Colon Cancer and Stomach Noises: Key Facts
- Foreword
- 1. Understanding Stomach Noises (Borborygmi)
- 2. What is colon cancer, exactly?
- 3. Symptoms of Colon Cancer
- 4. The Link Between Stomach Noises and Colon Cancer
- 5. Other Conditions That Cause Stomach Noises
- 6. Diagnostic Approaches
- 7. Treatment Options for Colon Cancer
- 8. Preventive Measures and Lifestyle Modifications
- 9. Emerging Research and Technologies
- 11. Frequently Asked Questions (FAQs)
- Closing Thoughts
Foreword
If your stomach’s been growling more than usual—or making unexpected gurgles at odd times—you’re not alone. These audible rumbles, medically known as borborygmi, are a normal part of digestion. But what happens when they feel louder, more frequent, or oddly timed? Could these gut sounds ever hint at something serious—say, even something as significant as colon cancer?
That question, while unsettling, is not as outlandish as it might seem. Most of us were taught to tune out digestive noises unless they become socially inconvenient. But sometimes, the body’s whispers—or in this case, grumbles—are trying to tell us something. In recent years, there’s been growing attention on how subtle gastrointestinal signals, such as changes in bowel sounds, might reflect deeper underlying conditions.
This article is designed to serve as your final stop on this topic. Whether you’re someone experiencing unusual stomach noises, a caregiver trying to understand a loved one’s symptoms, or a health enthusiast digging deep into the intersections of digestive function and colorectal health—you’re in the right place. We’ll explore every angle: the physiology of those rumbles, the red flags that might point to colon cancer, what the current science says, and what it doesn’t yet understand.
Most importantly, this isn’t about causing alarm. It’s about decoding your body’s messages with clarity and confidence.
Let’s begin with the fundamentals.
Understanding Stomach Noises (Borborygmi)
What exactly are those noises coming from your stomach, and why do you hear them? When your stomach growls, you’re hearing the sounds of your digestive tract in action. These noises arise from the movement of gas and fluid through the stomach and small intestines, driven by rhythmic muscular contractions called peristalsis that propel food along your digestive system.

Usually, these sounds are louder when your stomach is empty because there’s less food to muffle the movement of gas and fluids. That classic “hungry stomach growl” is a familiar example. But these noises can also occur after eating, during digestion, or even when you’re anxious. So while stomach noises are normal, they’re far from meaningless.
You might wonder: when should I be concerned about stomach noises? Not every loud gurgle signals trouble. But if the noises become noticeably louder, more frequent, or come with other symptoms like pain, bloating, or changes in bowel habits, it’s worth paying attention.
There’s also a difference between noises originating higher up in the digestive tract—such as the stomach or small intestine—and those from the colon lower down. Upper digestive noises tend to be higher-pitched and occur soon after eating, while noises from the colon may sound deeper and often accompany sensations of fullness or pressure. If you notice persistent low abdominal noises along with discomfort or irregular bowel movements, it could be an important clue.
You might be wondering why we’re focusing on stomach noises when talking about colon cancer. That’s an insightful question. While colon cancer doesn’t typically cause stomach noises on its own, it can interfere with normal gut motility, especially if a tumor partially blocks the colon. This blockage can alter how gas and waste move, producing abnormal or louder noises. It’s not the most common sign, but in combination with other symptoms, it shouldn’t be ignored.
Should you start listening more closely to your gut? Not obsessively, but yes—with awareness. Your gut is a complex and finely tuned system. When something’s off, it often signals it through changes in patterns—recurring noises, altered rhythms, or unusual sensations. Knowing what’s normal for you helps you recognize when something isn’t.
In summary, stomach noises are usually just the background music of your digestion. But when the tune changes—or plays out of sync with your usual rhythms—it’s worth tuning in. Next, we’ll take a closer look at colon cancer itself: what it is, who’s at risk, and why early detection is so critical.
What is colon cancer, exactly?
Colon cancer—often grouped with rectal cancer under the term colorectal cancer—is more common than many realize. It ranks among the most frequently diagnosed cancers worldwide. Yet despite its prevalence, colon cancer has a troubling habit of developing silently, often without obvious symptoms in its early stages. This stealthy progression raises two critical questions: how does such a serious disease manage to go unnoticed for so long, and why is early detection so vital?

