Cold Feet and Raynaud’s Phenomenon: Causes and Symptoms
Cold Feet and Its Clinical Significance
Cold feet are a common symptom experienced by many individuals, often indicating an underlying health condition. While sometimes resulting from environmental factors or temporary body temperature changes, persistent cold feet may signal serious circulatory or vascular issues. One common cause of cold feet is Raynaud’s phenomenon, which involves episodic vasospasm of peripheral blood vessels, reducing blood flow to the extremities and causing them to feel cold, pale, or even cyanotic (blue or purple).
Key Triggers of Raynaud’s Phenomenon:
- Cold temperatures
- Physical or emotional stress
In Raynaud’s disease, cold temperatures or stress can lead to vasoconstriction, worsening symptoms. This condition can be primary, occurring without systemic illness, or secondary, linked to diseases like scleroderma or lupus. Recognizing cold feet as a potential indicator of Raynaud’s phenomenon is essential for identifying patients who may need diagnostic evaluation and management to prevent circulatory complications.
Pathophysiology of Cold Feet and Raynaud’s Phenomenon
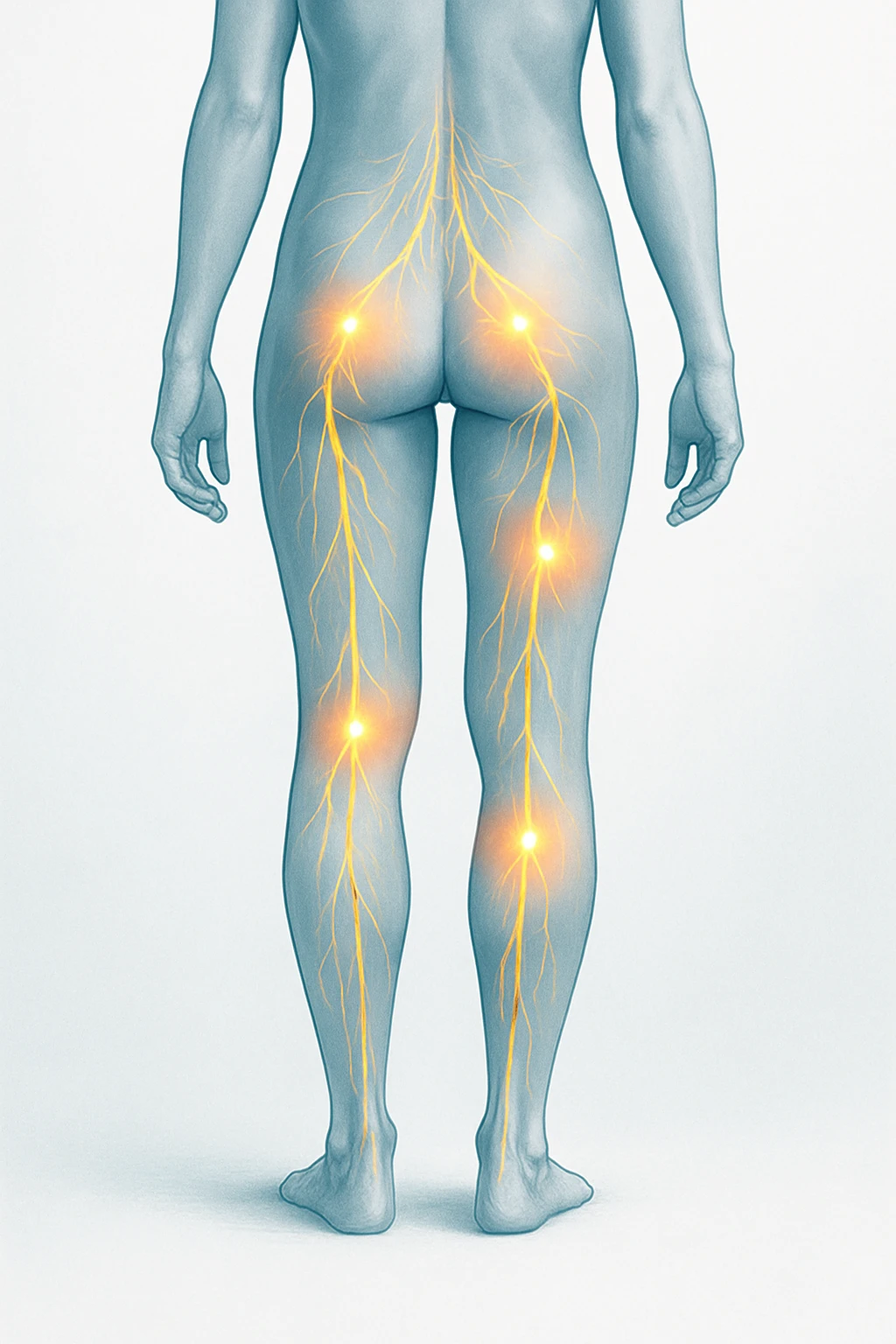
Cold feet, often associated with Raynaud’s phenomenon, occur due to a disruption in normal blood flow to the extremities. Raynaud’s disease causes vasospasm, a constriction of peripheral blood vessels that limits blood flow, leading to cold, pale, or cyanotic extremities.
