Celebrities with Prostate Cancer: Stories, Science & Support
- Foreword: Why This Topic Matters More Than You Think
- Part 1: Celebrity Diagnoses – A Chronological Overview
- Part 2: Understanding Prostate Cancer – What Every Man (and Woman) Should Know
- Part 3: In-Depth Profiles – What Celebrity Journeys Really Teach Us
- Part 4: The Power of Celebrity Advocacy – From Headlines to Health Impact
- Part 5: The Science Behind Prostate Cancer – What’s New, What Matters
- Part 6: Resources and Support – Navigating the Journey Together
- FAQ: What You Really Want to Know About Prostate Cancer
- A Final Word
Foreword: Why This Topic Matters More Than You Think
Let’s face it—celebrity health stories are everywhere. Some people dismiss them as tabloid fodder, others read them with casual curiosity. But occasionally, a headline about a famous actor, musician, or politician confronting illness does more than stir gossip—it sparks a global conversation. And in the case of prostate cancer, that conversation is long overdue.
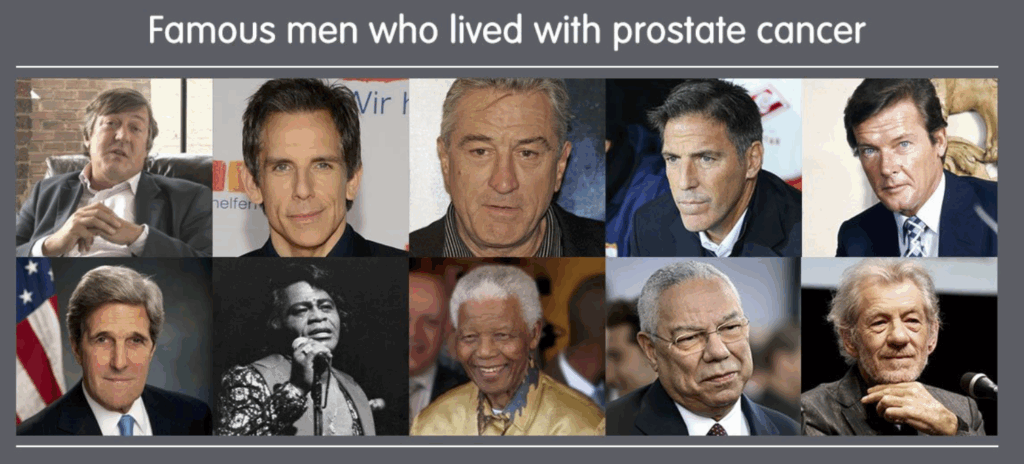
You might ask: Why should I care about which celebrity had prostate cancer? That’s a fair question. The answer lies not in celebrity culture, but in what happens because of it. When someone like Ben Stiller goes public with his diagnosis at 48—years before the average man even thinks about a PSA test—it challenges outdated assumptions. When someone like Colin Powell uses his platform to speak directly to African American men, a group disproportionately affected by the disease, it becomes more than a personal story. It becomes public health advocacy.
Prostate cancer is one of the most common cancers among men. One in eight men will be diagnosed with it during their lifetime. Yet for something so statistically unignorable, public understanding often remains frustratingly shallow. There’s confusion about symptoms (or lack thereof), hesitation around screening, and stigma about discussing anything related to “men’s health” below the belt.
This article aims to change that.
We’re going to walk through the stories of public figures who have lived with prostate cancer—some who survived, some who didn’t—and explore how their journeys mirror and diverge from the average patient’s experience. Along the way, we’ll unpack what prostate cancer really is, who’s most at risk, and what modern treatment and recovery look like.
But this isn’t just a celebrity roundup or a clinical manual. It’s a bridge between the headlines and the hard science—between public lives and private health choices.
By the end of this read, you won’t just know who had prostate cancer. You’ll understand why it matters that they told us.
Celebrity Diagnoses – A Chronological Overview
Let’s begin with what often makes people click: the names. The faces we recognize. The actors who made us laugh, the musicians who scored the soundtracks of our lives, the world leaders who shaped history. But instead of treating these individuals like entries on a trivia list, let’s look at the arc—how their stories have evolved over time and what they’ve meant in context.