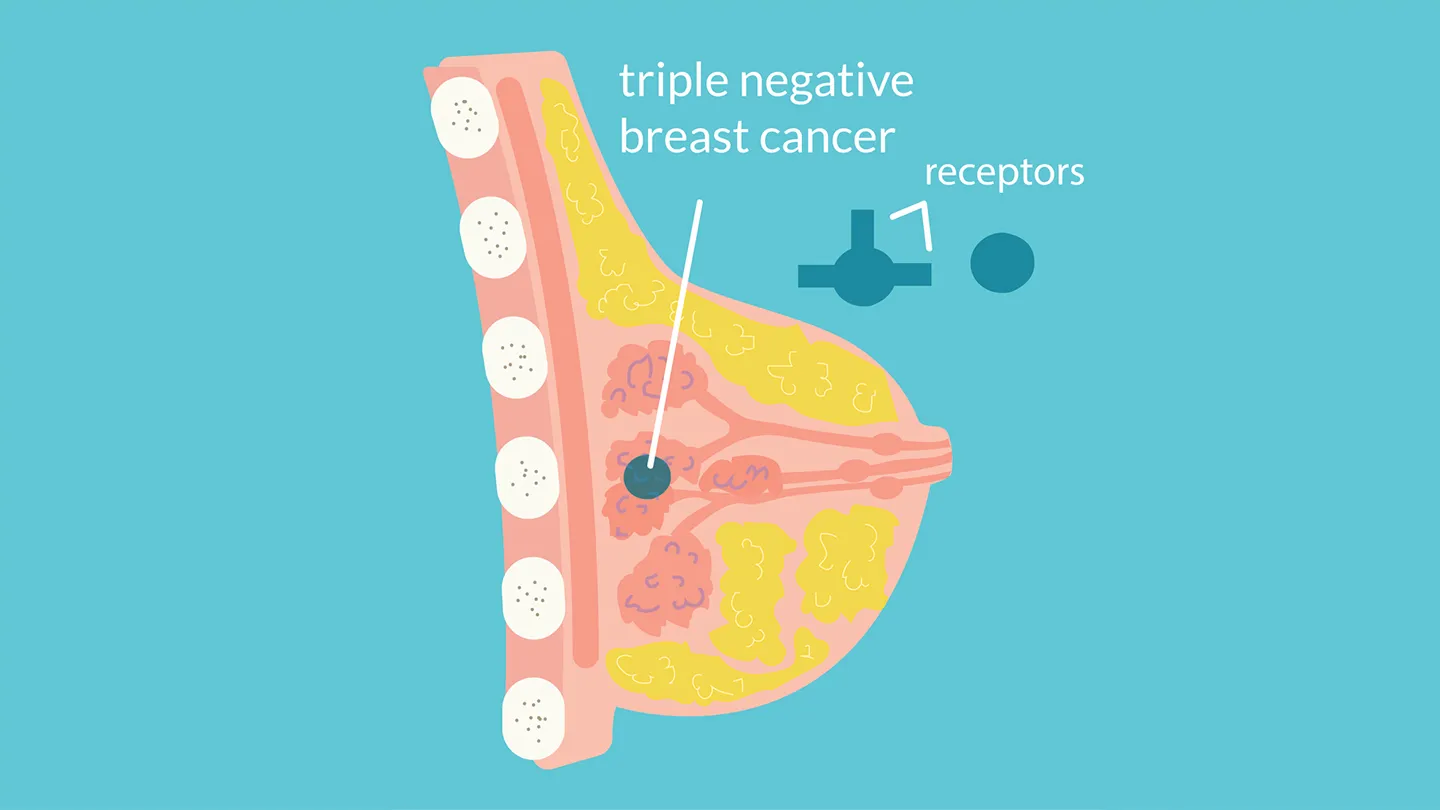
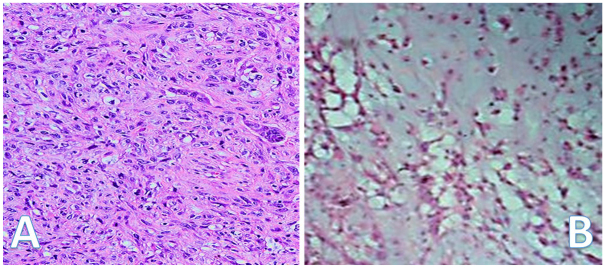
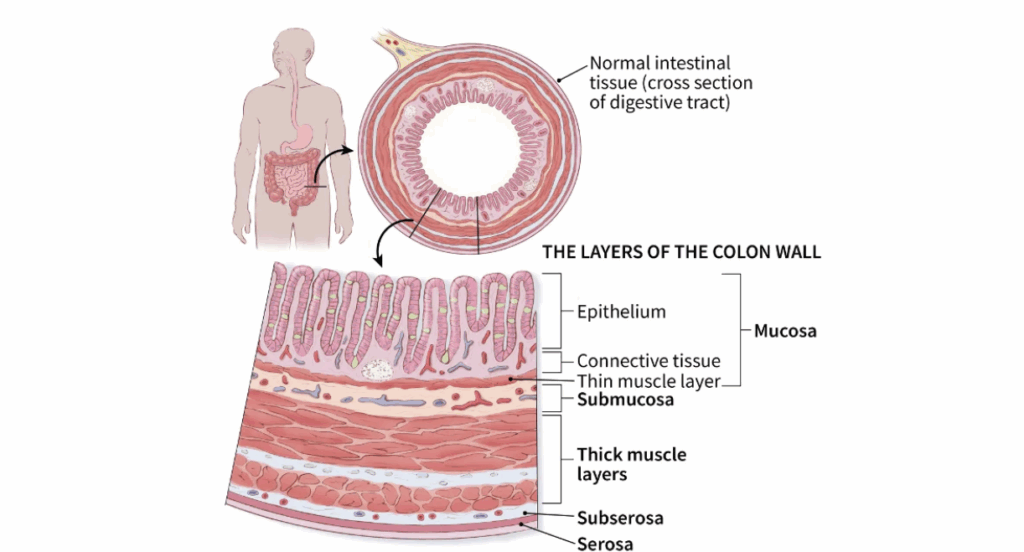
At its core, colon cancer is a malignant growth that originates in the inner lining of the large intestine, the part of your digestive system responsible for absorbing water and forming stool. Most colon cancers begin as small, benign growths called polyps—tiny clusters of cells that look somewhat like skin tags inside the colon. While many polyps remain harmless, some undergo genetic changes over several years, eventually turning into cancer.
