Can Dental X-Rays Detect Cancer? What They Reveal and Miss
- Foreword: Why This Question Matters More Than You Think
- 1. Understanding Dental X-Rays: What They Are and How They Work
- 2. The Basics of Oral Cancer: What You’re Actually Hoping Dental X-Rays Might Catch
- 3. Can Dental X-Rays Detect Cancer? Here’s the Honest, Nuanced Answer
- 4. When X-Rays Aren’t Enough: What Happens When We Need to Look Deeper
- 5. The Dentist’s Role in Cancer Detection: More Than Just Teeth Cleaning
- 6. The Risks of Dental X-Rays: Should You Be Worried About Radiation?
- 7. Innovations in Dental Imaging: How Technology Is Changing the Game
- 8. Patient Empowerment and Education: Taking Control of Your Oral Health
- 9. Frequently Asked Questions (FAQs)
- Closing Thoughts: What You Should Take Away About Dental X-Rays and Cancer Detection
- Final Thought
Foreword: Why This Question Matters More Than You Think
Imagine sitting in the dentist’s chair, that familiar bitewing tab tucked in your cheek, as the technician steps out of the room and the X-ray machine clicks. It’s routine—mundane, even. But what if that X-ray could do more than just show cavities or bone loss? What if it could detect cancer?
It’s a compelling idea, and not just because of its drama. Cancer, particularly in the oral and maxillofacial regions, can be insidious—hiding in plain sight, sometimes masquerading as a harmless sore or a swollen lymph node. Dentists, perhaps more than most realize, are in a unique position to catch these early signs. And dental X-rays? They are the lens through which that hidden pathology may, sometimes, begin to reveal itself.
But here’s the thing: dental X-rays aren’t crystal balls. They’re not comprehensive diagnostic tools for cancer in the way that, say, MRIs or PET scans are. So can they detect cancer? Sometimes. Can they miss it? Absolutely. And that’s where this article becomes valuable—because it will help you understand exactly what dental X-rays can and can’t do when it comes to cancer detection.
We’re going to unpack the science, confront some widespread myths, and walk through what you, as a patient or even a healthcare provider, should actually be thinking about when the topic of dental X-rays and cancer comes up. Expect nuance. Expect straight answers. And expect to leave this article equipped with everything you need to never Google this question again.
Understanding Dental X-Rays: What They Are and How They Work
Let’s start at the beginning: what exactly is a dental X-ray, and what can it show?
Dental X-rays—also known as dental radiographs—are specialized images that allow dentists to see beneath the surface of your gums and enamel. Think of them as the “Google Maps” of your mouth. They don’t just show traffic (i.e., cavities), but the terrain beneath (roots, bone structures, impacted teeth, and sometimes more). But like any map, there are limitations depending on the kind of lens and scale used.
Types of Dental X-Rays and What They Reveal
There are several types of dental X-rays, and they each offer a different angle on your oral health:
- Bitewing X-rays: These are the ones taken most frequently. They capture the crowns of the upper and lower teeth in one area, useful for spotting cavities and assessing bone loss due to gum disease.
- Periapical X-rays: These go deeper—literally. They show the entire tooth, from crown to root, and the surrounding bone. If there’s something brewing down at the root level (like a cyst or an abscess), this is where it will show up.
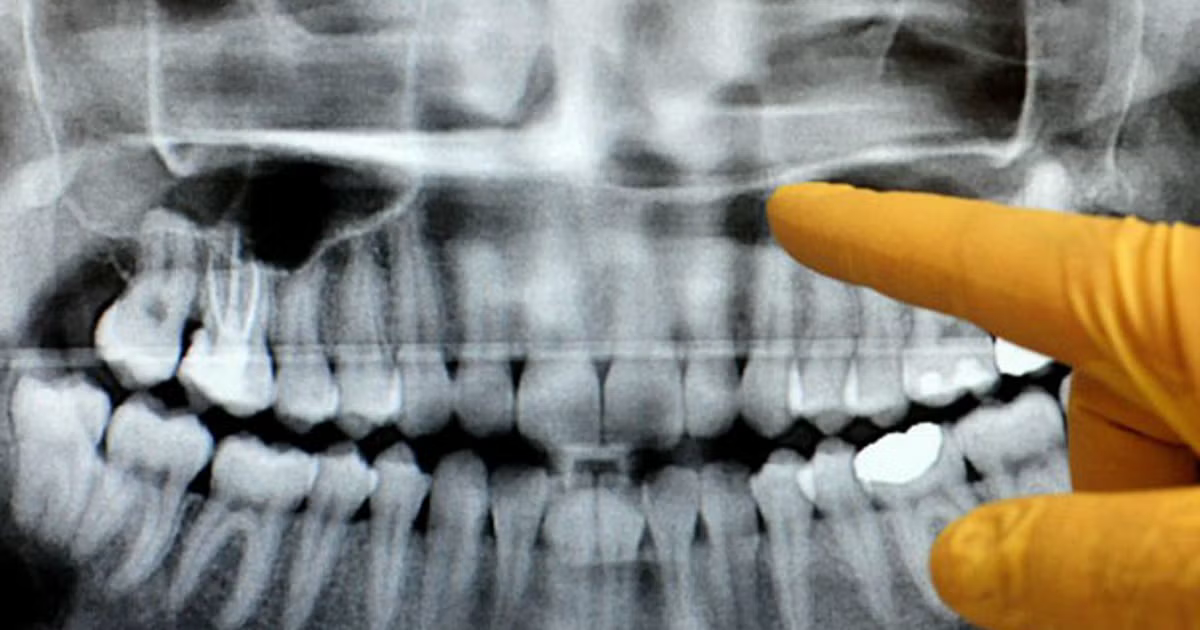
- Panoramic X-rays: These are broader and offer a sweeping view of the entire mouth: both jaws, the nasal area, sinuses, and the temporomandibular joints (TMJ). They can sometimes reveal larger issues—like tumors, jaw fractures, or impacted wisdom teeth—that don’t show up on bitewings.
