Can Rebounding Spread Cancer? Safety and Benefits Explained
- Foreword: Can Something So Simple Be That Risky?
- 1. Understanding Rebounding: More Than Just Jumping Around
- 2. The Lymphatic System and Cancer: What’s Moving, and Why It Matters
- 3. Rebounding and Lymphatic Circulation: What Happens When You Bounce?
- 4. Addressing the Concern: Can Rebounding Spread Cancer?
- 5. Benefits of Rebounding for Cancer Patients: More Than Just a Bounce
- 6. Guidelines for Safe Rebounding: How to Bounce Without Breaking
- 8. Integrating Rebounding into Cancer Care Plans: Making Movement Work for You
- 9. Frequently Asked Questions (FAQs)
- Closing Thoughts: Bouncing Forward With Confidence
Foreword: Can Something So Simple Be That Risky?
If you’ve landed here, you’ve likely come across the concept of rebounding—a deceptively gentle form of exercise involving a mini-trampoline—and you’re wondering: Is this safe for someone with cancer? Could it actually help, or could it do harm? Might it even accelerate the spread of cancer?
These are not idle questions. They’re intelligent, responsible, and surprisingly common.
As cancer patients or caregivers, you’re faced with a barrage of contradictory advice. One source tells you to rest, another to move. Some wellness blogs tout rebounding as a miracle detoxifier. Others whisper ominously about its potential to “stimulate metastasis.” Caught in the crossfire of hope and fear, how do you sort the science from the pseudoscience?
This article aims to be your final stop on the topic. We’re going to go deep—not just skim the surface. We’ll explore the mechanics of rebounding, the biology of the lymphatic system, how cancer spreads, and what medical literature actually says about this unique form of exercise. You’ll get a guided tour of both hope and caution, with clarity as the destination.
Is it safe to bounce with cancer? Let’s find out—grounded in science, not hearsay.
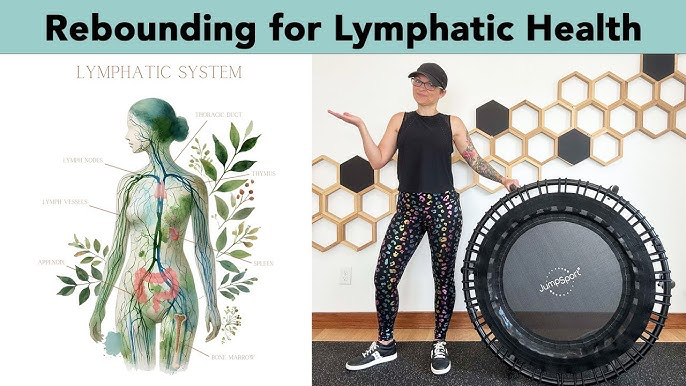
Understanding Rebounding: More Than Just Jumping Around
Let’s start by clearing up a basic question: What exactly is rebounding?
Rebounding is a low-impact aerobic exercise performed on a mini-trampoline, also known as a rebounder. Unlike high-intensity jumping, rebounding typically involves gentle vertical movement—more of a rhythmic bounce than a gymnastic launch. It can be as vigorous as jumping jacks or as subtle as standing and gently shifting your weight.

And it’s not new. The concept dates back to the 1970s when NASA famously studied rebounding to help astronauts recover bone density and muscle mass after spaceflight. Why a trampoline? Because it offers gravitational variation—a kind of mechanical stimulation that affects your muscles, bones, and yes, your lymphatic system.
Why Has Rebounding Captured Attention in the Cancer Community? Much of it has to do with the lymphatic system, a core part of your immune infrastructure—and something we’ll explore more in the next section. For now, know this: unlike your circulatory system, your lymphatic system doesn’t have a central pump like the heart. It relies on muscle contractions and body movement to move lymph fluid through its network. Rebounding, proponents claim, is one of the most efficient ways to stimulate this motion.
But therein lies the concern.
Some worry that by stimulating lymphatic flow, you might also stimulate the spread of cancer—particularly cancers that have invaded the lymph nodes or are prone to metastasize via lymphatic vessels. The logic is not unreasonable, especially for those dealing with malignancies like breast, melanoma, or lymphoma. It feels intuitive that “moving stuff around” might include “moving cancer cells around.”
So, does it?
Before we jump (pun intended) to conclusions, we need to understand how rebounding actually interacts with the body. Is this just another fitness fad, or is there a deeper physiological reality behind it? More importantly, are those physiological changes a benefit or a liability to someone facing a cancer diagnosis?