The Early Years: Silence and Stigma
Rewind to the 1980s and 1990s. Back then, prostate cancer was rarely discussed in public. When a celebrity was diagnosed—if it even became known—it was often after death or in a brief press release buried beneath more glamorous headlines. Privacy was the norm, and so was stigma.
Take Frank Zappa, the avant-garde musician and cultural icon. He died of prostate cancer in 1993 at age 52. By all accounts, his illness was kept under wraps for much of his final years. Zappa wasn’t alone. Many men in that era faced not just the disease, but a kind of social muting. To speak openly about prostate issues was to court embarrassment—a notion we now recognize as both outdated and dangerous.
The 2000s: Cracks in the Silence
The shift began in the early 2000s. High-profile figures began to speak more candidly, driven in part by a broader movement toward medical transparency.
Nelson Mandela—yes, that Nelson Mandela—was treated for prostate cancer in 2001. Though much of the coverage was carefully managed, it marked a pivotal moment. If a global statesman could acknowledge the condition without shame, perhaps other men could follow.
Dennis Hopper was another. Diagnosed in 2009, his case was widely reported, particularly as the illness progressed quickly. He passed away in 2010. What stood out, however, was how public his final months were—a bittersweet but important visibility for a disease still relegated to whispered conversations.
The 2010s: Advocacy Emerges
This decade saw a major turning point. Celebrities stopped just “revealing” diagnoses—they started using them.
Ben Stiller’s 2016 revelation is a textbook case. Diagnosed at 48 after a proactive PSA test (which he admits he initially didn’t even understand), Stiller went on the media circuit to discuss why early testing saved his life. He wasn’t pushing a product or chasing sympathy—he was laying down facts, making a case for the value of screening, especially for men under 50 who otherwise wouldn’t consider it.
Other notables—like Robert De Niro, who underwent surgery in the early 2000s but kept the story private until much later—added their voices in subtler ways. In interviews and documentaries, they acknowledged their cancer without dramatization, but with undeniable gravity.
The 2020s: Transparency and Technology
In the past five years, there’s been another evolution—not just in who’s speaking, but how they’re doing it.
Take Rod Stewart. In 2019, he revealed he’d been diagnosed two years earlier—and was now cancer-free. “No one knows this,” he told a crowd at a charity fundraiser, “but I thought it was time I told everybody.” Why? To help others. “Guys, you’ve got to really go to the doctor,” he added, “Finger up the bum, no harm done.”
Blunt? Absolutely. Effective? Undeniably.
More recently, men like Stephen Fry in the UK have opened up about their experiences with remarkable candor, documenting their treatment and recovery in real-time. This willingness to demystify the process—from MRI to surgery to incontinence and beyond—represents a cultural shift. Prostate cancer is no longer just an old man’s quiet burden. It’s a conversation.
Celebrity disclosures often shift public perception, which is why it’s interesting to contrast this with more technical coverage like the PI-RADS 4 Prostate Cancer guide — it shows what those behind the headlines may actually be facing.
Coming next in Part 2: We’ll break down what prostate cancer actually is, how it behaves, why it’s often asymptomatic, and what every man (and the people who love them) should know about detection, risk, and treatment.
Understanding Prostate Cancer – What Every Man (and Woman) Should Know
So now that we’ve heard the headlines—Rod Stewart cracking jokes about rectal exams, Ben Stiller crediting a PSA test with saving his life—you might be wondering: What is prostate cancer, really? Isn’t it just a “slow-growing old man’s disease”? Should we all be panicking? Or relaxing?
The reality, as is often the case in medicine, sits somewhere between alarm and apathy.
Let’s start with the basics.
First Things First: What Is the Prostate?
If you’re not quite sure where your prostate is or what it does, you’re in good company. It’s not exactly dinner-table conversation. But it is important.
The prostate is a small gland, roughly the size of a walnut, tucked just below the bladder and in front of the rectum. It plays a key role in male reproductive function—specifically, it produces seminal fluid that nourishes and transports sperm. It’s not glamorous, but it’s vital.
So why does it cause so much trouble?
Because like all glands, it’s made of cells. And sometimes, those cells start multiplying out of control.
What Is Prostate Cancer?
Prostate cancer occurs when cells in the prostate begin to grow uncontrollably. Most of the time, this starts in the outer part of the gland and grows slowly. In fact, many men with prostate cancer never experience symptoms or require treatment—the disease is discovered incidentally during routine screening or after investigating unrelated symptoms.