The process is slow, often spanning a decade or more from a normal colon lining to invasive cancer. This lengthy timeline, although alarming, offers a valuable window for early detection and prevention.
You might ask, “Why do some people develop colon cancer while others don’t?” The answer lies in a mix of genetics, lifestyle, and environmental factors.
Age is a significant risk factor. Colon cancer traditionally affects people over 50, but recent trends show an unsettling increase in younger adults, even those in their 30s. The reasons aren’t fully understood, but diet, sedentary lifestyle, microbiome changes, and environmental exposures likely play a role.
Family history also matters. Having a close relative diagnosed with colon cancer, especially at a young age, raises your risk. Certain inherited genetic conditions, such as Lynch syndrome or familial adenomatous polyposis (FAP), dramatically increase susceptibility but are often under-recognized.
Lifestyle factors wield considerable influence too. Diets low in fiber and high in red or processed meats, excessive alcohol consumption, smoking, and obesity all elevate colon cancer risk. The encouraging news is that many of these are modifiable—you have some control here.
Another fascinating area of emerging research is the gut microbiome—the vast community of bacteria living in your intestines. Some microbes protect your colon lining and reduce inflammation, while others may promote tumor growth through toxic byproducts. Scientists are still unraveling this complex ecosystem, but it’s becoming clear that a healthy microbiome might be a powerful ally in cancer prevention and treatment.
You might wonder why colon cancer, developing in such a vital digestive organ, often causes so few early symptoms. The truth is the colon is quite resilient and flexible. It can stretch, reroute, and compensate for slow-growing tumors, which means early-stage cancers frequently cause no noticeable issues.
When symptoms do arise, they’re often subtle—minor changes in bowel habits, occasional abdominal discomfort, or unexplained fatigue—that can easily be mistaken for less serious problems or the effects of aging.
This subtlety is precisely why colon cancer can be so dangerous; it silently advances until symptoms become more obvious and the disease more advanced.
You may be curious whether stomach noises could be an early warning sign. Usually, they’re not. But when a tumor grows large enough to partially block the colon, it can change how gas and waste move, leading to altered or increased bowel sounds. These noises won’t appear in isolation—they’ll typically be accompanied by other symptoms such as cramping, constipation, or changes in stool consistency.
Finally, it’s crucial to understand why early detection saves lives. When colon cancer is found while still confined to the colon, treatment success rates are very high—five-year survival can exceed 90%. However, once cancer spreads to distant organs, survival rates drop significantly.
Because early colon cancer rarely causes symptoms, routine screening—especially colonoscopy—is vital. Colonoscopy not only detects cancer but can prevent it by removing precancerous polyps before they turn malignant.
While loud stomach noises alone don’t ring alarm bells for colon cancer, if you experience unusual gut sounds alongside other symptoms or risk factors, it’s wise to seek medical evaluation. In the next section, we’ll dive deeper into what colon cancer symptoms actually feel like and how to distinguish them from common digestive issues.
Stomach activity is rarely the first thing we associate with colon cancer, but it’s surprising how many people miss subtler signs. You might also want to skim Early Symptoms of Colon Cancer for a broader picture.
Symptoms of Colon Cancer
You might be surprised to learn that colon cancer doesn’t often announce itself with drama. There’s no sudden collapse, no flashing pain to send you running to the ER. More often than not, it slips under the radar—subtle, persistent, and easily mistaken for “just aging,” a “weird diet week,” or “maybe I’m just stressed.”
That’s why understanding the texture of its symptoms—not just listing them—is essential. You need to know what these signs feel like in real life.
So what does colon cancer actually feel like?
Let’s talk in real terms. If you had colon cancer developing right now, you might feel totally fine for months. Maybe even years. But as it grows, the tumor can start to affect how things move through your colon. That’s when things begin to shift—slowly, then noticeably.
Here’s what to look for:
1. Changes in bowel habits
This is one of the most consistent red flags, but it’s frustratingly vague. What does “change” even mean?
It could mean:
- You used to go once a day like clockwork, and now it’s every other day—or three times a day.
- You’re suddenly more constipated or looser than normal.
- Your stool has narrowed or flattened (sometimes described as “pencil-thin”).
- You feel like you didn’t finish the job, no matter how many times you go.
But doesn’t everyone experience that sometimes? Absolutely. But colon cancer doesn’t cause one-off changes—it causes persistent ones. If these changes linger for more than a few weeks, especially if they’re accompanied by other symptoms, your doctor needs to hear about them.