As we move forward, we’ll tackle this with the seriousness it deserves—and the clarity you need. You’ll understand not just what rebounding does, but how it fits (or doesn’t) into a cancer recovery plan. Spoiler: the answer isn’t one-size-fits-all.
So hang on—because what comes next will reshape how you view one of the simplest, strangest, and potentially most powerful tools in the exercise toolbox.
Rebounding (mini-trampoline workouts) sometimes raises concerns among cancer patients, especially those post-surgery. If you’re wondering about actual spread patterns, How Breast Cancer Travels to the Liver and Skin offers clinical perspective.
The Lymphatic System and Cancer: What’s Moving, and Why It Matters
To really understand whether rebounding poses a risk—or offers a benefit—we have to take a step back and look at the system it most directly influences: your lymphatic system.

You’ve probably heard the term before, especially if cancer has touched your life. Maybe your oncologist mentioned lymph nodes during staging. Maybe your scans showed “lymphatic involvement.” But what is this system, and why does it matter so much in cancer—and in rebounding?
Let’s break it down.
What Exactly Is the Lymphatic System?
Think of the lymphatic system as your body’s second circulatory system. It runs in parallel to your blood vessels but carries a very different cargo: a clear, slightly yellow fluid called lymph. This fluid contains immune cells (mostly lymphocytes), proteins, fats, and cellular debris. It also serves as a garbage collection and surveillance network, sweeping up potential threats—bacteria, viruses, damaged cells—and delivering them to your lymph nodes for inspection.
And it’s vast. You’ve got hundreds of lymph nodes—tiny, bean-shaped filters—connected by a network of vessels that reach nearly every corner of your body.
Here’s the key detail: there’s no central pump. Your blood has the heart to keep it circulating. Lymph? It relies on you—your muscle movements, your breathing, your body’s position in space.
This is where rebounding comes in. Every time you bounce, even just a little, you’re creating a shift in gravitational forces—an acceleration and deceleration that milks your lymph vessels. It’s a passive-active flow boost, a kind of manual lymph drainage powered by motion. This is why some physical therapists and cancer rehab specialists advocate for rebounding, especially in the context of lymphedema prevention.
But here’s where things get complicated.
How Does Cancer Interact With the Lymphatic System?
Certain cancers—breast, melanoma, prostate, lung, gastrointestinal, and lymphomas, just to name a few—often spread through the lymphatic system. This process is called lymphatic metastasis. Cancer cells can detach from the primary tumor, hitch a ride in the lymph fluid, and lodge themselves in nearby lymph nodes or even distant organs.
This is why doctors check lymph nodes during cancer staging. If the nodes are clear, the cancer is more likely localized. If they’re positive, it’s a red flag for systemic spread. Hence the concern: If you stimulate the lymphatic system, are you encouraging those cells to move?
It’s a valid question. And to answer it, we need to look at a few things.
Here’s the uncomfortable truth: we don’t know if moving lymph moves cancer. But we do have some strong clues.
The spread of cancer through the lymphatics is not a purely mechanical process. It’s not as simple as “jostle the body, scatter the cancer.” Metastasis is biologically complex. Cancer cells that metastasize must undergo changes in gene expression, evade immune detection, survive physical transport, and then stick the landing in a new tissue environment that will support their growth.
So while lymph movement may technically help cancer cells travel, it’s not the main limiter in whether metastasis happens. Think of it like this: if cancer cells are trying to move cities, the lymph flow is the road—but metastasis is more like hijacking a truck, crossing multiple borders, bribing officials, and setting up shop in a new building.
In other words, stimulating lymphatic flow might make the highway smoother, but the cancer still has to be a very capable fugitive to exploit that road.
Here’s the reassuring part: there is no evidence that rebounding, or any form of light to moderate exercise, increases the risk of cancer metastasis. In fact, most studies on physical activity and cancer show the opposite—exercise is associated with better outcomes in many cancers, including lower recurrence rates and longer survival.
A 2019 review in JAMA Oncology found that physical activity after diagnosis was associated with a 27% lower risk of cancer-specific mortality. Another study in Nature Reviews Cancer explained how exercise modulates inflammation, immunity, and even the tumor microenvironment in ways that may inhibit cancer spread.