- Cephalometric and cone-beam CT scans: These are more advanced and typically used in orthodontics or oral surgery, but they can also assist in evaluating jaw-related tumors and cysts.
Now, here’s where we get to the real point: can any of these X-rays show cancer?
Can an X-Ray Spot a Tumor?
The short answer is: potentially. The long answer is a bit more technical, but worth your time.
Dental X-rays are great at visualizing hard tissue—meaning bone and teeth. If a tumor affects the jawbone or causes bone erosion, it may appear on a dental X-ray as a darkened area, an irregular border, or a disruption in normal bone patterns. But what about soft tissue tumors, like those on the tongue, cheek, or floor of the mouth? Those areas often don’t show up clearly on standard X-rays, which are not designed to visualize soft tissues in high detail.
So if your dentist sees something suspicious on an X-ray—a bone that looks moth-eaten, or a shadow that shouldn’t be there—it’s not a diagnosis. It’s a flag. A signpost that says, “This needs a closer look.”
And that’s the key distinction: dental X-rays don’t diagnose cancer. They suggest possibilities that require follow-up.
A Peek Behind the Curtain: How They Work
Dental X-rays use controlled bursts of ionizing radiation to create images based on how different materials in your mouth absorb or block those rays. Dense structures like enamel and bone absorb more radiation and show up as white. Soft tissues, being less dense, allow more rays through and appear darker.
That contrast is what allows dentists to identify anomalies. A cavity? That shows up as a dark spot in the tooth. Bone loss? A gradient shift along the jaw. A suspicious mass? It depends—location, density, size, and the angle of the X-ray all influence what gets seen.
You might wonder: if the technology is based on density and absorption, can’t we just tweak the contrast and see everything? Unfortunately, no. Soft tissues and early-stage tumors don’t produce the kind of contrast you’d need for reliable detection with standard dental X-rays.
What About Radiation Exposure? Is It Worth It?
This is a common concern—and a valid one. Yes, X-rays use radiation, but the doses are extremely low. A routine dental X-ray exposes you to about 0.005 millisieverts (mSv), which is roughly the same as a few hours of natural background radiation from the environment.
To put it in perspective, flying from New York to L.A. exposes you to more radiation than a dental X-ray. That said, repeated exposure—especially without medical justification—is discouraged. That’s why dentists follow the ALARA principle: As Low As Reasonably Achievable.
| Type of X-Ray | Description | Primary Uses | Cancer Detection Potential |
|---|---|---|---|
| Bitewing | Small images showing upper and lower teeth crowns | Detect cavities, check bone loss | Limited (mostly crowns and nearby bone) |
| Periapical | Full tooth from crown to root plus surrounding bone | Detect root problems, abscesses, bone issues | Moderate (bone changes around roots visible) |
| Panoramic | Wide view of jaws, teeth, sinuses, TMJ | Impacted teeth, jaw fractures, tumors | Good for bone involvement and large lesions |
| Cone-Beam CT (CBCT) | 3D imaging of teeth, jaw, sinuses | Detailed bone structure, surgical planning | Excellent for bone tumors and complex anatomy |
| Cephalometric | Side view of skull and jaws | Orthodontics and growth assessment | Limited for cancer detection |
If there’s no clinical reason for an X-ray, a good dentist won’t take one. If there is? The potential to catch a progressing disease—possibly even cancer—far outweighs the tiny risk of radiation.
The Basics of Oral Cancer: What You’re Actually Hoping Dental X-Rays Might Catch
So we’ve established that dental X-rays are sometimes capable of revealing suspicious findings—especially when it comes to bone—but the real elephant in the room is this: what exactly is “oral cancer”? What are we even looking for?
If you’re picturing a large, unmistakable mass somewhere obvious—something so glaring it would leap off an X-ray image—you’re not wrong to assume that’s one possibility. But that’s also not how most oral cancers show up, especially in the early stages. They’re quieter. Subtler. And that’s precisely what makes them dangerous.
What Is Oral Cancer, Technically Speaking?
Oral cancer is a type of head and neck cancer that develops in the tissues of the mouth or throat. It most commonly affects the tongue, floor of the mouth, cheeks, lips, palate, and gums. The vast majority of these cancers—about 90%—are squamous cell carcinomas, meaning they originate from the flat, scale-like epithelial cells lining your mouth.
That means most oral cancers begin on the surface—on tissue that is routinely visible, even inspectable, during a thorough dental exam. Ironically, this makes them more “available” for early discovery than many other cancers—if you know what to look for.
So why do they still get missed?
Because they rarely start with fireworks. No obvious pain, no dramatic swelling. Sometimes it’s just a white patch. Or a red spot that doesn’t go away. Or a sore that lingers for weeks. Things that are easily mistaken for more benign problems like canker sores or irritation from dental appliances.
And that’s precisely the problem: early oral cancer mimics the mundane.
How Common Is Oral Cancer, Really?
You might not hear about oral cancer in everyday conversation, but it’s far from rare. According to recent estimates, roughly 54,000 new cases of oral or oropharyngeal cancer are diagnosed each year in the U.S. alone. Around 11,000 people die from it annually.
| Symptom/Sign | Description | Why It Matters | Is It Visible on X-Ray? |
|---|---|---|---|
| Persistent sore or ulcer | A sore that doesn’t heal after 2 weeks | May indicate early cancer or precancer | Usually no |
| White or red patches (leukoplakia/erythroplakia) | Discolored areas on mucous membranes | Potential precancerous lesions | No |
| Lump or thickening | Noticeable mass in cheek, tongue, or gums | Could be a tumor or infection | Sometimes (if bone involved) |
| Numbness or tingling | Loss of sensation in mouth or jaw area | Nerve involvement could suggest advanced lesion | No |
| Difficulty swallowing or speaking | Changes in function affecting eating or speech | May indicate spread or advanced disease | No |
| Unexplained bleeding | Bleeding without obvious cause | Can signal tumor vascularization | Rarely |
Let that sink in. These are not abstract numbers. Oral cancer kills roughly one person per hour in the United States. Not because we don’t have the tools to fight it, but because most cases are diagnosed late—after the cancer has already advanced.