But don’t let that lull you into complacency.
Some prostate cancers grow aggressively. They can spread to the lymph nodes, bones, or other organs. And when they do, they become significantly harder to treat. That’s why early detection matters. The trouble is, early-stage prostate cancer usually doesn’t feel like anything.
No pain. No lumps. No obvious warning signs.
Which brings us to the natural question:
How Do You Know If You Have It?
Short answer: you often don’t—unless you test for it.
Here’s where we get into slightly controversial territory. The two most common ways to screen for prostate cancer are:
- PSA Test (Prostate-Specific Antigen): A simple blood test that measures a protein produced by the prostate. High levels can be a red flag, though not always for cancer—an inflamed or enlarged prostate (benign prostatic hyperplasia) can also elevate PSA.
- DRE (Digital Rectal Exam): Yes, that one. A doctor inserts a gloved finger into the rectum to feel for abnormalities on the prostate surface. It takes seconds. It’s awkward, but not painful—and potentially life-saving.
Now, here’s the nuance: not everyone agrees on when to screen, or how often. Some medical organizations recommend starting at age 50. Others suggest earlier screening—around age 45—for men at higher risk (we’ll get to that). Still others worry about overdiagnosis: catching cancers so slow-growing they’d never cause harm, and treating them anyway.
It’s a balancing act. One best navigated through conversation—with a doctor, yes, but ideally with awareness like this too.
Who’s Most at Risk?
Let’s unpack the risk factors:
- Age: This is the big one. Prostate cancer is rare under 40, but the risk climbs steeply after 50.
- Family History: If your father or brother had prostate cancer, your risk doubles. If multiple relatives were diagnosed, or if they were diagnosed young, your risk climbs even higher.
- Ethnicity: Black men are significantly more likely to be diagnosed with prostate cancer, and more likely to develop aggressive forms of it. No one fully understands why, though genetic and socioeconomic factors are likely contributors.
- Genetics: Mutations in genes like BRCA1 and BRCA2 (the same ones associated with breast and ovarian cancer in women) can also elevate risk in men.
- Lifestyle: While the research is less definitive here, some studies suggest that obesity, a sedentary lifestyle, and high-fat diets may contribute to more aggressive prostate cancers.
So yes, being male and aging are the biggest unavoidable factors. But family history, race, and lifestyle layer on risk—and awareness of these factors can guide screening decisions.
Let’s say your PSA is elevated. Maybe a DRE feels suspicious. What then?
What Happens After Diagnosis?
The next step is often a biopsy, typically done using a needle guided by ultrasound. If cancer is found, it’s graded and staged:
- Grade tells us how abnormal the cells look under a microscope—this is where the Gleason score comes in. The higher the score (out of 10), the more aggressive the cancer.
- Stage tells us how far the cancer has spread. Localized? Just in the prostate. Locally advanced? It’s spread to nearby tissue. Metastatic? It’s moved to distant parts of the body.
The treatment plan depends on both of these.
What Are the Treatment Options?
There’s no one-size-fits-all answer here, and that’s part of what makes this disease so complex—and personal.
- Active Surveillance: For low-risk cancers, particularly in older men, the best option may be to watch and wait. PSA levels are monitored regularly, and treatment only begins if the cancer shows signs of progressing.
- Surgery: Usually involves removing the entire prostate (radical prostatectomy). This can be curative, especially when the cancer is localized—but it carries risks, including urinary incontinence and erectile dysfunction.
- Radiation Therapy: Can be external or internal (brachytherapy). It’s effective but can also cause long-term side effects.
- Hormone Therapy: Prostate cancer feeds on testosterone. Cutting off that supply—either through medication or surgery (orchiectomy)—can slow or stop growth, particularly in advanced cases.
- Chemotherapy & Immunotherapy: Reserved for later stages, especially when other treatments stop working.
One of the silver linings? The past decade has seen huge advances in treatment. Precision medicine, robotic surgery, better radiation targeting—all of these are giving men more choices and better outcomes than ever before.
So—Should You Be Worried?
Not worried. Aware.
Prostate cancer isn’t an automatic death sentence. Many men live long, full lives after diagnosis. Some never even need treatment. But ignoring it? Hoping it goes away? That’s a gamble with poor odds.