As for rebounding specifically? The research is thinner, but not nonexistent. Some physical therapists use mini-trampolines for gentle rehab in cancer survivors. There’s anecdotal support and small pilot studies suggesting benefits for lymphatic drainage and quality of life. But large-scale randomized trials? Not yet.
So are the concerns entirely unfounded? Not quite. In certain rare scenarios—such as with unstable tumors near large lymphatic structures or during acute post-surgical recovery—it might be wise to avoid vigorous bouncing. But for the average cancer patient under medical supervision, rebounding in moderation doesn’t appear to pose any more risk than walking or swimming.
You’re smart to be cautious. And you’re smarter still to ask nuanced questions instead of settling for feel-good fitness slogans. The lymphatic system is deeply involved in cancer—but also in recovery, immunity, and healing. Rebounding affects that system—but so does every form of movement.
If you’re still unsure, don’t worry. We’re not done yet. Next, we’ll look at how rebounding influences lymphatic circulation, what that means practically, and how to navigate it safely if you’re dealing with cancer.
Let’s keep going. You’re not just bouncing—you’re building understanding.
Rebounding and Lymphatic Circulation: What Happens When You Bounce?
Now that we understand the vital role of the lymphatic system—both in defending against cancer and in how cancer can spread—let’s return to the trampoline. What actually happens inside your body when you bounce? And how does this movement influence the complex network of lymphatic vessels running throughout you?
This isn’t just idle curiosity. It’s central to answering the big question: can rebounding help your body heal, harm it, or possibly both?
When you rebound, even gently, your body experiences alternating phases of acceleration and deceleration. At the peak of your bounce, you experience a brief feeling of near-weightlessness, while at the bottom, as you land, gravitational forces intensify. This dynamic creates what you might call a mini gravitational massage. Each time your feet hit the trampoline surface, your muscles compress and stretch, your circulation improves, and most importantly, your lymph vessels are rhythmically squeezed open and shut.
This mechanical action is crucial because, unlike your circulatory system, your lymphatic system doesn’t have a pump like the heart to move fluid. Instead, it relies heavily on muscle contractions and body movements to push lymph through its vessels. Rebounding creates exactly the kind of stimulation that promotes efficient lymph flow. And unlike high-impact activities such as running or jumping, rebounding is gentle on your joints, making it accessible even if you’re coping with fatigue, recovering from surgery, or experiencing neuropathy.
So mechanically speaking, rebounding is one of the most effective ways to support lymphatic circulation.
Why is this so important, especially for cancer patients? Lymphatic stagnation can lead to serious complications. For instance, many patients who have lymph nodes removed during cancer surgery develop lymphedema, a painful and often debilitating buildup of lymph fluid. Radiation therapy can worsen this by causing scarring in the lymph vessels. In these scenarios, anything that gently promotes lymph flow can be invaluable.
Beyond fluid drainage, the lymphatic system is integral to immune function. It’s the training ground and deployment center for immune cells, tasked with detecting and eliminating harmful invaders, including rogue cancer cells. Efficient lymphatic circulation ensures that immune surveillance is effective and inflammation is resolved quickly. Whether you are undergoing treatment, recovering, or in remission, supporting your lymphatic system isn’t just helpful—it’s a cornerstone of comprehensive oncology care.
That said, it’s natural to ask: can too much lymphatic stimulation backfire? The answer is nuanced. In some rare cases, tumors may have invaded the lymphatic vessels extensively. In these situations—especially if the tumor is still active—vigorous movement that sharply increases lymph flow might cause problems. But this is about timing and context, not a condemnation of rebounding itself.
For example, immediately after surgery or biopsy, it might be wise to avoid bouncing for a short period. During chemotherapy, gentle movement is encouraged, but intensity should be moderated. In cases of bone metastases or severe fatigue, alternatives to rebounding may be better suited. On the other hand, during stable remission, rebounding could be one of the most beneficial exercises.
Ultimately, individualized care is paramount. Every cancer and patient is different, and exercise must be tailored accordingly.
Interestingly, the most effective way to rebound for lymphatic health might surprise you. It’s not about high jumps or vigorous activity but rather the “health bounce”—a simple, gentle up-and-down motion where your feet barely leave the mat. This deceptively easy movement activates deep muscular and lymphatic pathways throughout the body without undue strain. Even just one minute can warm you up, loosen your muscles, and “wake” your lymphatic system.
So is rebounding a lymphatic superpower or a double-edged sword? The truth lies somewhere in between. Used wisely and with medical guidance, rebounding can enhance immune circulation, reduce lymphedema risk, support detoxification, and improve mood and energy through gentle motion. Used recklessly, especially during vulnerable periods, it might pose risks—but these are situational, not inherent to rebounding itself.