This is where dental professionals come in.
Why Dentists Are Frontline Cancer Scouts (Even If They’re Not Oncologists)
Here’s something that might surprise you: many oral cancers are first flagged not by doctors, but by dentists or dental hygienists during routine exams. They have the best seat in the house, after all—literally in your mouth, under bright lights, several times a year.
Most comprehensive dental checkups include a visual and tactile cancer screening, even if your dentist doesn’t announce it that way. They’re feeling under your tongue, checking the sides of your mouth, pressing along your jaw and neck. They’re looking for asymmetry, ulcerations, unusual discolorations, or indurations (that means “firm spots,” for the curious).
But of course, what they can’t always see or feel is what might be happening beneath those tissues—or deep within the jaw. That’s where imaging steps in. And while dental X-rays aren’t the primary tool for cancer screening, they can add a layer of visibility that the naked eye simply can’t offer.
What Are the Main Risk Factors for Oral Cancer?
Let’s get clear on this, because it’s not just about luck.
- Tobacco use—in all forms—is the single biggest risk factor. Cigarettes, cigars, chewing tobacco, snuff… they all dramatically raise the odds.
- Heavy alcohol consumption is next in line, and when combined with tobacco? That’s a synergistic nightmare—the risk isn’t just additive, it’s multiplicative.
- HPV (Human Papillomavirus)—specifically HPV-16—is now responsible for a rapidly growing subset of oral and oropharyngeal cancers, particularly in younger, non-smoking individuals.
- Sun exposure plays a role too, particularly with lip cancers.
- Poor oral hygiene, chronic irritation (from broken teeth or ill-fitting dentures), poor nutrition, and a weakened immune system all contribute to risk, though their roles are more nuanced.
And then, yes, there’s the wildcard: genetics. Some people are simply more biologically susceptible.
So when your dentist spots something suspicious during an exam—or sees something odd on an X-ray—it’s not paranoia. It’s vigilance. And that vigilance can save lives.
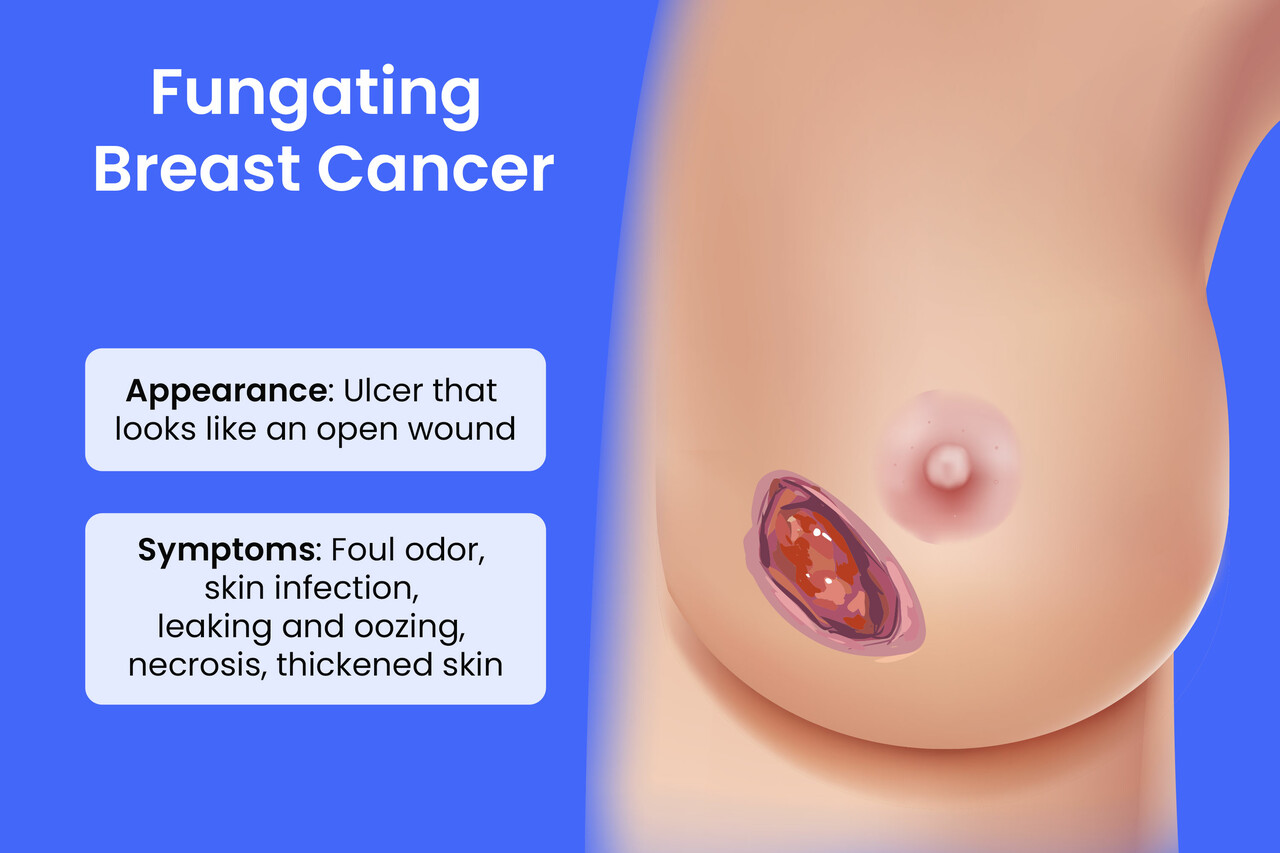
What Does Early Oral Cancer Look Like? (And Why It’s So Easy to Miss)
You’re smart enough to ask the follow-up: if we’re talking about surface-level cancers, shouldn’t they be easy to see?
