Chronic Cough: Common Causes and Effective Treatment Options
Chronic Cough Overview
Chronic cough is defined as a persistent cough that lasts more than 8 weeks. It is a common clinical issue that affects people globally, often leading to significant discomfort and disruption to daily life. Unlike acute cough, which resolves within a few weeks, chronic cough requires thorough evaluation to determine its underlying cause.
The prevalence of chronic cough varies, with studies estimating it affects between 2% and 18% of the general population. Some demographic groups, such as older adults and women, experience higher rates. Understanding this variation emphasizes the importance of considering individual risk factors and health conditions when managing chronic cough.
Common Causes of Chronic Cough
Chronic cough can arise from several conditions, including upper airway cough syndrome (UACS), asthma, gastroesophageal reflux disease (GERD), and nonasthmatic eosinophilic bronchitis. Recognizing these causes is key to accurate diagnosis and effective treatment.
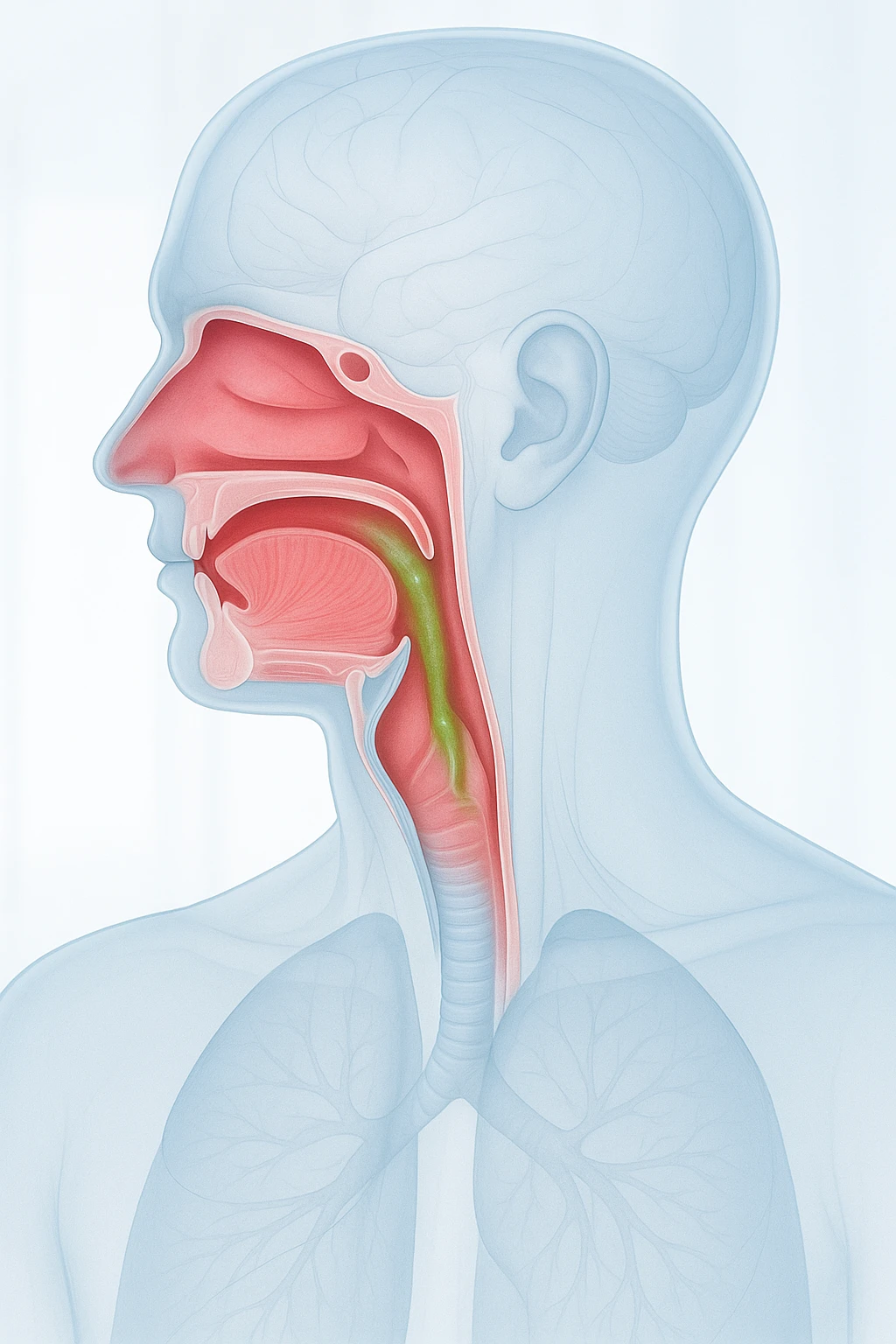
Upper Airway Cough Syndrome
UACS occurs when postnasal drip irritates the throat, triggering a persistent cough. This happens when excess mucus from the sinuses drips down the back of the throat, causing the body to clear the mucus. UACS is often linked to conditions such as allergies, sinus infections, or nasal polyps and is one of the most common causes of chronic cough.