2. Blood in the stool or rectal bleeding
Blood—especially if it’s bright red—tends to trigger concern. But what about darker blood? What about blood you can’tsee?
Here’s the truth: some colorectal cancers bleed slowly and invisibly, which leads to low-level blood loss over time. That kind of bleeding may not show up in the toilet bowl, but it can manifest as iron-deficiency anemia—something you might only discover through routine blood work.
Still, any visible blood—bright red on the tissue or mixed into the stool—should be investigated. Yes, it could be hemorrhoids. Yes, it could be an anal fissure. But assuming it’s only that, without ruling out more serious causes, is how people miss early-stage cancer.
3. Abdominal discomfort, cramping, or bloating
Another maddeningly vague symptom, right? Everyone gets bloated sometimes. But here’s the distinction: cancer-related abdominal discomfort tends to be persistent, poorly relieved by passing gas or going to the bathroom, and often hard to localize.
It’s not “food baby” bloating. It’s “something feels off, almost stuck” bloating. Often, it’s paired with changes in bowel patterns and a sense that your gut has become unpredictable.
4. Fatigue and unexplained weight loss
Cancer is a metabolically active process—it burns energy, even while you rest. And if you’re losing blood through the GI tract, you may become anemic, which compounds the fatigue.
The kind of tiredness people describe isn’t just “I need more sleep.” It’s a body-deep heaviness, a sense of dragging through the day no matter how much rest you get.
Unexplained weight loss—especially if you haven’t changed your eating or exercise habits—is another flag. Again, on its own, it’s not diagnostic. But in context? It adds weight to the picture.
5. Nausea and vomiting (especially if recurrent)
If a tumor starts to cause a partial obstruction in your colon, waste can back up. That can trigger nausea, appetite loss, or even vomiting. This usually happens later in the disease course, but it’s worth understanding how a mechanical problem in the colon can cause systemic symptoms.
And yes—obstructions can also cause more audible bowel sounds, which brings us back to our theme of stomach noises. If something is physically impeding normal flow, your intestines may become noisier as they struggle to push contents through.
How can you tell if symptoms are colon cancer—or something less serious?
That’s the billion-dollar question. And here’s the honest answer: you can’t always tell, not without proper testing. But patterns matter. Duration matters. Context matters.
Ask yourself:
- Has this been going on for more than a few weeks?
- Is this different from my usual “digestive hiccups”?
- Are there multiple symptoms clustering together?
- Do I have risk factors (age, family history, diet, smoking)?
If you’re nodding to more than one of these, it’s not paranoia—it’s prudence—to get checked.
What about people with IBS or IBD—should they be more worried?
Yes, and no. People with irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD) often live with chronic gut symptoms. That makes it trickier to detect a new pattern, but not impossible.
Here’s the trick: if your “usual” changes—either in intensity, frequency, or character—it’s worth a re-evaluation. Long-term IBD (especially ulcerative colitis and Crohn’s colitis) does increase colon cancer risk, so regular surveillance colonoscopies are a must.
For IBS patients, the risk isn’t significantly higher than the general population. But new bleeding, anemia, or weight loss should never be written off as “just IBS.”
Can colon cancer symptoms really be that silent?
Yes. And that’s precisely what makes awareness so powerful. If we only react to big symptoms, we’re often reacting too late. But if we’re attuned to patterns, if we notice the quieter shifts—the low hum of fatigue, the new bathroom routine, the gut that “feels off”—we give ourselves a head start.
—
Next, we’ll bring it all together: what happens when stomach noises intersect with this symptom landscape? Is there a physiological link, or are we just drawing lines where none exist? Spoiler: it’s more complicated—and more fascinating—than you might think. Let’s keep going.
The Link Between Stomach Noises and Colon Cancer
You might be wondering, “We’ve talked a lot about colon cancer symptoms and stomach noises separately—but what’s the real connection between these gut sounds and colon cancer?” It’s a great question because the relationship isn’t straightforward, but understanding it sheds light on how your body communicates when something is amiss.
First, it’s important to clarify: colon cancer does not typically announce itself with stomach noises alone. Those rumbles and gurgles you hear are almost always normal digestive sounds. But under certain conditions, colon cancer can influence these sounds by disrupting how your intestines work.
One of the main ways this happens is through a partial blockage in the colon. Imagine the colon as a garden hose, and the tumor as a pebble lodged inside. It may not block the flow completely, but it creates resistance. Your intestines respond by contracting more vigorously or erratically to push contents past the narrowing. These stronger or more frequent contractions can produce louder or unusual bowel sounds.
If you think about it, this makes sense—when you’re straining to push food, gas, or waste through a tight spot, the movement becomes noisier. However, partial obstruction doesn’t just cause noise; it usually brings along other symptoms such as bloating, cramping, constipation, or alternating diarrhea.
Another factor is the gut microbiome. Your colon is home to trillions of bacteria that ferment undigested food, producing gas and various byproducts. Colon cancer can change the local environment and bacterial balance, potentially increasing fermentation and gas production. This can lead to more audible stomach noises and bloating.