Sometimes, yes. But early oral cancer doesn’t announce itself with fanfare. It can look like:
- A white patch (leukoplakia) or red patch (erythroplakia)
- A non-healing ulcer, especially one that bleeds easily
- A lump or thickening of the oral tissues
- Persistent hoarseness or a sore throat
- Difficulty chewing or swallowing
- Numbness, especially in the lower lip or chin
Here’s a particularly underappreciated red flag: a sore spot that doesn’t hurt. Why is that significant? Because we’re conditioned to associate danger with pain. But many early oral cancers are completely painless, which leads people to ignore them—sometimes fatally.
Coming up next: in Part 3, we’ll explore how dental X-rays intersect with oral cancer, including the kinds of cancer they might show, what “suspicious” findings look like, and where they fall short.
Can Dental X-Rays Detect Cancer? Here’s the Honest, Nuanced Answer
Let’s get right to it: can dental X-rays detect cancer? It’s a simple question, but like most things in medicine, the answer lives in the gray space between “yes” and “no.”
If you’re here for certainty, here’s what I can offer: dental X-rays can reveal clues—sometimes even strong ones—that suggest a malignancy. But they are rarely definitive. They don’t give you a diagnosis. They give you a reason to ask more questions.
And that’s actually powerful. Because the earlier you ask those questions—when a suspicious shadow or irregular border first shows up—the better your chances of catching something before it becomes a crisis.
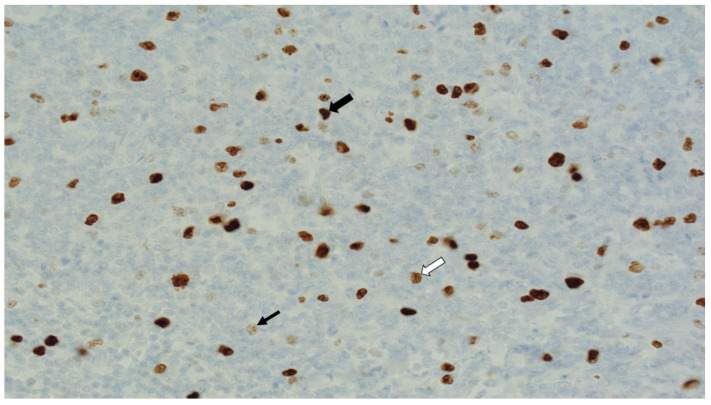
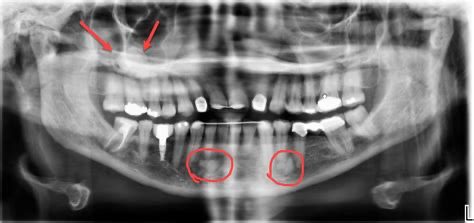
What Cancer Might Look Like on a Dental X-Ray
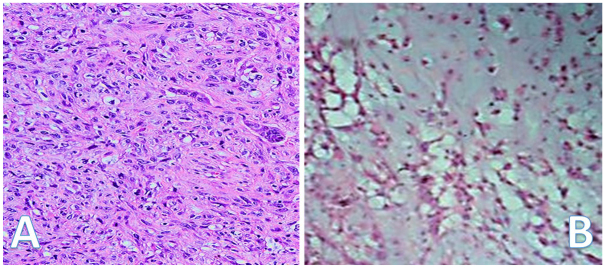
First, let’s set the stage: X-rays show contrast. Denser materials (like bone) appear light or white. Less dense materials (like soft tissue, air spaces, or fluid-filled cysts) appear darker. Dental X-rays excel at capturing the structural integrity of teeth and jawbone. They’re less helpful when it comes to soft tissue (we’ll tackle that later).
So what might a cancerous lesion look like on an X-ray?
- Irregular bone loss: Not the neat, horizontal resorption you see in gum disease, but patchy, asymmetric erosion—often described as “moth-eaten” or “ill-defined.”
- Radiolucent lesions: That means dark areas where you wouldn’t expect them. These can suggest anything from a cyst to a benign tumor to something more ominous like a malignancy.
- Loss of lamina dura: This is the thin, white line that outlines the tooth socket. If it’s missing or disrupted, that might be a red flag.
- Unusual widening of the periodontal ligament space: This can be a subtle but early sign of malignancy.
- Root resorption or displacement: When a tumor presses against or invades bone, it can alter the natural positions of roots and surrounding structures.
So yes—X-rays can absolutely pick up on abnormalities that raise concern for cancer, particularly when it involves bone invasion or deep-seated tumors in the jaws or sinuses.
But—and it’s a big but—X-rays cannot see what they are not designed to see.
What Dental X-Rays Can’t Show (And Why That Matters)
Here’s where reality steps in. Most oral cancers begin in soft tissues—the tongue, the inner cheeks, the floor of the mouth, the lips. These structures are not dense enough to show clearly on a traditional dental X-ray. You might get a faint outline or silhouette if a tumor is large enough, but subtle soft-tissue changes? Forget it.
This is why dentists use visual exams and palpation—running their fingers along your neck, your jawline, the sides of your tongue—not because X-rays are useless, but because they’re incomplete. They’re one piece of a larger diagnostic toolkit.
Another key limitation? Angle and coverage. A bitewing X-ray may give you excellent detail on the crowns of your molars but tell you nothing about your anterior palate or the base of your tongue. Even panoramic films, while broader in scope, can suffer from distortion or artifacts that obscure small but significant lesions.
So if your dentist tells you, “We need to take a closer look”—that’s not overkill. That’s precision. That’s how cancer is caught early.