If you’re a man over 45 (especially if you’re Black or have a family history), have a conversation with your doctor. You don’t need to commit to anything. Just talk. Just ask.
And if you’re not a man? You still have a stake in this. Sons, brothers, fathers, friends—your awareness might be the nudge that gets someone you love to take action.
Some readers may be exploring disability or veteran care routes too, and the VA disability rating breakdown offers clarity on what’s covered.
Part 3: In-Depth Profiles – What Celebrity Journeys Really Teach Us
Let’s shift gears. You now understand the biology of prostate cancer—where it starts, how it spreads, why it hides. But statistics can only take us so far. They give us scale, not soul.
To really feel the human stakes of this disease, we have to look at stories. Names. Faces. People we know—or at least feel like we know. And that’s where celebrities become uniquely powerful. Not because their lives matter more, but because they play out in public. Their pain, their choices, their fears—when shared—can inform and influence thousands, if not millions.
But let’s be clear: this isn’t about voyeurism. It’s about visibility. When someone famous says “I had prostate cancer,” they peel back the curtain on something deeply private—and they make it okay for others to talk about it too.
So let’s talk about them.
Ben Stiller – The Comedian Who Didn’t Laugh This Off
Ben Stiller’s story is, in many ways, a model of how early detection should work. In 2014, at just 48 years old—an age not traditionally flagged for routine screening—he underwent a PSA test. It was his doctor’s idea. Stiller had no symptoms. No family history. Nothing that screamed “at risk.”
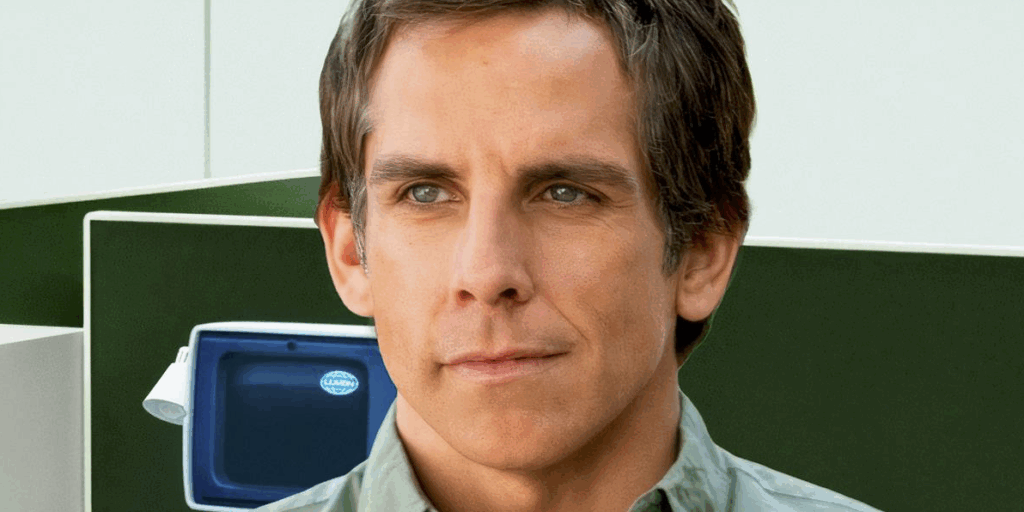
And yet, the PSA came back high. A follow-up test confirmed it. A biopsy sealed it. He had prostate cancer.
Within weeks, he’d opted for surgery to remove the prostate. The cancer was contained, and he’s been cancer-free ever since.
So what made his story different?
Stiller went public not to be inspirational—but to be practical. He published a detailed essay on Medium explaining how he never would’ve caught the cancer early if not for a PSA test that many medical guidelines don’t recommend until 50 or even 55. He didn’t advocate for panic or over-testing. He advocated for informed choice.
“Taking the PSA test saved my life,” he wrote. “Literally. That’s why I’m writing this now.”
It’s a line that still echoes in prostate cancer forums and advocacy circles. Because it didn’t come from a doctor. It came from Zoolander. And that reach made a difference.
Robert De Niro – Stoic, Private, and Unapologetically Resilient
Robert De Niro, like many men of his generation, kept his diagnosis close to the chest. He was diagnosed in 2003 at age 60. He chose surgery and, by all accounts, made a full recovery.