Vasospasm and Blood Flow Reduction
Vasospasm in Raynaud’s phenomenon involves rapid constriction of blood vessels in the fingers, toes, and other extremities, reducing the amount of oxygenated blood flowing to the tissues. This causes the extremities to feel cold. Prolonged lack of blood supply can lead to tissue damage, contributing to color changes and discomfort.
Triggers of Raynaud’s Phenomenon
Raynaud’s episodes are often triggered by external factors such as cold weather or emotional stress. When exposed to cold, the body constricts blood vessels to conserve heat, which may trigger episodes in individuals with Raynaud’s. Stress activates the sympathetic nervous system, causing vasoconstriction, further exacerbating symptoms. These triggers lead to exaggerated vascular responses, causing cold extremities.
Common Triggers of Raynaud’s Phenomenon:
- Cold weather
- Emotional stress
- Physical exertion
- Exposure to cold temperatures
Raynaud’s Phenomenon: Primary vs Secondary
Primary Raynaud’s Phenomenon
Primary Raynaud’s phenomenon is characterized by episodes of vasospasm without any underlying systemic disease. It is considered idiopathic, where the blood vessels abnormally respond to cold or stress. Individuals typically experience cold, pale, or cyanotic extremities, especially during environmental stressors. This form usually affects otherwise healthy individuals, often starting in early adulthood, and is more common in women. While benign, it can cause discomfort and difficulty managing daily tasks.
Secondary Raynaud’s Phenomenon
Secondary Raynaud’s phenomenon is associated with systemic diseases like scleroderma, lupus, or atherosclerosis, which affect blood vessel regulation. In secondary cases, episodes may be more severe, with patients at greater risk of complications like digital ulcers or tissue necrosis due to chronic poor blood flow. The presence of underlying systemic disease necessitates a more complex management approach that addresses both the primary disease and Raynaud’s symptoms.
Key Differences Between Primary and Secondary Raynaud’s Phenomenon:
- Primary Raynaud’s: Occurs without underlying disease and is generally episodic and benign.
- Secondary Raynaud’s: Triggered by systemic conditions like scleroderma, lupus, or atherosclerosis, leading to more severe symptoms and complications.
Diagnosis of Cold Feet and Raynaud’s Phenomenon
Clinical History and Physical Examination
Diagnosis begins with a detailed patient history and physical examination. Understanding the onset, frequency, and triggers of symptoms is essential. The patient’s medical background, including autoimmune disease history, is important for distinguishing between primary and secondary Raynaud’s phenomenon. The physical exam focuses on identifying color changes, temperature differences, and vascular abnormalities in the extremities.
Diagnostic Tools for Raynaud’s Phenomenon
Diagnostic tools help confirm Raynaud’s phenomenon and differentiate its primary and secondary forms. Nailfold capillaroscopy is a key diagnostic tool where the small blood vessels at the base of the fingernails are examined. In primary Raynaud’s, capillaries appear normal, while in secondary cases, particularly those related to systemic diseases like scleroderma, capillary abnormalities such as dilation or distortion are common. Nailfold capillaroscopy helps clinicians identify microvascular changes and guide diagnosis and treatment planning.
Key Diagnostic Steps:
- Patient History: Document onset, frequency, and triggers of symptoms, as well as underlying conditions.
- Physical Examination: Examine extremities for color changes, temperature differences, and vascular abnormalities.
- Nailfold Capillaroscopy: Examine capillaries at the base of the fingernails to distinguish primary from secondary Raynaud’s phenomenon.
Management and Treatment of Cold Feet
Lifestyle Modifications
For patients experiencing cold feet, particularly those with Raynaud’s phenomenon, lifestyle modifications are crucial in managing symptoms. Warming techniques, such as wearing insulated socks and gloves, help maintain blood flow to the extremities. Stress management is also key, as emotional or physical stress can trigger vasospasm. Regular exercise to improve circulation and avoid prolonged exposure to cold environments further helps mitigate symptoms. These lifestyle changes are often the first line of management for individuals with Raynaud’s and can significantly reduce the frequency and severity of episodes.
Pharmacologic Treatment Options
Pharmacological treatments for cold feet aim to alleviate vasoconstriction and improve blood flow. Calcium channel blockers are commonly prescribed to relax blood vessels, thereby reducing the frequency of Raynaud’s attacks. Emerging treatments include endothelin receptor antagonists, which target the endothelin-1 pathway, known to contribute to vasoconstriction in Raynaud’s phenomenon. Phosphodiesterase inhibitors, which increase blood flow by inhibiting the breakdown of cyclic AMP, also show promise in reducing symptoms. These treatments are particularly effective for patients experiencing moderate to severe Raynaud’s episodes.