You might ask, “Can I tell the difference between ‘normal’ noisy digestion and something caused by cancer?” The honest answer is, not really—at least not without medical help. There’s no unique “cancer noise” signature. But what you can do is notice changes over time. Are your stomach sounds louder than usual? Happening more often? Accompanied by discomfort or other concerning symptoms?
It’s also key to remember that many other common conditions cause loud or irregular stomach noises—things like irritable bowel syndrome (IBS), infections, food intolerances, and small intestinal bacterial overgrowth (SIBO). Most of the time, these benign causes are far more likely than colon cancer.
So when should stomach noises raise a red flag? If your gut sounds are new, persistent, louder, and come with other symptoms like blood in stool, persistent abdominal pain, weight loss, or a family history of colon cancer, it’s time to seek evaluation.
There’s an exciting horizon here, too. Researchers are working on technology that could “listen” to your gut with sensors and analyze patterns of sounds to detect abnormalities early. While this is still experimental, it highlights how your body’s noises may one day become an important diagnostic tool.
In summary, stomach noises alone rarely indicate colon cancer, but when paired with other symptoms and risk factors, they become part of a larger story worth paying attention to. Next, we’ll broaden our view and look at other conditions that commonly cause stomach noises and how they compare.
Other Conditions That Cause Stomach Noises
By now, you’re probably thinking: If stomach noises can sometimes be linked to colon cancer, but most of the time they’re not—what else could be causing these sounds? That’s an excellent question because it gets to the heart of how complex and noisy our digestive systems really are.
If you’re worried about overlapping GI symptoms, there’s an insightful comparison in Colorectal Cancer vs IBS.
The truth is, stomach noises are a symptom—not a diagnosis. They’re the audible signal of a lot of different processes happening in your gut. Most of those processes are completely benign or related to less serious conditions. But some can mimic colon cancer symptoms, making the clinical picture tricky. Let’s explore the usual suspects, so you can understand what might be going on if cancer is unlikely.
1. Irritable Bowel Syndrome (IBS)
IBS is arguably the most common functional bowel disorder—meaning your gut isn’t structurally damaged but behaves abnormally. If your digestive tract was an orchestra, IBS would be the section that’s a bit out of sync. You’ll experience symptoms like abdominal cramping, bloating, diarrhea, or constipation—and yes, often loud, irregular stomach noises.
Why do noises increase with IBS? It’s because the muscles in the intestines can contract more frequently or erratically, causing more pronounced movement of gas and fluid. Stress and certain foods (think caffeine, fatty meals, or FODMAPs) often worsen symptoms.
Question to ponder: If you already have IBS, how can you tell if your symptoms are evolving or if something new is happening?
The answer lies in change. If you suddenly notice blood in your stool, unexplained weight loss, or persistent severe pain, it’s time to reassess. IBS itself doesn’t cause bleeding or weight loss.
2. Inflammatory Bowel Disease (IBD)
Unlike IBS, IBD refers to actual inflammation in the digestive tract, which includes Crohn’s disease and ulcerative colitis. Both can cause increased stomach noises due to inflammation-driven motility changes, strictures (narrowing), and ulcerations.
These diseases often present with more severe symptoms—persistent diarrhea (sometimes bloody), abdominal pain, and systemic signs like fever or weight loss. Importantly, long-standing IBD increases the risk of colon cancer, which is why regular surveillance is critical.
3. Food Intolerances and Malabsorption
Ever notice your stomach grumble after eating certain foods? If you’re lactose intolerant, your body lacks the enzyme lactase needed to digest lactose, leading to fermentation of undigested sugars by gut bacteria. This produces excess gas and, consequently, louder stomach noises.
Similarly, conditions like celiac disease cause damage to your small intestine lining, impairing nutrient absorption and leading to bloating, cramping, and noisy digestion.
Curious: Can changing your diet reduce stomach noises?
Often, yes. Avoiding trigger foods or following an elimination diet can make a big difference. But beware: if your noises come with other concerning symptoms, diet changes alone aren’t enough.
4. Gastrointestinal Infections
Stomach bugs, whether viral or bacterial, can temporarily ramp up gut motility and increase gas production. During the acute phase, it’s common to hear louder stomach noises, often accompanied by diarrhea, nausea, and cramping.
If symptoms persist beyond a few days, or if you develop blood in your stool or severe pain, it’s time to seek medical attention.
5. Small Intestinal Bacterial Overgrowth (SIBO)
SIBO is a condition where bacteria that normally live in the colon start to overpopulate the small intestine. This leads to excessive fermentation and gas production earlier than usual in the digestive tract, often causing loud stomach noises, bloating, diarrhea, or constipation.
Diagnosis typically requires specialized breath tests, and treatment involves antibiotics or probiotics.
6. Mechanical Causes (Obstruction, Adhesions)
Apart from cancer, other physical causes can partially block the intestines—like scar tissue (adhesions) from prior surgeries, hernias, or strictures from inflammation. These can cause loud stomach noises as the intestines struggle to push contents through narrow spots.
What should you do if your stomach noises are loud and persistent, but you don’t have cancer?
This is where a good relationship with your healthcare provider is key. A thorough history and physical exam, combined with selective testing, can help zero in on the culprit.