There’s also ongoing interest in terrain theory and metabolic risk, both of which are unpacked in The Metabolic Approach to Cancer.
If you’re wondering whether you should be rebounding, the better question is: when, how, and under what guidance? We’ll explore that next, along with what the scientific and medical experts say about rebounding and cancer spread. It’s time to confront the core fear head-on: does bouncing actually spread cancer? Let’s face that question with data and clarity, not with anxiety.
Addressing the Concern: Can Rebounding Spread Cancer?
Now, let’s confront the question that likely brought many readers here in the first place: can rebounding actually spread cancer? If you’ve followed along so far, you may have noticed the growing interest in rebounding—not only as a form of fitness but also as a tool for recovery, lymphatic support, and emotional well-being. Yet beneath this promise often lies a nagging fear: am I unintentionally doing something risky? Could bouncing on a mini-trampoline somehow encourage cancer cells to spread?
This is a fair and reasonable concern. After all, it stems from two well-known facts: some cancers do spread via the lymphatic system, and rebounding is known to increase lymphatic flow. When you place those two facts side by side, it’s easy to see why the leap to worry feels almost inevitable. If cancer cells travel in lymph fluid, and rebounding accelerates lymph movement, does it not follow that rebounding might “help” cancer spread?
But biology is rarely so simple. Cancer metastasis—the process by which malignant cells spread to other parts of the body—is far more complex and highly selective than a mere matter of fluid transport. For a cancer cell to metastasize via the lymphatic system, it must detach from the primary tumor, evade immune detection, penetrate the lymph vessel walls, survive the journey through lymph fluid, bypass or survive filtering at lymph nodes (which are specifically designed to trap and destroy such cells), exit the node, re-enter circulation, and finally find a hospitable environment in a distant organ where it can grow. Each step involves numerous biological barriers and cellular adaptations.
Therefore, while rebounding does increase lymph flow, this alone does not guarantee—or even necessarily promote—metastasis. In fact, many everyday activities such as walking, stretching, and even deep breathing also enhance lymphatic circulation without causing cancer spread. If simply moving lymph fluid were enough to promote metastasis, then normal daily life would pose the same risk.
What does the scientific research say? Large bodies of evidence consistently show that moderate physical activity after a cancer diagnosis is associated with lower recurrence rates and improved survival across various cancer types including breast, colon, and prostate. Exercise improves immune surveillance, reduces systemic inflammation, and helps normalize tissue oxygenation, creating an environment less hospitable to cancer progression. Importantly, systematic reviews find no clinical evidence that gentle exercise accelerates disease progression—even in patients with lymphatic involvement.
If rebounding truly caused harm by spreading cancer, oncologists and rehabilitation specialists would not be quietly recommending it as part of survivorship care. Of course, this doesn’t mean rebounding is universally safe for every individual or at every stage. Timing, intensity, and personal health factors matter greatly.
You may have encountered anecdotal warnings—stories online of people claiming their cancer recurred after starting rebounding. While such stories can be frightening, it is crucial to remember that correlation does not imply causation. Cancer recurrence often follows an unpredictable timetable, and coincidental timing with an activity doesn’t prove it caused the event. In fact, movements that promote circulation, immune function, and mental clarity are far more likely to be allies than adversaries in the healing process.
That said, there are circumstances when rebounding or any vigorous movement should be approached with caution. Immediately following surgery—particularly when lymph nodes have been removed or irradiated—rest and healing are priorities. Patients with bone metastases may risk fractures from impact, even low-impact. Severe fatigue or low blood counts can make any exercise overwhelming or unsafe. Active disease in lymph-rich areas can cause discomfort or strain with aggressive movement.
Ultimately, these concerns highlight the importance of individualized care rather than outright avoidance. Any new exercise regimen, including rebounding, should be discussed with your oncology team and ideally coordinated with physical therapists or rehabilitation specialists who understand your unique health profile.
So, what’s the bottom line? Current scientific evidence provides no solid basis to believe that rebounding spreads cancer. On the contrary, light-to-moderate physical activity supports healing and overall wellbeing. When done thoughtfully and under appropriate guidance, rebounding can safely enhance lymphatic function and improve quality of life.