Asthma and GERD
Asthma and GERD are significant contributors to chronic cough. Asthma involves airway inflammation and narrowing, causing coughing, wheezing, and shortness of breath. Triggers such as allergens or exercise can worsen the cough. GERD occurs when stomach acid irritates the throat and respiratory tract, often resulting in a chronic cough. Many individuals have both asthma and GERD, complicating treatment and exacerbating symptoms.
Nonasthmatic Eosinophilic Bronchitis
This condition is characterized by eosinophilic inflammation of the airways, leading to persistent coughing without typical asthma symptoms such as wheezing or shortness of breath. Coughs are often triggered by environmental irritants like smoke or pollutants. Distinguishing this condition from asthma is essential as treatment approaches may differ.
Risk Factors and Demographic Variations
Chronic cough is influenced by several risk factors, including smoking, asthma, GERD, and lower socioeconomic status. Recognizing these factors, along with their demographic variations, is crucial for effective management.
Smoking and Chronic Cough
Smoking is a primary risk factor for chronic cough. The chemicals in tobacco smoke irritate the airways, leading to inflammation and increased mucus production. Smokers are also at a higher risk of developing respiratory conditions such as chronic bronchitis and emphysema, both of which contribute to persistent coughing. Smoking can worsen pre-existing conditions like asthma, exacerbating chronic cough.
Asthma, GERD, and Socioeconomic Status
Apart from smoking, asthma and GERD contribute significantly to chronic cough. Asthma causes airway inflammation and narrowing, leading to coughing, wheezing, and difficulty breathing. Exposure to allergens can worsen asthma-related coughing. GERD occurs when stomach acid refluxes into the esophagus, irritating the throat and causing a chronic cough. Additionally, lower socioeconomic status has been linked to a higher prevalence of chronic cough, often due to factors such as limited access to healthcare, higher smoking rates, and increased exposure to pollutants.
Impact on Quality of Life
Chronic cough severely impacts an individual’s quality of life. It affects both physical and mental well-being, often leading to anxiety, depression, and impaired sleep, creating a cycle that complicates the management of the condition.
Mental Health Consequences
Chronic cough often leads to anxiety and depression due to the ongoing discomfort and the social stigma surrounding the condition. Unpredictable coughing fits, particularly in public or during conversations, can cause embarrassment and self-consciousness. Over time, this can lead to social isolation, worsening anxiety. The constant focus on the cough can contribute to depression, as it hinders engagement in daily activities and enjoyment of life. These mental health issues not only worsen the perception of chronic cough but can also decrease the effectiveness of treatment efforts.
Physical Burden of Chronic Cough
The physical impact of chronic cough is equally significant. It disrupts sleep, causing fatigue and decreased physical functioning. Frequent waking due to coughing episodes leads to daytime drowsiness, reduced concentration, and impaired performance at work or school. Chronic cough can also cause muscle soreness and, in severe cases, rib fractures. This physical strain weakens the body and reduces vitality, making it harder for individuals to perform daily tasks, further lowering their quality of life.
Diagnosis and Treatment Strategies
Diagnosing and managing chronic cough requires a comprehensive approach, as it can stem from various underlying causes. The diagnostic process includes a detailed clinical evaluation, using common tests to pinpoint the source of the cough. Once the cause is determined, treatment options range from pharmacological interventions to lifestyle modifications, with a stepwise approach ensuring the best care.
Clinical Evaluation and Testing
The diagnostic process begins with a thorough clinical evaluation, including a detailed history of the cough, its onset, duration, and triggers. Physical exams can reveal signs of respiratory or gastrointestinal issues. Common diagnostic tests include spirometry to assess lung function and identify asthma or other respiratory conditions. Chest X-rays may help rule out infections or structural abnormalities. pH monitoring can diagnose GERD-related cough, a frequent but often underrecognized cause.
Pharmacological Treatments
Once the cause is identified, treatment is tailored to the specific diagnosis. Pharmacological treatments include inhalers for asthma or COPD, which help with airway inflammation. For GERD-related cough, proton pump inhibitors (PPIs) reduce stomach acid production to prevent throat irritation. Antihistamines or nasal corticosteroids are prescribed for allergies or postnasal drip-related cough.
Non-Pharmacological Approaches
Non-pharmacological treatments are also crucial. Smoking cessation is a key step for smokers, as tobacco smoke is a significant irritant to the airways. Managing GERD through lifestyle changes, such as avoiding trigger foods and eating smaller meals, can help reduce symptoms. For individuals with nonasthmatic eosinophilic bronchitis, avoiding environmental irritants, such as smoke and air pollution, can reduce coughing episodes. These combined approaches are essential for managing chronic cough effectively.
Economic and Healthcare Burden of Chronic Cough
Chronic cough imposes a significant burden on both healthcare systems and individuals. As the condition persists, it leads to increased healthcare resource usage, including frequent doctor visits, hospitalizations, and emergency department visits. This not only affects the patients but also contributes to escalating healthcare costs.