Sometimes, the best first step is a detailed symptom diary—note what you eat, when noises happen, what other symptoms appear, and how your body feels overall. This context helps your doctor make sense of the noise and prioritize investigations.
Why don’t doctors take stomach noises more seriously?
Because, in isolation, they rarely indicate serious disease. The challenge lies in distinguishing normal gut sounds from those that are clinically significant. That’s why patterns and accompanying symptoms are so important.
Listening to your gut literally is a powerful tool—but only when paired with informed interpretation.
Diagnostic Approaches
So, you’ve been paying attention to your body—maybe noticing stomach noises that feel different, or other subtle symptoms that don’t quite add up. The big question now is: how do you and your healthcare provider move from uncertainty to clarity? How do we figure out what’s really going on inside that noisy gut?
Diagnosis of digestive issues—and especially colon cancer—is rarely a straightforward, single-step process. Instead, it’s a carefully layered approach, designed to piece together clues from your history, symptoms, and a variety of tests. Each step builds on the last to create a clearer picture.
It all begins with a thorough medical history and physical exam. Your doctor will want to know the details: when the noises happen, how often, their character, and any associated symptoms like changes in bowel habits, bleeding, pain, or fatigue. They’ll also ask about your family history, lifestyle, diet, and any medications you’re taking. This foundational information helps prioritize the next steps.
From there, simple blood tests often come first. These can reveal anemia—low red blood cell counts—which might suggest hidden bleeding in the digestive tract. Markers of inflammation or infection may also be checked. While these blood tests aren’t definitive on their own, they guide further investigation.
Stool tests are another important tool. They can detect occult (hidden) blood that you wouldn’t see visually but might signal a problem in the colon. Stool studies may also screen for infections or other abnormalities.
When warranted, your doctor will recommend a colonoscopy. This is considered the gold standard for detecting colon cancer and precancerous lesions. A colonoscopy involves inserting a flexible tube with a camera into your colon to directly visualize the lining and take biopsies if needed. It’s not a casual procedure, but it’s invaluable because it not only diagnoses cancer but can also prevent it by removing suspicious polyps.
Imaging studies, like CT scans or ultrasounds, might be ordered if symptoms suggest complications such as obstruction or if cancer spread is suspected. CT scans provide detailed pictures of abdominal organs and can detect masses or lymph node involvement, complementing what colonoscopy shows.
It’s worth noting that no test can directly measure or diagnose the cause of abnormal stomach noises. However, these tests uncover the underlying conditions—like tumors, inflammation, or infections—that may be responsible.
Sometimes, despite all testing, results come back normal, yet symptoms persist. This scenario is common in functional disorders like irritable bowel syndrome (IBS). In such cases, diagnosis is often one of exclusion, and the focus shifts toward symptom management. Specialized testing like breath tests for bacterial overgrowth or motility studies might be pursued.
You might wonder how to prepare for a medical evaluation to make it as effective as possible. Keeping a symptom diary—tracking when noises and other symptoms occur, your diet, and lifestyle factors—can be invaluable. It helps your doctor connect dots that might otherwise seem disconnected.
In essence, diagnosing what lies behind your stomach noises and symptoms is a stepwise process combining your story with targeted testing. This approach ensures that serious causes like colon cancer are not missed while avoiding unnecessary invasive procedures.
Next, we’ll explore treatment options should colon cancer be diagnosed, detailing what to expect and how care is tailored to individual needs.
Treatment Options for Colon Cancer
So, the tough question: what if the diagnosis comes back positive for colon cancer? It’s normal to feel a wave of emotions—shock, fear, confusion. But here’s something every patient, caregiver, or curious reader needs to know right away: colon cancer today is one of the most treatable cancers, especially when caught early.
Let’s walk through the treatment landscape, break down the options, and unpack what you might realistically expect if you—or someone you care about—faces this diagnosis.
How is colon cancer treated?
Treatment depends on several factors: the stage of the cancer, its exact location in the colon, your overall health, and sometimes genetic markers of the tumor. The most common treatment modalities include surgery, chemotherapy, radiation, and newer targeted therapies.
Let’s take these one by one.
1. Surgery: The cornerstone of cure
For most people with colon cancer, surgery is the first and most important step. The goal? Remove the tumor and any nearby lymph nodes that might harbor cancer cells.
You might wonder: Is the entire colon removed? Not necessarily. Surgeons usually remove only the affected segment—a procedure called a colectomy. Depending on the tumor’s location, this could mean removing part of the ascending, transverse, descending, or sigmoid colon.
Sometimes, temporary or permanent colostomies are necessary, where the bowel is diverted through an opening in the abdomen to allow stool to exit into a bag. This can sound intimidating, but it’s often temporary and manageable with good support.
2. Chemotherapy: Cleaning up the microscopic leftovers
After surgery, some patients receive chemotherapy. Think of chemo as a mop cleaning up tiny cancer cells that might have escaped the surgeon’s scalpel. It’s systemic treatment—meaning it travels through your bloodstream to reach cancer cells anywhere in the body.