Unlike Stiller, De Niro didn’t give interviews about his diagnosis. There was no essay, no press tour. He didn’t owe the public a detailed accounting. But his quiet resilience is instructive in its own way.
Here was a man known for portraying the ultimate tough guys—from Raging Bull to Goodfellas—openly facing a disease that many still associate with vulnerability and diminished masculinity. And in doing so, he reminded the world that strength isn’t about invincibility. It’s about confrontation.
De Niro may not have raised awareness in the conventional sense. But he did something else: he normalized survival. He went on with his life, his career, his advocacy work. Cancer was just one chapter.
Rod Stewart – “No One Knew… Until Now”
Few celebrity prostate cancer disclosures have been as classically Rod Stewart as the one he made in 2019. Standing onstage at a charity event, microphone in hand, he casually announced:

“No one knows this, but I thought it was about time I told everybody. I’m in the clear now, simply because I caught it early.”
He had been diagnosed two years earlier and treated successfully. The news stunned the audience—not just because it was personal, but because it was so unfiltered.
Then came the kicker: “Guys, you’ve got to really go to the doctor. Finger up the bum, no harm done.”
Was it cheeky? Yes. Was it effective? Absolutely.
Here’s why Stewart’s delivery mattered. His fans span generations. Many of them are in their 50s, 60s, 70s—the exact demographic that often dodges medical exams out of fear, embarrassment, or inertia. Stewart’s bluntness cut through that. He made the uncomfortable conversation laughably normal.
Sometimes that’s all it takes.
Andrew Lloyd Webber – Creativity Interrupted, Not Ended
The legendary composer of Phantom of the Opera and Cats was diagnosed with prostate cancer in 2009. And while his cancer was treated successfully, Webber was unusually candid about the toll it took—not just physically, but emotionally.

In interviews, he spoke of the depression that followed his diagnosis. The strange sense of vulnerability. The frustrations of dealing with side effects like fatigue and incontinence, especially as someone whose life had been defined by creativity and momentum.
“I lost confidence in myself. I couldn’t write,” he admitted later. “It felt like the music had gone.”
That honesty resonated. Not every cancer survivor feels “empowered” post-treatment. Some feel drained. Changed. Even broken for a time. But acknowledging that reality is part of the healing too.
Webber’s story reminds us that cancer isn’t always a clean arc from diagnosis to triumph. It’s often jagged, messy—and profoundly human.
Colin Powell – The Statesman Who Knew His Risk
Colin Powell, former U.S. Secretary of State, was diagnosed with prostate cancer in 2003 at age 66. A Black man with a demanding public role, he was in a high-risk category—and he knew it. He underwent surgery and recovered well.

But Powell didn’t stop there. He spoke openly about the disproportionate impact of prostate cancer on Black men. He used his platform to encourage early screening and better access to healthcare.
His death in 2021, unrelated to cancer, brought his prostate story back into public view—and with it, renewed discussion about racial disparities in prostate cancer outcomes.
Powell didn’t just survive. He educated. And that, too, is a form of legacy.
What Do These Stories Tell Us?
They’re not just anecdotes. They’re signals.
They show that prostate cancer doesn’t care how rich you are, how talented, how powerful, or how beloved. It comes for sitcom stars and generals, rock icons and reclusive composers alike.
But they also show what’s possible—with early detection, informed choices, and the courage to speak publicly about something deeply private.
You may never star in a movie or sell out a stadium. But your story, or the story of someone you love, is no less important.
And perhaps the lesson behind all of this is deceptively simple: Talk about it.
Next up in Part 4: We’ll zoom out again and explore how these celebrity disclosures have shaped public health awareness, altered cultural norms, and actually moved the needle on prostate cancer research and funding.
The Power of Celebrity Advocacy – From Headlines to Health Impact
Let’s pause for a second and ask something deceptively simple: Do celebrity health disclosures actually matter? Or are we just giving undue weight to famous people’s lives because… well, because they’re famous?
On one level, it’s easy to be skeptical. Celebrities don’t necessarily know more about prostate cancer than your next-door neighbor. They’re not trained physicians. They don’t sit on review boards. They don’t write medical guidelines.
But here’s the reality: they don’t need to.
In public health, visibility often trumps technical expertise. A single candid interview, a late-night TV appearance, or even an off-the-cuff joke on a talk show can spark more awareness—and more action—than a hundred brochures sitting unread in a clinic.
