign particularly deceptive in women is its similarity to symptoms of constipation, endometriosis, or pelvic organ prolapse. However, unlike those conditions, the sensation with colon cancer doesn’t improve with hydration, laxatives, or time. It lingers or worsens and may be accompanied by narrow stools or rectal discomfort. “When to euthanize a dog with cancer” — especially in terms of decision making when quality of life deteriorates gradually but irreversibly.
Symptom 7: Nausea and Vomiting Unrelated to Infection
A Gastrointestinal Blockage Warning
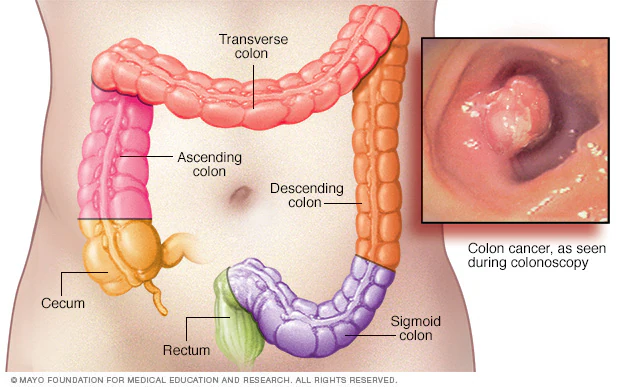
Nausea and vomiting are common symptoms of viral infections, pregnancy, or food intolerance. But in women with undiagnosed colon cancer, these can be signs of a physical blockage caused by tumor growth, especially if the mass is in the ascending or transverse colon. When waste cannot move freely through the intestines, the system backs up, resulting in nausea, vomiting, and sometimes severe abdominal pain.
The presence of vomiting, particularly when it occurs with constipation or bloating, may indicate a late-stage obstruction. This is a medical emergency. Unlike morning sickness or gastroenteritis, cancer-related nausea is often progressive and resistant to over-the-counter medications. It tends to appear later in the disease when the tumor has significantly reduced bowel lumen.
How These Symptoms Differ From Other Female Health Issues
Overlap with Menstrual, Hormonal, and GI Disorders
What makes colon cancer difficult to identify in women is the high degree of symptom overlap with other common conditions. Premenstrual syndrome, endometriosis, irritable bowel syndrome (IBS), ovarian cysts, and even menopause can all cause bloating, fatigue, irregular bowel habits, and abdominal discomfort. Without imaging or endoscopy, these overlapping signs can mask the presence of a growing malignancy.
Understanding the duration and progression of symptoms is key. Cancer-related changes tend to worsen with time and do not improve with rest, dietary changes, or menstrual cycle resolution. For example, if what seems like IBS fails to respond to probiotics, fiber, or stress reduction, further evaluation is necessary.
| Symptom | Common Explanation | Colon Cancer Warning Context |
| Constipation | Hormonal changes | Lasts several weeks; worsening stool pattern |
| Abdominal cramping | PMS or endometriosis | Daily pain, persistent, non-cyclical |
| Fatigue | Stress or anemia | Paired with blood loss or pale skin |
| Bloating | Menopause or food intolerance | Constant, unrelated to meals or cycle |
| Weight loss | Diet, thyroid | Rapid, unintentional, despite eating normally |
“Does botox cause cancer” is an example where fear and physiology need to be backed up by real medical data, not just feelings.
Importance of Early Detection in Women
Why Timing Affects Survival Rates
Colon cancer is one of the most treatable malignancies when caught early, with five-year survival rates exceeding 90% for localized disease. However, once it spreads to lymph nodes or distant organs, the outlook becomes far more serious. In women, delayed diagnosis is a critical issue, partly due to underestimating symptoms or attributing them to less serious conditions like hormonal fluctuations or IBS.
Routine screenings such as colonoscopy, beginning at age 45 or earlier for high-risk individuals, are the most effective tool for early detection. Women who notice persistent symptoms—even those that seem minor or embarrassing—should report them to a physician. Bloodwork, fecal occult blood testing, and imaging can often catch cancer before it advances. In many cases, removing a small polyp during a routine exam can prevent cancer altogether.
Gender-Specific Challenges in Diagnosing Colon Cancer
How Female Physiology and Social Norms Interfere
Biological and societal factors uniquely affect how colon cancer presents in women and how it is diagnosed. Anatomically, women may experience more diffuse symptoms due to a longer colon and pelvic structure that can displace the intestine, masking tumor-related discomfort. Hormonal changes from pregnancy, menopause, or birth control can alter bowel patterns, complicating symptom interpretation.
Socially, women are often more likely to downplay symptoms, prioritize the health of others over their own, or feel embarrassment discussing rectal bleeding or bowel changes. These delays can lead to diagnosis at a more advanced stage. There is also evidence that physicians may initially dismiss or misattribute women’s symptoms to anxiety or stress, reinforcing underdiagnosis in the early phase of disease.