Not everyone needs chemotherapy. It’s usually recommended for more advanced stages or if there are high-risk features on pathology. Side effects vary, but modern regimens are increasingly tolerable, and oncologists tailor treatments to minimize impact on quality of life.
3. Radiation Therapy: Precision targeting
Radiation isn’t commonly used for colon cancer the way it is for rectal cancer, but there are exceptions. For tumors that are hard to remove surgically or that have spread locally, radiation can help shrink the tumor or alleviate symptoms.
It’s a local treatment, targeting a specific area rather than the whole body. Side effects might include fatigue or skin irritation but are usually temporary.
4. Targeted and Immunotherapies: The new frontier
This is where cancer treatment is evolving fast. Targeted therapies are drugs designed to interfere with specific molecules involved in tumor growth. Immunotherapy works by boosting your immune system’s ability to recognize and attack cancer cells.
Not all colon cancers respond to these treatments, but for those with certain genetic markers, they can be game-changers.
What about lifestyle during treatment? Can diet, exercise, or supplements help?
Great question. While treatment focuses on eradicating cancer, lifestyle factors can support your body’s resilience.
- Nutrition: Eating balanced meals tailored to your tolerance and preferences helps maintain strength and healing.
- Physical activity: Light to moderate exercise improves energy and mood, reduces fatigue, and can aid recovery.
- Mental health: Emotional support, counseling, and community connections are vital.
Supplements? Some can interact with treatment, so always check with your care team before starting anything new.
How long does treatment last?
This varies widely. Surgery recovery might take weeks; chemotherapy cycles often last several months; targeted therapies can be ongoing. Your care team will guide you with a personalized timeline.
What about prognosis?
Prognosis depends heavily on stage at diagnosis. Early-stage colon cancer has an excellent outlook, with five-year survival rates above 90%. Advanced cancers require more complex treatment and carry a more guarded prognosis, but even then, new therapies are improving outcomes steadily.
Can colon cancer come back after treatment?
Recurrence is a reality for some patients, which is why regular follow-up care is critical. This includes periodic scans, blood tests (like carcinoembryonic antigen or CEA), and colonoscopies.
The good news: early detection of recurrence often means it can be treated effectively.
Should I get a second opinion?
Absolutely. Colon cancer treatment is a big deal, and a second opinion from a colorectal cancer specialist or a multidisciplinary team can provide reassurance, alternative options, or access to clinical trials.
And for later-stage progression, Colon Cancer Metastasis to the Peritoneum walks through what complications can look like when things move beyond digestion alone.
Preventive Measures and Lifestyle Modifications
Now that we’ve covered diagnosis and treatment, let’s pivot to a question that’s on many mindsHaving covered diagnosis and treatment, it’s natural to ask: what can you do to prevent colon cancer in the first place? Or, if you’ve already faced this disease, how can you reduce the risk of it coming back? The encouraging truth is that while some risk factors—like genetics—are beyond your control, a significant portion can be influenced by your lifestyle choices. These changes not only lower your cancer risk but also enhance your overall health.
Prevention is crucial because colon cancer usually develops slowly, often over years or decades. This long window offers ample opportunity to intervene before cancer even starts or catches it in its earliest, most treatable stages. Prevention, therefore, isn’t just about avoiding cancer; it’s about maintaining a healthy, resilient gut and body.
One of the most powerful prevention strategies is diet. Consistently eating a diet high in fiber—rich in fruits, vegetables, and whole grains—helps move waste efficiently through the colon, reducing the time harmful substances contact the colon lining. Conversely, diets heavy in red and processed meats, especially when cooked at high temperatures, have been linked to increased colon cancer risk due to the formation of carcinogenic compounds.
Limiting alcohol intake and avoiding smoking are equally important. These substances not only raise the risk for colon cancer but affect multiple aspects of health.
Exercise also plays a key role. Regular physical activity doesn’t just help maintain a healthy weight—it improves gut motility, lowers inflammation, and boosts immune function, all factors that contribute to reducing cancer risk. Even moderate, consistent movement like walking or cycling can be beneficial.
Maintaining a healthy weight is another cornerstone. Excess body fat produces hormones and inflammatory molecules that can promote tumor growth and progression, so managing weight through diet and exercise supports prevention.
Of course, lifestyle changes are only part of the picture. Screening is an essential pillar of prevention. Starting at age 45—or earlier for those with family history or other risk factors—regular colon cancer screening, primarily with colonoscopy or stool-based tests, is vital. These screenings detect and allow removal of precancerous polyps before they turn malignant, significantly reducing cancer incidence and mortality.
If you’ve already had colon cancer, prevention shifts toward survivorship care. This includes adhering to follow-up screening schedules, maintaining healthy habits to reduce recurrence risk, managing treatment side effects, and supporting emotional well-being. Research shows that lifestyle improvements after treatment can enhance outcomes and quality of life.
You might wonder about supplements. While calcium, vitamin D, and aspirin have been studied for possible protective effects, evidence is mixed, and these should never replace healthy lifestyle choices or screening. Moreover, supplements can interact with medications, so always consult your healthcare provider before starting any.
Interestingly, many preventive lifestyle habits—such as eating a high-fiber diet and exercising regularly—also help normalize gut motility and reduce abnormal stomach noises. So the very steps that lower your cancer risk may also improve the digestive symptoms that initially concerned you.