Does this mean you should rush out and buy a mini-trampoline tomorrow? Not necessarily. But it does mean that fear alone should not keep you from exploring movement that your body needs and thrives upon. Cancer, despite its complexity, does not get the final say in how you live.
Next, we’ll explore the benefits of rebounding more deeply, particularly for those living with or recovering from cancer. From detoxification and vitality to emotional resilience, there’s much more to discover.
Let me know if you’d like me to continue with Part 5 or make any adjustments!
Benefits of Rebounding for Cancer Patients: More Than Just a Bounce
By now, you’re probably wondering: Okay, rebounding doesn’t spread cancer—but what good does it actually do? After all, it’s not just about safety; it’s about real, tangible benefits, especially when you’re navigating cancer treatment or recovery.
So, what makes rebounding more than a fun pastime or a quirky fitness trend? Let’s dig into why so many healthcare professionals and survivors swear by it—and why it might just be a game-changer for you.
Physical Benefits: Gentle, Effective, and Accessible
First off, rebounding is an excellent low-impact cardiovascular workout. For many cancer patients, high-impact exercises like running or jumping rope are off the table due to fatigue, joint pain, or bone health concerns. Rebounding offers a middle ground—an aerobic workout that raises your heart rate without stressing your knees, hips, or spine.
You might ask, “But can gentle bouncing really help build strength or stamina?” The answer: yes, absolutely. The constant mini gravitational shifts engage your core muscles, calves, glutes, and even your arms if you incorporate light movements. It also improves balance and coordination, which can deteriorate during cancer treatment or as a result of neuropathy.
What’s more, rebounding stimulates bone density. This is vital because many cancer treatments—like chemotherapy or hormone therapy—can cause bone thinning or osteoporosis. NASA’s original interest in rebounding was for astronauts who lose bone mass in zero gravity. Your mini-trampoline is like a portable, home-friendly gravity trainer.
Lymphatic and Immune System Boost
We’ve already talked a lot about lymphatic flow, but it bears repeating: Rebounding is one of the most effective ways to stimulate your lymphatic system. Unlike your heart, the lymph system has no pump; it relies on movement to push fluid through your vessels and nodes.
Why does this matter? Because efficient lymph drainage helps reduce swelling, flush toxins, and supports immune surveillance—all critical for cancer recovery and overall health. It can be especially helpful for patients prone to lymphedema after lymph node removal or radiation therapy.
Many cancer survivors report that gentle rebounding sessions help them feel lighter, less swollen, and more energized. This isn’t just anecdotal; physical therapists often incorporate rebounders into post-treatment rehab.
Psychological and Emotional Lift: Mood, Motivation, and Mental Clarity
Let’s face it: cancer isn’t just a physical battle; it’s an emotional and psychological rollercoaster. Fatigue, anxiety, depression, and “chemo brain” are all too common.
Here’s where rebounding offers another superpower: it releases endorphins and serotonin, those feel-good brain chemicals that can lift mood and reduce stress. The rhythmic, almost meditative bounce can be a form of active mindfulness—helping to break cycles of rumination or anxiety.
And because rebounding is easy to start, even short sessions provide a quick confidence boost. That sense of accomplishment—I moved, I did something good for myself—can snowball into a more positive mindset and increased motivation to keep going.
Practicality and Adaptability: Exercise on Your Terms
One of the best things about rebounding is how adaptable it is. You can do it:
- At home, on your schedule
- While watching TV or listening to music or podcasts
- For just a few minutes a day, with options to increase as you feel stronger
- Sitting, standing, or holding onto a support bar for balance
For those dealing with fatigue or balance issues, you can start with gentle health bounces or even seated rebounding (moving feet gently on the trampoline while sitting). Over time, you can build up to longer or more vigorous sessions.
In other words, rebounding meets you where you are—not the other way around.
What About Detoxification? Is It a Real Thing?
You might have heard claims that rebounding “detoxifies” the body by accelerating lymph flow and flushing waste. Is this scientific fact or health hype?
It’s both, in a way.
While “detox” is often overused and oversimplified, it’s true that your lymphatic system plays a key role in removing cellular debris, pathogens, and metabolic waste from tissues. When lymph circulation improves, this cleansing process is more efficient.
That said, rebounding is one part of a bigger puzzle: hydration, nutrition, sleep, and stress management also matter greatly. So don’t think of the trampoline as a magic detox machine—but rather as a valuable tool to support your body’s natural waste management system.
Is There Evidence From Real Patients?