So yes, celebrity disclosures matter. In fact, when it comes to prostate cancer, they’ve reshaped the landscape more than you might think.
From Private Worry to Public Conversation
There was a time when prostate cancer was barely spoken of outside of hospitals and support groups. It wasn’t just medical—it was personal, intimate, and often cloaked in silence. After all, what part of invasive rectal exams or erectile dysfunction after surgery screams “dinner conversation”?
But as more celebrities began to open up—first reluctantly, then courageously—that silence started to break.
Suddenly, prostate cancer wasn’t just something whispered about in waiting rooms. It was being discussed on morning shows, in magazine profiles, on podcasts. And that shift—seismic as it was—started a ripple effect in the real world.
One famous example? The “Angelina Jolie Effect.”
In 2013, Jolie publicly revealed that she carried a BRCA1 mutation and had undergone a preventative double mastectomy. Genetic testing for breast cancer risk surged in the months that followed—by some estimates, up to 64% in certain demographics.
The same kind of effect, albeit less formally studied, has occurred with male cancers. Ben Stiller’s PSA essay sparked a wave of Google searches. Rod Stewart’s comments were echoed across social media by men who’d previously avoided their annual exams. Stephen Fry’s detailed public journey led to a spike in discussion on UK-based health forums.
This isn’t celebrity worship. It’s behavioral science.
Shifting Attitudes, Changing Behavior
A growing body of research backs this up. Several studies have shown that when celebrities disclose a health condition—particularly one involving early detection or preventative care—it significantly boosts public engagement.
A 2020 analysis published in BMJ Open looked at trends following celebrity health announcements. It found that disclosures about cancer diagnoses consistently led to measurable increases in health-seeking behavior, especially among the demographic matching the celebrity’s profile.
In other words, when a beloved 60-year-old actor says, “I had no symptoms, and it could’ve killed me,” a 60-year-old fan listens.
These moments don’t just lead to curiosity. They lead to action—appointments made, tests requested, questions asked that might otherwise never have surfaced.
And sometimes, that’s all it takes to save a life.
How Celebrity Advocacy Shapes Medical Policy
This is where things get even more interesting.
It’s not just that celebrities influence individual behavior—they can shape institutional responses too. When enough noise builds around a specific issue, public health agencies pay attention.
Take prostate cancer screening. The U.S. Preventive Services Task Force (USPSTF) updated its PSA screening guidelines in 2018, softening its previously strong stance against routine screening for men aged 55–69. One of the reasons? Increased public pressure to allow more individualized decision-making—pressure driven in part by high-profile patient stories.
In the UK, campaigns led by figures like Stephen Fry and Bill Turnbull (a former BBC presenter who died of prostate cancer in 2022) influenced both government awareness campaigns and funding for targeted outreach in at-risk populations.
This isn’t just soft power. It’s real, structural change—and it often begins with someone famous saying, “I went through this. Let’s talk about it.”
Cultural Shift: Making Men’s Health Less Taboo
Perhaps the biggest long-term impact of celebrity advocacy isn’t clinical—it’s cultural.
Historically, men have been less likely than women to seek preventative care, discuss symptoms, or pursue follow-ups. Why? A toxic cocktail of stigma, stoicism, and societal expectations around masculinity.
But what happens when the most traditionally masculine men you can imagine—think Robert De Niro, Rod Stewart, or even James Bond himself, Pierce Brosnan, whose father died of prostate cancer—publicly confront their vulnerability?
It resets the narrative.
Suddenly, going to the doctor isn’t weak. Admitting you’re scared isn’t emasculating. Getting a PSA test becomes something your hero does—not something you avoid out of discomfort.
You can trace this cultural thaw in real time. Compare magazine editorials or daytime talk shows from the 1990s to those today. The tone has shifted from “uncomfortable necessity” to “informed self-advocacy.”
And celebrity voices are the megaphone through which much of that shift has happened.
A Tangible Legacy
So what’s the real takeaway here?
Celebrity disclosures aren’t just anecdotes—they’re catalysts. They push conversations into the mainstream. They prompt men to take ownership of their health. They nudge medical institutions toward more human-centered policies.
And they provide something else, too: hope.
When someone sees that a public figure they admire not only survived prostate cancer but thrived afterward—continued working, creating, living—it reframes what a diagnosis means. It softens the terror. It offers a roadmap.