Increased Healthcare Visits
Individuals with chronic cough often require frequent visits to healthcare providers, including both primary care physicians and specialists such as pulmonologists or gastroenterologists. These visits typically focus on managing the underlying causes of chronic cough, which may require continuous monitoring and adjustments in treatment plans. As a result, patients may experience a higher frequency of consultations, contributing to a rise in healthcare utilization.
Hospitalization and Emergency Department Visits
Chronic cough is associated with an increased number of hospitalizations and emergency department (ED) visits, particularly when the condition worsens or leads to complications like respiratory infections or severe asthma exacerbations. Patients may seek immediate care during acute coughing episodes that disrupt breathing or cause significant discomfort. These visits are often costly and can lead to longer stays in healthcare facilities, further adding to the financial burden of managing chronic cough.
Diagnosis and Treatment of Chronic Cough
Diagnosing and managing chronic cough requires a comprehensive approach, as the condition can arise from a variety of underlying causes. The diagnostic process involves a thorough clinical evaluation, including common tests to pinpoint the source of the cough. Once the cause is identified, treatment options range from pharmacological interventions to lifestyle modifications, with a stepwise approach to therapy ensuring optimal care for the patient.
Clinical Evaluation and Testing
The first step in diagnosing chronic cough is a detailed clinical evaluation. Healthcare providers will typically begin by taking a thorough history, asking about the onset, duration, and triggers of the cough. Physical exams may reveal signs of respiratory or gastrointestinal issues that could be contributing to the cough. Common diagnostic tests include:
- Spirometry: Assesses lung function and identifies asthma or other obstructive pulmonary conditions.
- Chest X-rays: Helps rule out structural abnormalities or infections.
- pH Monitoring: Used for diagnosing gastroesophageal reflux disease (GERD), which is a common cause of chronic cough.
Pharmacological Treatments
Once an underlying cause is identified, treatment options are tailored to the specific diagnosis. Some common pharmacological treatments include:
- Inhalers (bronchodilators and corticosteroids): Used for asthma or chronic obstructive pulmonary disease (COPD), conditions that involve airway inflammation.
- Proton Pump Inhibitors (PPIs): Prescribed for GERD-related cough to reduce stomach acid production and prevent irritation in the throat and respiratory tract.
- Antihistamines or Nasal Corticosteroids: Used when chronic cough is related to upper airway cough syndrome caused by allergies or postnasal drip.
Non-Pharmacological Approaches
Alongside medications, non-pharmacological strategies are essential for managing chronic cough. Some effective approaches include:
- Smoking Cessation: A key strategy for individuals who smoke, as tobacco smoke is a major irritant to the airways and a primary cause of chronic cough.
- GERD Management: Lifestyle changes, such as avoiding trigger foods and eating smaller meals, can alleviate symptoms.
- Avoiding Environmental Irritants: For patients with nonasthmatic eosinophilic bronchitis, avoiding smoke and air pollution can reduce coughing episodes.
These non-pharmacological approaches, combined with medical treatments, form the cornerstone of effective chronic cough management.
- Chronic cough is a persistent cough lasting over 8 weeks.
- The prevalence of chronic cough ranges from 2% to 18%, varying by region and demographics.
- Approximately 10% of adults in the U.S. experience chronic cough, with higher rates in women and older individuals.
- Common causes of chronic cough include upper airway cough syndrome, asthma, GERD, and nonasthmatic eosinophilic bronchitis.
- Smoking significantly increases the risk of chronic cough.
- Risk factors for chronic cough also include asthma, GERD, and lower socioeconomic status.
- Chronic cough can severely affect quality of life, leading to anxiety, depression, and disrupted sleep.
- It is linked to increased healthcare usage, including more visits to emergency departments and hospitalizations.
- Management involves identifying and treating the underlying causes, with a stepwise approach to therapy.
Frequently Asked Questions about Chronic Cough
- What is chronic cough? Chronic cough is a persistent cough that lasts longer than 8 weeks, differing from acute cough which typically resolves within a few weeks.
- What are the main causes of chronic cough? Common causes include upper airway cough syndrome (UACS), asthma, gastroesophageal reflux disease (GERD), and nonasthmatic eosinophilic bronchitis.
- How does smoking affect chronic cough? Smoking irritates the airways, leading to inflammation and excess mucus production, which can trigger or worsen chronic cough.
- Why is chronic cough more common in some people? Factors such as age, gender (more common in women), and lower socioeconomic status are linked to higher rates of chronic cough.
- What impact does chronic cough have on mental health? Chronic cough can lead to anxiety and depression due to ongoing discomfort and social stigma, often exacerbated by embarrassment during coughing episodes.
- How does chronic cough affect sleep? Persistent coughing, especially at night, can disrupt sleep, leading to daytime fatigue and reduced concentration, which further impacts quality of life.
- Can chronic cough be treated? Yes, treatment often involves managing the underlying causes, such as using inhalers for asthma, PPIs for GERD, or antihistamines for allergies.
- Is chronic cough linked to other health problems? Chronic cough is often associated with increased healthcare visits, hospitalizations, and emergency department visits, contributing to higher healthcare costs.