Absolutely. Survivors from breast cancer to lymphoma to colorectal cancer have shared how rebounding helped them regain strength, improve mobility, and boost mood.
Physical therapists specializing in oncology rehab frequently include rebounding in their programs. Some even use it as a tool to reduce lymphedema symptoms or improve balance post-treatment.
While more large-scale clinical trials are needed to nail down exact protocols and benefits, the current body of evidence and patient experience is promising.
Guidelines for Safe Rebounding: How to Bounce Without Breaking
Rebounding can be a powerful tool for people recovering from cancer—but like any potent therapy, it requires respect and care. You might be wondering, how do I start safely? How hard should I bounce? What signs should I watch out for? These are excellent questions, and the answers matter greatly—not only for your safety but also to ensure you gain the maximum benefits from your practice.
1. Always Check with Your Medical Team First
This isn’t just a polite suggestion; it’s a fundamental safety measure. Your oncologist, physical therapist, or rehabilitation specialist understands your diagnosis, treatment plan, and current physical condition in detail. They can guide you on whether rebounding is appropriate at this stage or if it’s better to wait until your body has healed further. If you have undergone surgery involving lymph nodes, radiation to sensitive areas, have bone metastases, or experience treatment side effects like neuropathy, fatigue, or abnormal blood counts, getting their approval is essential before you start.
2. Start Slow and Embrace the Health Bounce
Once you have the go-ahead, start slow. You don’t need to jump around like a child at a trampoline park to see benefits. The health bounce involves a gentle, rhythmic up-and-down motion where your feet barely leave the mat. This low-impact movement is easy on your joints and muscles yet effectively stimulates lymph flow and gently raises your heart rate. Begin with one to two minutes per session, and as your energy and confidence improve, gradually increase to five to ten minutes daily.
3. Pay Attention to Your Body’s Signals
Rebounding should never cause pain, dizziness, or excessive fatigue. If you experience any sharp pain, swelling, shortness of breath, or chest tightness, stop immediately and consult your healthcare provider. Fatigue can be tricky—some tiredness after exercise is normal, but rebounding shouldn’t leave you completely drained for the rest of the day.
4. Use Support if Needed
Balance can be challenging during and after cancer treatment, especially if you have neuropathy or muscle weakness. Many rebounders come equipped with support bars or handles—use them! Holding onto a stable support can help prevent falls and boost your confidence. If your rebounder lacks a support bar, consider positioning it near a sturdy countertop or wall for added balance assistance.
5. Ensure Proper Equipment Setup
Your mini-trampoline should be sturdy and designed specifically for rebounding, with an adequate weight rating. Place it on a flat, non-slip surface, and check that it’s clean and free of damage. If balance is a concern, a support bar is highly recommended. Regularly review the manufacturer’s guidelines for weight limits and maintenance to keep your rebounder safe and enjoyable.
6. Combine Rebounding with Other Movements and Recovery Practices
While rebounding is a powerful exercise tool, it should be part of a broader recovery routine. Complement it with gentle stretching to maintain flexibility, breathing exercises to boost oxygenation and calm your nervous system, proper hydration and nutrition to support healing, and plenty of rest and sleep. This holistic approach amplifies the benefits of rebounding and helps prevent overexertion.
7. Be Mindful of Timing in Your Treatment Cycle
Certain phases of cancer treatment may require you to pause or modify your rebounding routine. For example, during active chemotherapy cycles when energy and immune function may be low, immediately following surgery or radiation sessions, or if your blood counts—like platelets or white blood cells—are dangerously low, it’s best to consult your care team. They can help you recognize these windows and advise you on when and how to safely resume.
8. Track Your Progress and Adjust
Keeping a simple journal noting how long you rebound, how you feel before, during, and after sessions, and any symptoms or side effects helps you adjust your routine thoughtfully. It also provides your medical team with important feedback to optimize your care.
9. Stay Educated and Stay Connected
Cancer care and exercise science continually evolve, so keep up to date on the latest research and recommendations. Joining cancer survivor support groups or online communities focused on fitness and wellness can offer motivation, insights, and camaraderie. Hearing how others have successfully integrated rebounding into their recovery can be inspiring and reassuring.
Worried about exacerbating things? It may be worth comparing the mechanics of movement with Dense Dose Chemotherapy Protocols, which often impact muscle recovery and lymphatic load.
So, what’s your next step? If you’re ready, begin slowly with the health bounce after getting your doctor’s approval. Set up your rebounder in a safe place with appropriate support, and always listen to your body. Remember, rebounding isn’t about perfection or high performance—it’s about movement as medicine, done with respect for where you are today.