We live in a world saturated with information. But not all information carries equal weight. Sometimes, it takes a familiar face to deliver the message in a way that actually sticks.
It’s also worth keeping prostate in context with other men’s health cancers, such as the less-discussed but no less real Testicular Cancer and Low Testosterone link.
The Science Behind Prostate Cancer – What’s New, What Matters
By now, you’ve heard the personal stories and seen how celebrity voices have shaped awareness and action. But behind every diagnosis, every treatment choice, and every public disclosure is a swirl of science—often complex, sometimes frustratingly slow, but always evolving.
So let’s pull back the curtain and ask: What does modern research tell us about prostate cancer? And where is it headed?More importantly, what should you know to make sense of it all?
➤ Why Does Prostate Cancer Happen? The Genetics Puzzle
Cancer, at its core, is a disease of the genome: cells lose their ability to regulate growth due to mutations in DNA. But prostate cancer isn’t caused by a single gene mutation. Instead, it’s a multifaceted puzzle involving multiple genetic and environmental factors.
You may have heard about BRCA genes—famously linked to breast and ovarian cancer risk. Well, here’s something less commonly known: mutations in BRCA1 and BRCA2 can also increase a man’s risk of aggressive prostate cancer. If you have a family history of these mutations, it’s a signal to discuss genetic testing with your doctor.
But BRCA isn’t the whole story.
Scientists have identified dozens of other gene variants that subtly raise prostate cancer risk. This polygenic risk score—an aggregate of many small genetic changes—is starting to help doctors personalize screening and prevention strategies.
Genetics doesn’t just predict risk. It’s reshaping treatment, too. For example, men with certain DNA repair mutations might benefit from newer drugs called PARP inhibitors, which target cancer cells’ ability to fix their own DNA.
➤ Disparities: Why Are Black Men More at Risk?
This is one of the most urgent questions in prostate cancer research—and in public health overall.
Black men are about 60% more likely to be diagnosed with prostate cancer and more than twice as likely to die from it compared to white men. Why?
No single answer exists, but the truth is a complex mix of genetics, socioeconomics, access to healthcare, and systemic inequalities.
Researchers have found some genetic differences that may contribute. But social factors—like delayed diagnosis due to poor access or mistrust of the healthcare system—play a huge role.
This means addressing disparities requires more than medicine. It demands community outreach, culturally sensitive education, and policy changes aimed at equity.
➤ Precision Medicine: Tailoring Treatment to the Individual
Remember when prostate cancer treatment was basically “one size fits all”? Those days are fading fast.
Thanks to advances in genomics and molecular biology, doctors are now able to classify tumors not just by size and spread, but by genetic profile and behavior. This helps differentiate which cancers need aggressive treatment and which can be safely monitored.
Techniques like MRI-guided biopsies and genomic testing reduce unnecessary procedures and help avoid overtreatment—a major concern with prostate cancer.
For the patient, this means less guesswork and fewer side effects. For the healthcare system, smarter resource use.
➤ Immunotherapy and New Frontiers
You may have heard about immunotherapy revolutionizing treatment for cancers like melanoma or lung cancer. Prostate cancer has been slower to respond, but progress is underway.
Scientists are testing vaccines designed to stimulate the immune system to attack prostate cancer cells, as well as checkpoint inhibitors that release the brakes on immune cells.
While these treatments aren’t yet mainstream for prostate cancer, ongoing trials offer hope—especially for advanced or resistant cases.
➤ Lifestyle and Prevention: Can You Influence Your Risk?
Here’s a question everyone wants answered: Is there anything I can do to prevent prostate cancer?
The short answer: there’s no guaranteed way to prevent it. But research suggests that lifestyle matters.
A diet rich in fruits, vegetables, and healthy fats—think Mediterranean-style eating—may reduce risk or slow progression. Regular exercise, maintaining a healthy weight, and avoiding smoking also help.
Some studies have looked at supplements like vitamin D or selenium, but results are mixed. Talk to your doctor before starting anything new.
➤ What Does the Future Hold?
The future of prostate cancer care looks promising:
- Earlier, more accurate detection using liquid biopsies (blood tests that detect tumor DNA).
- Highly personalized therapies based on individual genetic profiles.
- Expanded access to care through telemedicine and community programs.