In the end, prevention isn’t about perfection; it’s about small, consistent steps. Over time, these choices build resilience, reduce risk, and help your digestive system function smoothly—keeping those noisy alerts to a minimum.
Next, we’ll look ahead to emerging research and technologies that promise to change how we detect and treat colon cancer in the near future. Stay tuned.
Emerging Research and Technologies
Having covered the essentials of colon cancer—what it is, how it presents, and how it’s diagnosed, treated, and prevented—it’s time to look forward. What does the future hold? Are there breakthroughs on the horizon that might transform how we detect, understand, and manage this disease? The answer is a hopeful yes, and many of these advances are already reshaping care in exciting ways.
One intriguing area of research focuses on gut sounds themselves. Scientists are developing acoustic biosensors—wearable or implantable devices that “listen” to intestinal noises and analyze patterns using artificial intelligence. These tools could one day detect abnormal motility or fermentation changes that signal early cancer or other gut disorders. Imagine a future where subtle changes in your gut’s soundtrack could prompt early investigation—long before symptoms become obvious.
Another breakthrough comes in the form of liquid biopsies. Unlike traditional biopsies that require tissue samples from colonoscopy, liquid biopsies detect circulating tumor DNA (ctDNA) in the bloodstream. This minimally invasive test can identify cancer presence, monitor treatment response, and catch recurrence earlier than imaging or symptoms. Liquid biopsy is rapidly gaining traction as a tool for personalized, less burdensome cancer monitoring.
Artificial intelligence (AI) is also revolutionizing colon cancer care. AI algorithms improve colonoscopy accuracy by helping doctors spot small or flat polyps that might otherwise be missed. AI can analyze complex clinical data to predict prognosis and tailor treatments, leading to more precise and effective care.
Personalized medicine is evolving as well. By decoding the genetic makeup of tumors, oncologists can select targeted therapies designed to attack specific mutations driving cancer growth. Immunotherapy, which empowers the immune system to fight cancer cells, is becoming an important option, especially for tumors with particular genetic profiles.
Preventive screening is not standing still either. Innovations like capsule endoscopy—where you swallow a tiny camera that travels through your digestive tract—offer less invasive ways to visualize the colon, potentially improving screening acceptance. Meanwhile, advanced stool tests analyze genetic and epigenetic markers, offering highly sensitive, non-invasive screening options that may complement or eventually rival colonoscopy.
While many of these technologies are still in development or limited to specialized centers, clinical trials are expanding their availability. If you or a loved one faces colon cancer, discussing access to such innovations with your care team might open doors to cutting-edge diagnostics or treatments.
What’s the big takeaway? Colon cancer care is entering a new era—one where earlier detection, smarter diagnostics, and tailored therapies converge to improve outcomes and reduce treatment burdens. Even stomach noises, once dismissed as trivial, could become part of a sophisticated diagnostic toolkit.
The story of colon cancer is not static. It’s an evolving narrative powered by science, technology, and patient engagement. Staying informed and proactive helps you navigate this rapidly changing landscape.
Frequently Asked Questions (FAQs)
Can stomach noises alone indicate colon cancer?
No. Stomach noises are usually normal digestive sounds. However, if they are louder, persistent, or accompanied by other symptoms like changes in bowel habits, blood in stool, or unexplained weight loss, they warrant medical evaluation.
What distinguishes normal stomach sounds from those that are concerning?
Normal stomach noises vary and are often linked to hunger or digestion. Concerning noises tend to be new, louder, occur frequently, or happen alongside symptoms like pain, bloating, or altered bowel movements.
How often should I get screened for colon cancer?
Screening is generally recommended starting at age 45 for average-risk individuals, earlier for those with family history or other risk factors. Frequency depends on the screening method and findings but typically ranges from every 1 to 10 years.
Are there specific diets that can help prevent colon cancer?
Diets high in fiber, fruits, vegetables, and whole grains and low in red and processed meats reduce risk. Limiting alcohol and avoiding tobacco are also important.
What are the early warning signs of colon cancer?
Early signs may include changes in bowel habits, blood in stool, abdominal discomfort, fatigue, and unexplained weight loss. However, early-stage colon cancer may cause no symptoms.
How is colon cancer diagnosed?
Diagnosis involves medical history, physical exam, stool tests, blood tests, imaging, and definitive confirmation by colonoscopy with biopsy.
Closing Thoughts
Stomach noises are a natural part of life—often just the soundtrack of digestion. But when those sounds change or accompany other symptoms, they might be telling a more important story. Colon cancer, while serious, is one of the most treatable cancers when caught early. Listening to your body, knowing the signs, and staying proactive with screening and healthy lifestyle choices form the cornerstone of prevention and early detection.
Remember, no question or symptom is too small when it comes to your health. Trust your instincts, seek medical advice when needed, and keep informed about advances in care. Your gut’s messages matter—they are part of a vital conversation between you and your body.
Thank you for joining this deep dive into colon cancer and stomach noises. Here’s to empowered health and wise listening—to your body and beyond.