The Case for Vigilance: When Dental X-Rays Have Caught Cancer
You might be wondering: Do we have real-world examples of dental X-rays leading to a cancer diagnosis? Absolutely.
Take the case of jawbone tumors, for instance—osteosarcomas, ameloblastomas, or metastatic lesions that have traveled from another primary cancer site (like breast or prostate). These are often first noticed on a routine X-ray when the dentist sees something that just doesn’t look right. Sometimes the finding is incidental: a patient comes in for wisdom teeth removal, and the panoramic X-ray reveals a mass in the mandible.
Or consider sinus involvement. A periapical or panoramic image might reveal opacification or bony destruction of the sinus floor—something a sinus infection wouldn’t typically cause. This can lead to further imaging, a referral to ENT, and ultimately, a diagnosis that might have otherwise been missed for months.
In these cases, the X-ray wasn’t the diagnostic endpoint—it was the starting line. The breadcrumb. The alert.
What Happens When Something Suspicious Shows Up?
This is the part that many patients don’t see—but it’s worth understanding. When a dentist sees a potential red flag on an X-ray, they don’t just hand you a diagnosis. Instead, they initiate a process:
- Repeat or alternative imaging: This might include a cone-beam CT (CBCT) scan for more detailed 3D imagery.
- Clinical correlation: They’ll match the radiographic finding with what they see and feel during your oral exam.
- Referral to a specialist: If suspicion remains, you’ll likely be referred to an oral surgeon, ENT, or oral pathologist for a biopsy or advanced imaging (CT, MRI, or PET).
- Biopsy and diagnosis: Ultimately, only a biopsy can confirm cancer. Everything up to that point is pattern recognition and educated inference.
This layered approach is intentional. It avoids over-treatment while ensuring that nothing dangerous gets overlooked.
So Should You Worry? Or Trust the Process?
That’s the million-dollar question, right?
Here’s the truth: you should be aware, but not anxious. Dental X-rays are not miracle detectors, but they’re incredibly useful tools in the right context. If your dentist recommends one, it’s likely because they’re looking out for more than just cavities. They’re checking your foundation—your bone health, your anatomy, and yes, signs that something might be wrong.
Curious how these stack up against more advanced imaging? PET scans for colon cancer offer a broader view but aren’t typically used in routine dental care.
And if they don’t find anything? That’s good news—but it doesn’t mean you’re invincible. That’s why regular clinical exams and open communication matter just as much.
When X-Rays Aren’t Enough: What Happens When We Need to Look Deeper
Let’s say your dentist sees something on an X-ray—something irregular, something… off. It’s not necessarily alarming, but it’s not routine either. What happens next?
Or maybe your symptoms are persistent—an odd tingling in your jaw, unexplained pain, a sore that’s lingered too long—but your X-rays come back clear. Is that the end of the road? Not even close.
This is where advanced imaging steps in. Because sometimes, X-rays can only whisper what needs to be shouted. And when there’s ambiguity—when something looks suspicious, but not conclusive—the next step is escalation. Not panic, not worst-case assumptions, but better tools and sharper resolution.
Why Standard Dental X-Rays Hit a Wall
We’ve talked about the strengths and limitations of dental X-rays, but it’s worth underscoring this: they’re fundamentally 2D snapshots of a 3D world. That means they suffer from overlap, distortion, and “hidden zones” where small pathologies can slip through undetected.
| Imaging Modality | What It Shows Best | Limitations | Typical Use Case in Cancer Detection |
|---|---|---|---|
| Standard Dental X-Rays | Teeth and bone structure | Poor soft tissue visualization | Initial screening, bone involvement suspicion |
| Cone-Beam CT (CBCT) | 3D detailed bone anatomy | Limited soft tissue contrast | Detailed bone lesion assessment, surgical planning |
| Medical CT Scan | Bone and soft tissue contrast | Radiation dose higher than dental X-rays | Tumor extent, lymph node involvement |
| MRI | Soft tissue contrast and nerve involvement | Longer scan time, costlier | Soft tissue tumors, nerve infiltration |
| PET Scan | Metabolic activity of tissues | Limited anatomical detail, expensive | Detecting metastasis and tumor activity |
| Fluorescence/Optical Imaging | Surface tissue abnormalities | Mostly experimental, limited availability | Early mucosal changes in specialized centers |
And then there’s the issue of soft tissue invisibility. If a tumor is growing on the base of your tongue, nestled against your tonsillar pillars, or pressing into the floor of your mouth? A bitewing X-ray will have no idea. That’s not a design flaw. It’s just the wrong tool for that particular job.
So when a dentist says, “Let’s get a cone-beam scan,” or refers you out for a CT or MRI, they’re not throwing darts in the dark. They’re asking for higher resolution, wider context, and—if necessary—a full anatomical landscape.
Let’s break down these options, one by one.
Cone-Beam Computed Tomography (CBCT): The 3D Revolution in Dental Imaging
CBCT has become a game-changer in dentistry. Think of it as the MRI of the dental world—except instead of soft tissues, it gives a 3D view of your teeth, bones, and sinus anatomy. If a conventional X-ray is a photograph, CBCT is a hologram.

Dentists use CBCT when they need more precise detail on:
- Jawbone tumors or cysts
- Impacted teeth and root structure
- Temporomandibular joint (TMJ) issues
- Sinus involvement
- Suspicious lesions that don’t resolve
For detecting malignancies of the jaw, CBCT can be crucial. It allows clinicians to assess the size, shape, and borders of a lesion—and determine whether bone is being eaten away, displaced, or invaded.
Here’s a practical example: a periapical X-ray might show a faint radiolucent area at the apex of a molar. Could it be an abscess? Possibly. But a CBCT could reveal cortical bone expansion and erosion—features far more suggestive of something neoplastic (tumor-like) than inflammatory.
And yet—CBCT isn’t the whole story.