- Greater focus on quality of life and managing long-term side effects.
➤ What Should You Take Away from This?
Science is moving fast, but it can feel overwhelming.
Here’s what’s most important:
- Know your risk. Age, family history, ethnicity, and genetics all matter.
- Stay informed. Screening guidelines evolve, and new tests emerge.
- Talk to your doctor. Share your history and concerns.
- Advocate. Whether for yourself or loved ones, don’t hesitate to ask questions or seek second opinions.
And remember: behind every clinical trial and breakthrough are stories like Ben Stiller’s and Rod Stewart’s—people who chose awareness over silence, action over fear.
Your journey may never be headline news, but it’s no less important.
FAQ: What You Really Want to Know About Prostate Cancer
Let’s be honest—there’s a lot of confusing, sometimes contradictory information out there about prostate cancer. So before we wrap up, let’s clear the air on some of the most frequently asked questions. Consider this your go-to quick reference, but with enough depth to truly satisfy your curiosity.
1. What are the early signs of prostate cancer?
You might expect a clear, dramatic set of symptoms—like pain or a noticeable lump—but prostate cancer often doesn’tcause any symptoms early on. That’s part of what makes it so tricky. When symptoms do appear, they can include urinary difficulties such as weak stream, frequent urination (especially at night), blood in urine or semen, or discomfort in the pelvic area. However, these symptoms can also be caused by benign conditions like prostatitis or an enlarged prostate. This is why screening and regular checkups are so important.
2. At what age should men start getting screened for prostate cancer?
This is a nuanced question with evolving answers. Most guidelines suggest starting discussions about screening at age 50 for average-risk men. If you have a family history of prostate cancer or are African American—both groups at higher risk—starting at 45 or even 40 may be appropriate. Importantly, screening is a decision, not a mandate; it involves weighing risks like overdiagnosis against the benefits of early detection. The best approach is an informed conversation with your healthcare provider tailored to your individual risk factors.
3. How reliable is the PSA test? Should I be worried about false positives?
PSA testing is a powerful tool, but it’s not perfect. Elevated PSA levels don’t always mean cancer; infections, inflammation, or even recent ejaculation can cause spikes. Conversely, some cancers don’t raise PSA levels significantly. That’s why doctors use PSA as part of a broader diagnostic toolkit, often combining it with digital rectal exams and imaging like MRI. If a PSA test is abnormal, it usually leads to further tests—not immediate diagnosis.
4. If diagnosed, what are my treatment options?
Treatment depends heavily on cancer grade, stage, patient age, and overall health. For low-risk, localized prostate cancer, active surveillance (regular monitoring without immediate treatment) is increasingly common, minimizing side effects. More aggressive cancers may require surgery (removing the prostate), radiation therapy, hormone therapy, or a combination. Newer options like focal therapies and immunotherapies are emerging. Importantly, side effects—like urinary incontinence and erectile dysfunction—vary by treatment type and individual.
5. Can prostate cancer be cured?
Absolutely. Many prostate cancers, especially those caught early, are curable. The 5-year survival rate for localized prostate cancer is nearly 100%. Even with more advanced disease, treatments can extend life significantly and maintain quality of life. The key takeaway? Early detection and personalized care can make a life-saving difference.
6. Why is prostate cancer more common and more deadly among Black men?
This is a critically important and complex issue. Genetics play a role, but social determinants of health—like disparities in access to care, socioeconomic factors, and systemic bias—also contribute. Black men are often diagnosed at a later stage and receive less aggressive treatment. Efforts to improve education, screening access, and culturally sensitive care are essential to closing this gap.
A Final Word
Prostate cancer touches many lives—public and private alike. The stories of celebrities who have faced this disease remind us that it can happen to anyone, but also that early detection and informed choices can change the outcome dramatically.
This article aimed to give you a complete picture: the science, the personal journeys, the cultural shifts, and the resources available. But ultimately, the most important step is yours. Whether it’s having that sometimes awkward conversation with a doctor, encouraging a loved one to get screened, or simply staying informed, your actions matter.
Remember: knowledge is not just power—it’s hope. And hope is the foundation of every story that ends in survival, resilience, and renewed life.
Thank you for taking the time to learn, reflect, and engage. Here’s to health, awareness, and the courage to face what lies ahead—together.