Integrating Rebounding into Cancer Care Plans: Making Movement Work for You
You’ve learned what rebounding is, why the lymphatic system matters, the safety considerations, and heard real stories of how it helps. Now comes the big question: How do you weave rebounding into your cancer care routine in a way that’s effective, safe, and sustainable?
This part is about integration—not just bouncing in isolation, but making rebounding a smart part of your holistic approach to wellness.
Why Integration Matters
Cancer treatment isn’t a one-dimensional battle; it’s a marathon with many moving parts. You have chemotherapy or radiation schedules, nutrition plans, symptom management, emotional support, and physical rehabilitation. Each piece affects the others.
If rebounding is going to be part of this mix, it needs to fit your unique situation and goals. It can’t be a generic “exercise prescription.” It must be customized.
You might wonder: Is it realistic to add another thing to my plate?
Or, How can I know if I’m doing more good than harm?
Those concerns are valid and deserve thoughtful answers.
Collaborate With Your Care Team
The cornerstone of integration is communication.
Talk openly with your oncologist, physical therapist, and any rehab specialists. Share your interest in rebounding and ask for their input on timing, intensity, and precautions.
If you don’t have a rehab team, consider asking your oncology nurse or primary care provider for referrals. Many centers now offer cancer rehabilitation programs tailored to patient needs.
Remember: you’re the expert on your body and experience, but your care team provides essential medical guidance. Together, you’ll find the safest path forward.
Build Rebounding Into a Balanced Routine
Rebounding is best used alongside other supportive practices:
- Strength Training: Resistance exercises help rebuild muscle lost during treatment. Rebounding complements this by improving cardiovascular health and lymphatic flow.
- Flexibility and Stretching: Keeping muscles and joints supple reduces stiffness and injury risk.
- Mind-Body Practices: Yoga, tai chi, or meditation can enhance mental resilience and reduce stress. Rebounding’s rhythmic motion can feel meditative too, creating synergy.
- Nutrition and Hydration: Fueling your body well amplifies recovery and exercise benefits.
- Rest: Sleep and rest are non-negotiable. Rebounding should energize, not exhaust you.
Together, these create a holistic ecosystem of healing.
Adapt as You Go
Cancer care is dynamic. Your energy levels, symptoms, and treatment phase will ebb and flow.
This means your rebounding routine should be fluid, not rigid. Some days might be perfect for 15 minutes; others, just a gentle 2-minute health bounce. That’s okay.
Tracking how you feel after sessions helps you adjust intelligently. Over time, you’ll develop a sense of your own “bounce rhythm”—the pace that supports your body best.
Set Realistic Goals
You don’t need to train for a marathon or become a fitness influencer. The goal is movement that supports healing and quality of life.
This might mean improving balance to prevent falls, reducing swelling in an affected limb, or simply reclaiming a sense of vitality and control.
Celebrate the small wins. Maybe it’s fewer moments of brain fog, better sleep, or just the pleasure of movement after weeks of inactivity.
When to Pause or Modify
Certain red flags mean it’s time to stop and seek advice:
- New or worsening pain
- Sudden swelling or bruising
- Dizziness or shortness of breath
- Severe fatigue or malaise lasting beyond a day after rebounding
These don’t mean rebounding is “bad,” but they signal that your body needs a reset or that your routine needs tweaking.
Leveraging Technology and Support
Many patients find that using apps or wearable trackers helps keep them motivated and safe. Simple reminders to hydrate, short session timers, or gentle progress tracking can make a difference.
Online communities or local cancer wellness groups can offer encouragement and shared knowledge. The journey is easier when you know you’re not alone.
The Takeaway: Rebounding as a Living Practice
Rebounding isn’t a prescription you follow once and forget. It’s a living practice, evolving with your needs, treatments, and goals.
By integrating it mindfully, you harness not just the physical benefits but the psychological and emotional uplift that movement provides.
Your cancer care is a complex, personal journey—and rebounding can be a surprisingly effective companion on the road to recovery and beyond.
Let me know if you want me to continue or adjust anything!
Frequently Asked Questions (FAQs)
Navigating exercise during cancer treatment can be confusing, and rebounding is no exception. You likely have questions—some practical, some nuanced. Let’s tackle the most common ones, head-on, with clear, evidence-informed answers. If your question isn’t here, feel free to ask anytime!