CT Scans and MRI: Going Beyond the Jaw
Once a red flag is raised—especially if it involves soft tissue or has the potential to extend beyond the oral cavity—your dentist or specialist may refer you for more advanced medical imaging.
CT (Computed Tomography) Scans
These scans use X-rays and digital processing to create cross-sectional images of the body, including the head, neck, and upper chest. CT scans are especially valuable for:
- Evaluating how far a tumor has spread
- Detecting lymph node involvement
- Visualizing bone destruction in more complex cases
They’re faster and better at visualizing bone and dense structures, but they still provide more soft-tissue detail than standard dental X-rays.
MRI (Magnetic Resonance Imaging)
If the goal is to map a tumor’s interaction with muscles, nerves, glands, or the base of the skull, MRI becomes the gold standard. It’s non-ionizing, meaning there’s no radiation exposure, and it excels at capturing detailed images of soft tissues—something dental X-rays simply can’t touch.
An MRI might be ordered when a suspicious lesion:
- Appears to involve muscle or nerve tissue
- Causes unexplained numbness or motor deficits
- Is located near critical structures like the tongue base, pharynx, or salivary glands
In some cases, both CT and MRI are used together, offering a comprehensive picture of both the structural and soft-tissue context of the lesion.
PET Scans: The Cancer Tracker
Now we’re venturing into full-on oncologic territory. Positron Emission Tomography (PET) scans are not standard tools in dentistry. But if a malignancy has been diagnosed—or is strongly suspected—your care team might order a PET scan to assess metabolic activity.
In plain English? A PET scan shows how active a tissue is, metabolically. Cancer cells tend to be ravenous—they consume glucose at high rates. A PET scan tracks a radioactive glucose tracer, lighting up areas where cancer might be hiding, even when anatomical imaging looks ambiguous.
So if a lesion is borderline or a biopsy is inconclusive, a PET scan might tip the balance toward action.
What Does All This Mean for You?
If you’re reading this and thinking, “This seems like a lot of steps just to confirm something suspicious,” you’re absolutely right. And that’s because the stakes are high, but the cost of overtreatment is too.
You don’t want to go into surgery or radiation therapy without a clear understanding of what you’re dealing with. And you also don’t want to delay intervention for something that’s growing and spreading silently. That balance—precision without panic—is what modern diagnostic imaging strives for.
If you’re worried about cumulative exposure, you’re not alone. Many people also ask whether dental implants or crowns raise any risk over time.
And the truth is, the process usually works. It’s methodical. Intentional. Designed to protect you both from harm and from unnecessary fear.
The Dentist’s Role in Cancer Detection: More Than Just Teeth Cleaning
When you think of a dentist, what comes to mind? Probably teeth cleanings, cavity fillings, maybe braces or whitening treatments. Rarely do people think of their dentist as a potential cancer sentinel. But the truth is, dentists are often the unsung heroes in early oral cancer detection.
You might wonder: “Wait, how is my dentist qualified to spot cancer? Aren’t they just teeth doctors?” Great question. The answer reveals just how comprehensive dental training really is—and how crucial your routine dental visits can be for your overall health.
Why Dentists Are Uniquely Positioned to Catch Early Cancer
Dentists see your mouth more thoroughly and more frequently than most doctors. While a primary care physician might glance in your mouth briefly during a check-up, your dentist examines every nook and cranny at every visit.
That includes:
- Checking the soft tissues—the inside of your cheeks, the tongue, floor of the mouth, palate, gums—for any suspicious changes.
- Palpating (feeling) for lumps, thickened areas, or tenderness in your mouth, jaw, and neck.
- Evaluating your oral hygiene, looking for chronic irritants or lesions.
- Reviewing your medical history and risk factors, like tobacco or alcohol use.
This combination of visual, tactile, and historical data gives dentists a distinct advantage. They’re not just fighting cavities; they’re scanning for red flags that could indicate cancer.
But Are Dentists Actually Trained to Spot Cancer?
You might ask, “Is cancer screening part of dental school curriculum?” Absolutely.
Dental education covers oral pathology extensively. Dentists learn to identify the early signs of oral cancer and differentiate them from benign conditions. They’re trained to understand what lesions warrant immediate referral and which can be safely monitored.
Of course, no dentist works alone in these cases. If something suspicious is found, the next step is often a referral to an oral surgeon, ENT specialist, or oral pathologist for biopsy and definitive diagnosis.
What Happens During a Cancer Screening at the Dentist?
If you’re curious what this looks like practically, here’s the typical flow:
- Visual Exam: Your dentist inspects all soft tissues for any discolorations, patches, lumps, or sores. They look for asymmetry, texture changes, and anything out of the ordinary.
- Palpation: Using gloved fingers, they gently press and feel around your tongue, under your jaw, your neck, and throat for any lumps or swelling.
- History Review: They’ll ask about risk factors, symptoms like pain, numbness, difficulty swallowing, or unexplained weight loss.
- Documentation and Monitoring: If something suspicious is found but not immediately alarming, they might document it carefully and monitor it over time.
- Referral: If warranted, you’ll be referred promptly for further testing—biopsy, imaging, or specialist evaluation.
It’s a surprisingly thorough process for what many imagine as a quick “look in the mouth.”
Can You Ask Your Dentist to Screen for Cancer?
Definitely. It’s your mouth, your health, your right. If you’re concerned about cancer—especially if you have risk factors or notice something unusual—bring it up. Dentists appreciate proactive patients. They want to know about:
- Sores or patches that don’t heal within two weeks
- Persistent lumps or thickened areas
- Unexplained pain or numbness
- Changes in speech, chewing, or swallowing
The more open your communication, the better your dentist can tailor their exam to your specific concerns.
Does Every Dental Visit Include a Cancer Screening?
In an ideal world, yes. The American Dental Association recommends an oral cancer screening at every routine dental visit for adults. However, the thoroughness varies depending on the practice and provider. Some dentists may be more vigilant than others, and some patients might receive more frequent X-rays or adjunct imaging depending on their risk profile.