Risk Factors Specific to Women
Conditions and Lifestyle Factors That Increase Likelihood
Certain risk factors for colon cancer affect both sexes, but some are more common or more impactful in women. These include:
– A family history of colon or ovarian cancer
– Long-term use of hormone replacement therapy (HRT)
– A history of breast cancer or endometrial cancer
– Sedentary lifestyle combined with poor dietary fiber intake
– Type 2 diabetes or metabolic syndrome
Unlike men, women may also face unique risks during and after pregnancy, particularly if digestive changes persist or if gestational diabetes occurs. Chronic inflammation from endometriosis or pelvic surgeries may also increase risk by altering gut environment. While none of these guarantee cancer development, their presence warrants a lower threshold for screening.
When to Talk to Your Doctor
Thresholds for Medical Evaluation
The key factor for determining when to see a physician is persistence. If any of the symptoms discussed—especially changes in bowel habits, blood in stool, or unexplained fatigue—last more than two weeks, they should be reported. Waiting for symptoms to resolve on their own can allow progression to a more advanced stage.
Doctors typically begin with a physical exam and blood tests, followed by stool sample tests or imaging if needed. A colonoscopy remains the gold standard, as it allows direct visualization and biopsy of any suspicious lesions. For women under 50 experiencing unexplained gastrointestinal symptoms, early evaluation is even more crucial, as incidence is rising in younger populations.
Misdiagnosis and Delayed Diagnosis in Women
The Cost of Being Told “It’s Just Stress”
Many women report that initial visits for colon cancer-related symptoms result in reassurance or misdiagnosis. They are often told their problems stem from anxiety, diet, menstruation, or irritable bowel syndrome. While these may indeed be factors, the danger lies in assuming benign causes without further investigation. Studies confirm that women, especially under 50, are more likely than men to have their gastrointestinal symptoms initially dismissed.
Misdiagnosis delays treatment, allowing tumors to grow and spread. What might have been a treatable, early-stage lesion can progress into an invasive cancer with limited therapeutic options. This is why persistence in seeking answers—and trusting one’s instincts when symptoms do not improve—is critical for early intervention and survival.
Diagnostic Tools and Screening Recommendations
Methods Used to Confirm or Rule Out Colon Cancer
When symptoms suggest potential colon malignancy, clinicians rely on a range of diagnostic tools to determine the cause. Blood tests, including complete blood count and iron levels, may reveal anemia due to internal bleeding. Stool tests such as fecal occult blood test (FOBT) or fecal immunochemical test (FIT) detect hidden blood in feces.
The most definitive diagnostic tool remains the colonoscopy. This allows direct visualization of the entire colon and rectum, removal of polyps, and biopsy of suspicious areas. In some cases, imaging such as CT colonography or MRI may be used. For women with incomplete colonoscopies or structural abnormalities, capsule endoscopy offers a non-invasive alternative.
Prognosis and Survival Outlook
Why Early Detection Makes a Dramatic Difference
The prognosis of colon cancer depends almost entirely on the stage at diagnosis. If caught early, before the cancer has penetrated the colon wall or spread to lymph nodes, five-year survival rates are high. Once metastasis occurs, especially to the liver or lungs, the outlook becomes significantly worse.
Women often face unique challenges that influence prognosis, including delayed recognition of symptoms, under-screening, and coexisting gynecological issues. However, when cancer is identified early and removed surgically, many women go on to live full, healthy lives. Advances in chemotherapy, immunotherapy, and targeted agents continue to improve outcomes even in later stages.
Prevention and Lifestyle Measures
Reducing Risk Through Proactive Choices
While not all cases of colon cancer can be prevented, many risk factors are modifiable. A fiber-rich diet, low in processed red meats and high in vegetables and whole grains, supports a healthier colon environment. Regular physical activity improves digestion and reduces inflammation. Avoiding tobacco and limiting alcohol consumption also lowers risk.
Women should pay special attention to screening guidelines. Starting at age 45 (or earlier if at higher risk), colonoscopies or non-invasive stool-based tests should be done regularly. Knowing family history, managing body weight, and addressing gastrointestinal symptoms early are essential steps in prevention.
FAQ: 7 Symptoms of Colon Cancer in Women
What makes colon cancer symptoms different in women?
Women often have subtler symptoms that overlap with menstrual or hormonal issues, making early detection more difficult.
Can colon cancer cause bloating like PMS?
Yes, bloating from colon cancer tends to be persistent and not linked to menstrual cycles or food intake.
Is fatigue an early sign of colon cancer in women?
Fatigue caused by anemia due to internal bleeding is a common early warning sign, especially if unexplained.
How can I tell if constipation is serious?
If constipation lasts more than two weeks and doesn’t respond to diet or hydration, it could be a symptom of a larger issue.
What kind of bleeding is concerning?
Bright red or dark blood in the stool, or black tar-like stools, should always be evaluated—especially outside of menstruation.