Advanced Interventions
In severe or unresponsive cases of Raynaud’s phenomenon, more advanced treatments may be required. Prostacyclin analogs, a class of medications, help dilate blood vessels and improve circulation in patients with severe vascular constriction. In some cases, surgical intervention such as sympathectomy – the surgical severing of nerves responsible for triggering vasoconstriction – may be necessary. These advanced treatments are generally reserved for cases where other interventions have not effectively controlled symptoms.
Summary of Treatment Options:
- Lifestyle Modifications: Warming techniques, stress management, and exercise.
- Pharmacologic Treatments: Calcium channel blockers, endothelin receptor antagonists, phosphodiesterase inhibitors.
- Advanced Interventions: Prostacyclin analogs, sympathectomy.
Psychological and Quality-of-Life Considerations
Psychological Impact of Cold Extremities
Living with chronic cold feet, especially in individuals with Raynaud’s phenomenon, can have significant emotional and psychological effects. The constant discomfort of cold, pale, or cyanotic extremities can lead to feelings of frustration, helplessness, and anxiety. These emotional burdens are particularly prevalent in patients who experience frequent or severe episodes of Raynaud’s, as the unpredictability of symptoms can disrupt daily life and routine activities. Furthermore, dealing with a visible, persistent physical symptom can lead to depression, particularly when the condition is not well understood or effectively managed.
Stress and Symptom Exacerbation
There is a bidirectional relationship between stress and cold feet symptoms. Emotional or physical stress can trigger episodes of vasospasm in Raynaud’s phenomenon, worsening cold extremities and causing further discomfort. In turn, the chronic symptoms of Raynaud’s, such as cold and numbness, can heighten stress levels, creating a vicious cycle. Effective stress management techniques are essential in the treatment plan for Raynaud’s patients. Relaxation techniques, mindfulness, and other coping strategies can help reduce the frequency and severity of Raynaud’s episodes, improving both physical and psychological well-being.
Key Psychological Considerations:
- Anxiety and Depression: Chronic cold feet can contribute to emotional distress, including feelings of helplessness and anxiety.
- Stress and Symptom Cycle: Stress can exacerbate symptoms, while cold extremities can increase stress, creating a vicious cycle.
- Stress Management: Relaxation techniques, mindfulness, and coping strategies are essential for managing both psychological and physical symptoms.
- Cold feet can result from Raynaud’s phenomenon, where vasospasm in peripheral vessels restricts blood flow to the extremities.
- In Raynaud’s disease, cold or stress triggers vasoconstriction, causing cold, pale, or cyanotic extremities.
- Diagnosing cold feet involves a thorough patient history, physical examination, and nailfold capillaroscopy to differentiate primary from secondary Raynaud’s.
- Treatment for Raynaud’s includes lifestyle changes, calcium channel blockers, and, in severe cases, prostacyclin analogs or surgery.
- Emerging therapies for Raynaud’s disease include endothelin receptor antagonists and phosphodiesterase inhibitors to enhance circulation.
- Conditions like acrocyanosis, pernio, and small fiber neuropathy can mimic Raynaud’s phenomenon with similar symptoms.
- What is the connection between cold feet and Raynaud’s phenomenon?
- Cold feet can be caused by Raynaud’s phenomenon, where blood vessels constrict in response to cold or stress, limiting blood flow to the extremities.
- How can Raynaud’s disease affect the appearance of my feet?
- In Raynaud’s disease, episodes of vasospasm can cause cold, pale, or even cyanotic (blue or purple) discoloration of the extremities, particularly during cold exposure or stress.
- What triggers episodes of Raynaud’s phenomenon?
- Episodes of Raynaud’s can be triggered by cold weather, emotional stress, physical exertion, or exposure to cold temperatures.
- Can cold feet be caused by conditions other than Raynaud’s?
- Yes, conditions like acrocyanosis, pernio, and small fiber neuropathy can present with cold extremities, resembling Raynaud’s phenomenon.
- What is the best way to manage cold feet caused by Raynaud’s?
- Management typically includes lifestyle changes such as stress management, wearing warm clothing, and medications like calcium channel blockers to improve blood flow.
- When should I consider medical treatments for cold feet?
- If lifestyle changes do not reduce the frequency or severity of cold feet, medications like endothelin receptor antagonists or, in severe cases, surgical interventions may be necessary.
- How do doctors diagnose Raynaud’s phenomenon?
- Raynaud’s is diagnosed through a patient history, physical exam, and tools like nailfold capillaroscopy, which helps distinguish primary from secondary forms of the condition.