So if you’re unsure, ask your dentist: “Do you perform an oral cancer screening as part of my exam?” If they say no, consider seeking a provider who does.
The Takeaway: Your Dentist Is Your Partner in Health
Ultimately, your dentist is more than just a cavity fixer. They’re a critical partner in your health team, trained to detect early warning signs of oral cancer that might otherwise go unnoticed.
By showing up regularly, staying informed, and speaking up about changes in your mouth, you’re empowering your dentist to do the best possible job. It’s a collaboration—and that’s where the power lies.
The Risks of Dental X-Rays: Should You Be Worried About Radiation?
By now, we’ve talked a lot about what dental X-rays can reveal. But a thoughtful discussion on their role in cancer detection would be incomplete without addressing the quiet worry in the background—the “but what about the radiation?” reflex that lingers in the minds of many patients, even if they don’t bring it up directly.
It’s not an unreasonable concern. “Radiation” is one of those words that carries weight. We associate it with nuclear fallout, environmental toxins, airport scanners, and serious medical procedures like CT scans or cancer therapy. So the moment we hear that dental X-rays involve radiation—especially if we’re told we need them routinely—it’s natural to pause and wonder: is this safe? Could it be doing more harm than good?
Let’s unpack that, carefully and with full context.
What’s the Actual Dose?
A single bitewing dental X-ray exposes you to about 0.005 millisieverts (mSv) of radiation. That number won’t mean much on its own, but for perspective: simply living on Earth exposes you to about 3 mSv of background radiation every year—from the sun, the soil, the air, even bananas. If you’ve ever taken a cross-country flight, say from New York to Los Angeles, that one trip gives you six times more radiation than a dental X-ray.
So no, we’re not talking about a level of exposure that meaningfully alters your long-term risk profile. In fact, the radiation from a typical dental X-ray is among the lowest of all medical imaging modalities—far lower than a chest X-ray, and orders of magnitude lower than a CT scan.
But of course, radiation isn’t only about single doses. It’s about accumulation.
Cumulative Exposure: Does It Add Up?
The question of “how much is too much?” hinges on context. Repeated exposure to ionizing radiation, even in small amounts, can theoretically increase cancer risk over time. That’s not controversial. But here’s where the nuance matters: most people aren’t getting dozens of dental X-rays a year, and when X-rays are taken, it’s because there’s a clinical need.
That’s the principle behind ALARA: “As Low As Reasonably Achievable.” Dentists are trained to use radiation only when it provides diagnostic value that justifies the exposure. That means no routine imaging just for the sake of it, and certainly no X-rays without cause.
If you’re a generally healthy adult who sees your dentist once or twice a year and gets bitewing films every 12 to 24 months, the actual radiation burden is trivial. Even for people undergoing complex procedures or chronic condition monitoring, modern digital X-rays minimize unnecessary exposure through precise targeting, ultra-sensitive sensors, and lower radiation output.
What About Children? And Pregnant Women?
This is where concern sharpens, and rightly so. Children are more sensitive to radiation because their cells are still dividing rapidly. The developing body is, by definition, more vulnerable to environmental stressors.
But the dental community knows this. Pediatric protocols aren’t just scaled-down versions of adult care—they’re tailored. Smaller sensors, protective shields, and conservative imaging frequency are the norm. When a child does need imaging, it’s done with extra layers of caution baked into every step. And in almost every case, the benefit of catching an emerging problem early—whether it’s a deep cavity, a congenital anomaly, or something more serious—far outweighs the vanishingly small radiation risk.
Pregnancy, too, warrants special attention. While dental X-rays don’t directly target the abdomen, and the radiation doesn’t reach the fetus, most providers err on the side of caution. Elective imaging is typically postponed until after birth, particularly during the first trimester. However, if a dental infection or suspected tumor demands attention, imaging can still be performed safely using lead aprons and thyroid collars. The decision is always risk-balanced, and patients are always part of that conversation.
But Haven’t There Been Studies Linking Dental X-Rays to Cancer?
Yes—and they make the rounds every few years in headlines and health blogs. The most commonly cited studies have looked at correlations between frequent dental X-rays and rare conditions like meningiomas (a type of brain tumor) or thyroid cancer. But correlation isn’t causation, and these studies have several important limitations.
Many rely on self-reported exposure histories, which are notoriously unreliable. Others involve patients who were exposed to older, higher-radiation imaging systems—decades before today’s digital tech. And most importantly, these studies often don’t control for confounding factors like genetic predisposition or other sources of radiation.
What’s emerged from more recent, methodologically sound research is a consistent conclusion: when used appropriately, modern dental X-rays do not pose a meaningful cancer risk to the average patient. The theoretical risk is dwarfed by the very real diagnostic benefit.
So, Should You Ever Decline a Dental X-Ray?
You can. It’s your right to refuse any test or treatment. But the better question is whether the refusal protects your health—or compromises it.
A good dentist doesn’t order imaging carelessly. If they’re recommending an X-ray, it’s likely because they’ve found something suspicious or want to rule out a deeper issue that they can’t assess with the naked eye. If you’re hesitant, ask: What are we looking for? Is this urgent? Are there alternatives?
And for signs that might show up too late for imaging to help, Oral cancer progression gives a reality check on early detection vs. advanced symptom onset.
Most dentists will welcome that dialogue. And more often than not, you’ll find that the rationale for imaging is based on your own best interest—not habit, not billing, and certainly not indifference.
The Game Is Changing: Innovations in Dental Imaging
By now, you have a clear understanding of what dental X-rays can and can’t do in the context of cancer detection—and how they fit into the broader diagnostic landscape. But the field isn’t static. In fact, it’s evolving at a remarkable pace. Behind the scenes, dental imaging is undergoing a quiet revolution, one that’s redefining what dentists can see, how early they can act, and how confidently they can diagnose.