1. Is rebounding safe for all types of cancer?
Great question. The short answer: usually yes, but context matters. Most cancers do not prohibit gentle physical activity like rebounding. However, cancers involving bone metastases, active tumors in lymphatic-rich regions, or severe treatment side effects may require tailored approaches or temporary avoidance. Always consult your oncologist before starting.
2. How often should a cancer patient engage in rebounding exercises?
Frequency depends on your energy, treatment phase, and medical advice. For many, starting with just a few minutes daily and gradually increasing to 10–15 minutes works well. Consistency matters more than intensity. Even short, daily sessions stimulate lymph flow and improve mood.
3. Can rebounding replace other forms of physical therapy?
No. While rebounding is excellent for cardiovascular fitness, lymphatic stimulation, and balance, it’s not a substitute for specialized physical therapy targeting strength, flexibility, or rehabilitation from surgery or neuropathy. Think of it as a complementary tool within a broader rehab plan.
4. Are there specific rebounders recommended for cancer patients?
Look for sturdy mini-trampolines designed for exercise, ideally with a support bar if balance is a concern. Size matters—too small can feel unstable; too large may be unwieldy in a home setting. Brands with good reviews from cancer rehab professionals are a plus. Avoid cheap, low-quality models that might compromise safety.
5. What precautions should be taken during rebounding sessions?
Monitor your body’s response and adjust accordingly
Start slow with health bounces before attempting higher impact
Use a support bar or stable surface for balance
Stop immediately if you feel pain, dizziness, or unusual symptoms
Avoid rebounding right after surgery or during acute treatment side effects without medical clearance
Stay hydrated and wear supportive footwear or go barefoot if the surface allows
7. Is there a risk of injury or falls while rebounding?
Like any exercise, there’s some risk—especially if you have balance or neuropathy issues. Using a support bar, starting slowly, and ensuring a safe setup dramatically reduce risk. If you’re concerned, consider supervised sessions with a physical therapist initially.
Closing Thoughts: Bouncing Forward With Confidence
We’ve covered a lot of ground together—from understanding the lymphatic system and how cancer spreads, to addressing the common fear that rebounding might accelerate metastasis, and finally exploring the real benefits, safety considerations, and personal experiences related to rebounding during cancer treatment. By now, you have a clear, evidence-based picture of how rebounding fits into the broader context of cancer care. It’s a journey that blends science, personal insight, and practical wisdom.
Rebounding is not a cure for cancer, nor should it replace any medical treatment prescribed by your oncologist. However, it offers a uniquely accessible way to support your body’s natural healing processes, improve cardiovascular fitness, stimulate lymphatic flow, and boost mood and balance. It’s a holistic form of movement that engages both body and mind, helping many regain a sense of control and well-being during a challenging time. While this might sound optimistic, it’s well supported by research and real-world patient stories.
Understandably, the fear that rebounding could “stir up” cancer cells and spread the disease is one of the biggest barriers for patients considering this activity. Yet, cancer metastasis is a highly complex biological process, not simply a matter of physically moving lymph fluid faster. The scientific consensus is that moderate, appropriate physical activity—including rebounding—is safe and beneficial for most patients. Your body thrives on movement, and the key lies in how and when you move, rather than avoiding movement altogether out of fear.
The path forward involves trusting both your body’s signals and the expertise of your medical team. Everyone’s cancer journey is different, which means rebounding routines must be personalized. Starting slowly, paying close attention to how your body responds, and maintaining open communication with healthcare providers ensures you use rebounding as a safe and supportive tool. Celebrate small milestones—whether that’s bouncing a little longer, feeling less swollen, or simply enjoying the mental lift that comes with movement.
Remember, rebounding is just one piece of a larger puzzle. Alongside good nutrition, adequate rest, stress management, and your prescribed treatments, it can enhance overall wellness. There’s no pressure to become an exercise enthusiast overnight; even gentle, short bouts of rebounding can offer meaningful benefits. Taking this simple step can be an act of hope and self-care.
In the end, cancer tests us in every dimension—physically, emotionally, and mentally. But within that challenge lies opportunity. Choosing to engage with movement, to educate yourself, and to participate actively in your recovery are powerful decisions. Rebounding, with its literal and metaphorical spring-back, symbolizes resilience—the ability to recover, find balance, and move forward even when the road is uncertain.
If you feel ready, it’s time to bounce—with intention, courage, and confidence.