You might be wondering: Are all these new imaging technologies really necessary? Or are they just expensive upgrades—nice to have but not essential? It’s a fair question. The truth? While some advances may initially feel like high-tech overkill, many are delivering meaningful improvements that directly benefit patients like you.
Digital Radiography: A Smarter Standard
Gone are the days of waiting for film to develop in a darkroom. Today, most modern dental offices have shifted to digital radiography—and not just for convenience. This isn’t just about faster workflows; it’s about better care.
Digital sensors are far more sensitive than traditional film, which means your dentist can obtain high-quality images using significantly lower radiation doses. The images appear instantly on a screen and can be magnified, contrast-enhanced, or color-adjusted to help detect subtle abnormalities that film might miss.
In the context of cancer detection, this translates to a greater chance of spotting bone changes or unusual lesions earlier—potentially before they progress or become symptomatic. Digital tools don’t just see more; they help your dentist interpret more.
Cone-Beam CT (CBCT): Imaging in 3D
While traditional X-rays offer a flat, two-dimensional view, CBCT technology creates detailed 3D images of your teeth, jawbones, and surrounding anatomy. Think of it as going from a snapshot to a virtual model of your mouth.
This matters because real anatomy isn’t flat. Structures overlap, hide behind curves, and twist in three dimensions. CBCT helps your dentist navigate that complexity. It’s especially helpful in:
- Detecting early bone changes that may signal tumors
- Differentiating lesions from routine infections
- Planning surgeries or biopsies with precision
Imagine trying to find a small fracture by looking at a photocopy. Now imagine being able to pick up the actual object, rotate it, and examine it from every angle. That’s the diagnostic advantage CBCT brings.
AI in Dentistry: Smarter, Not Just Faster
One of the most promising—and often misunderstood—advancements is the emergence of artificial intelligence in dental diagnostics. You might ask, Can a computer really detect cancer better than my dentist? The answer is: not yet. But it’s getting better all the time—and it’s already helping.
AI isn’t replacing dentists; it’s assisting them. These systems are trained on thousands (sometimes millions) of annotated images. They learn to recognize patterns—tiny shadows, asymmetries, or density changes—that a busy human might miss. They act as a second set of eyes, catching things that might otherwise be overlooked.
Right now, AI is helping dentists:
- Flag small radiolucent or radiopaque anomalies
- Measure lesion size and monitor progression over time
- Compare findings across patient records for risk assessment and trend analysis
Think of it like using grammar check in a word processor. It won’t write your novel, but it might catch the typo that changes the meaning of a sentence. In a clinical setting, that could mean catching a cancer earlier.
Beyond Radiation: Fluorescence and Optical Imaging
Not all progress involves radiation. Researchers and clinicians are also turning to light-based technologies to assess tissue health in non-invasive ways.
- Fluorescence imaging uses specialized light to make abnormal tissue “glow” differently than healthy tissue. It’s fast, safe, and could become a routine screening tool.
- Optical Coherence Tomography (OCT) is like ultrasound, but with light. It can produce high-resolution cross-sectional images of soft tissues, potentially identifying precancerous or cancerous changes earlier than a traditional exam.
These technologies are still emerging, mostly seen in research settings or advanced clinics—but they hold real promise for the future of routine cancer screening in dentistry.
So, What Does This Mean for You?
This isn’t about gadgets for gadgetry’s sake. These innovations mean your dentist is better equipped to detect problems sooner, with less radiation, more precision, and greater confidence. That means:
- Fewer missed cancers
- Less invasive follow-ups, because you’re catching things earlier
- More tailored treatment planning
- And increasingly, personalized care based on your individual risk profile
And perhaps the best news? These technologies are rapidly becoming more affordable and more widely available. What’s high-tech today may soon be the new standard in every practice.
Frequently Asked Questions (FAQs)
1. Can dental X-rays detect all types of oral cancer?
Great question. The simple answer is no. Dental X-rays are excellent at showing hard tissues like teeth and bone, so they may detect cancers that involve the jawbone or cause bone changes. But many oral cancers start in soft tissues—the tongue, cheeks, or floor of the mouth—which don’t show up well on standard X-rays. So while X-rays can provide important clues, they’re just one piece of the puzzle.
2. How often should I have dental X-rays taken?
There’s no one-size-fits-all answer here. Frequency depends on your oral health, risk factors, and your dentist’s clinical judgment. For some, X-rays might be needed every year; for others, every two or three years is enough. The key is that X-rays are only taken when there’s a clear reason—routine monitoring, new symptoms, or risk factors. Always ask your dentist why they recommend imaging.
3. Are dental X-rays safe for children and pregnant women?
Generally, yes—with caveats. Modern dental X-rays use very low radiation doses. Dentists take special care with children, using shielding and only imaging when necessary. Pregnant women are usually advised to avoid elective X-rays, especially in the first trimester, but urgent imaging can be done safely with proper precautions. Always inform your dentist if you’re pregnant or suspect you might be.
4. What should I do if my dentist finds something unusual on an X-ray?
Don’t panic. An “unusual” finding isn’t an automatic cancer diagnosis—it’s a signal for further investigation. Your dentist will likely recommend additional imaging or refer you to a specialist for evaluation and possibly a biopsy. Follow their guidance promptly, ask questions, and keep communication open.
5. Do dental X-rays expose me to harmful levels of radiation?
The radiation dose from dental X-rays is extremely low—far less than you’d get from natural background radiation or a routine flight. When used judiciously and with protective measures, the benefits of detecting potential problems outweigh the minimal risk from radiation.
Final Thought
Dental X-rays won’t show every cancer, but they’re a crucial piece of the puzzle. They complement your dentist’s hands and eyes in protecting one of your most important assets: your oral health—and by extension, your overall wellbeing.
Thank you for diving deep into this topic. You’re now better equipped to approach your next dental visit with clarity, confidence, and the right questions.