Can Dental Crowns Cause Cancer? Risk Breakdown & Safe Materials
- Foreword
- 1. Introduction to Dental Crowns
- 2. Understanding Cancer Risks in Dentistry
- 3. Examining the Evidence: Do Dental Crowns Cause Cancer?
- 4. Material-Specific Risks
- 5. Importance of Proper Dental Practices
- 6. Emerging Research and Future Trends
- 7. Patient Testimonials and Case Studies
- 8. FAQs
- Closing Thoughts
Foreword
It usually starts with a quick dental visit—maybe a chipped molar, an old filling gone soft, or a sudden jolt of pain when biting down. Your dentist gives you the verdict: You need a crown. It sounds routine. And it is. Until, somewhere between the X-rays and the numbing gel, a quiet question sneaks into your mind:
Is this safe?
Could a dental crown actually cause cancer?
You’re not alone in wondering. In an age where we question what goes into our food, on our skin, and even in our cookware, it’s natural to scrutinize what’s being permanently installed in your body—especially something that sits inside your mouth, day in and day out, in direct contact with tissue, saliva, and your bloodstream.
The internet doesn’t help. One search leads to a maze of conflicting opinions, outdated claims, and well-intentioned but often misinformed advice. Some articles flatly dismiss any concern as paranoia; others invoke toxicity, heavy metals, and worst-case scenarios without context. Neither extreme is helpful.
That’s why this article exists.
What follows is not just an answer to a single question—it’s a comprehensive exploration of what dental crowns are made of, how they interact with the body, and what science (not speculation) actually tells us about risk. It’s a breakdown of materials, techniques, biology, and yes, the legitimate concerns patients raise when facing what should be a simple restorative procedure.
This isn’t fearmongering. And it isn’t blind reassurance either. It’s clarity—backed by evidence, experience, and a healthy respect for your right to make informed decisions about your health.
So if you’re looking for the final word on whether dental crowns can cause cancer—and what to do with that information—you’ve found the right place.
Let’s begin.
Introduction to Dental Crowns
Let’s start with the obvious question: what exactly is a dental crown—and why would anyone need one in the first place?
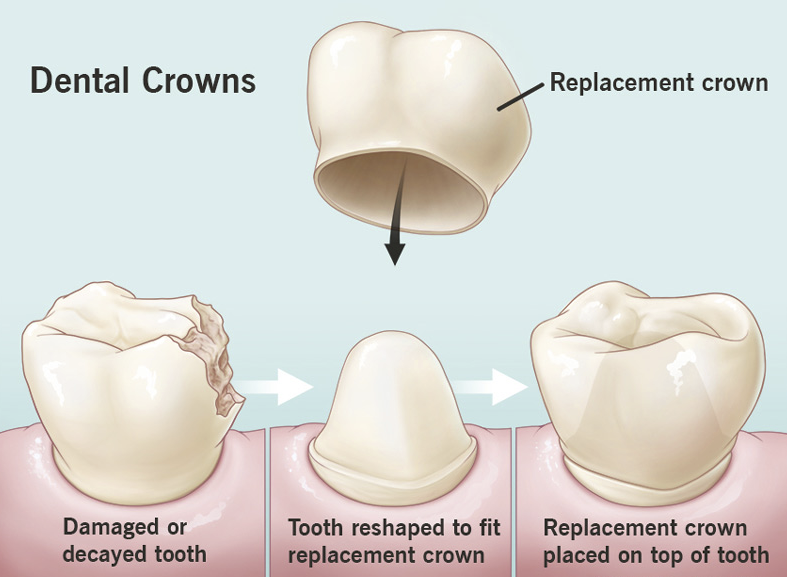
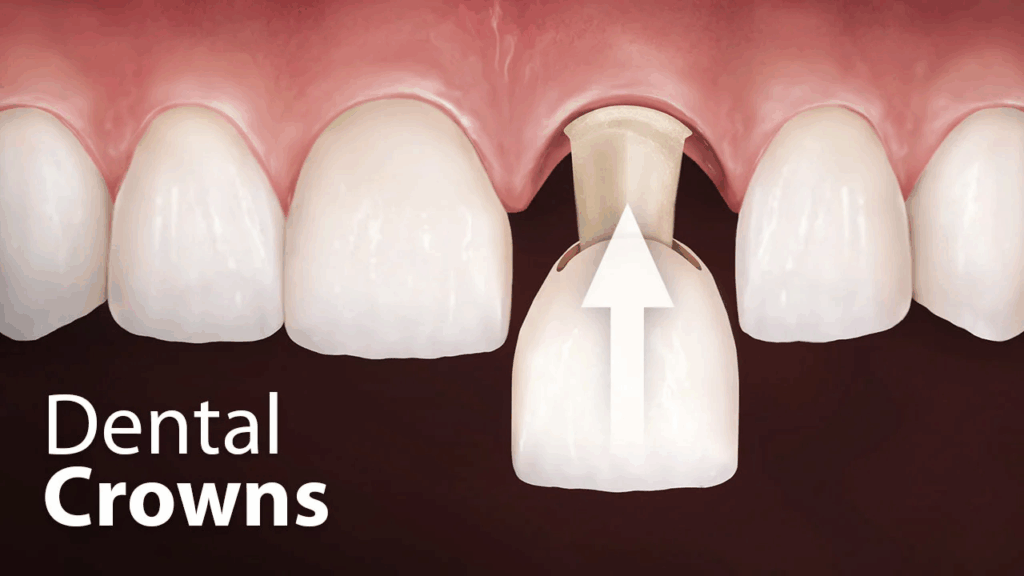
If you’re imagining something elaborate and gilded, you’re not entirely off-base. A dental crown is, quite literally, a protective cap—custom-made to fit snugly over a tooth that’s been damaged, weakened, or aesthetically compromised. It restores the tooth’s shape, size, and strength, and often, it improves the way it looks. You could think of it as a tailored suit for your tooth, engineered to protect and enhance what’s underneath.
Dental crowns are everywhere. By some estimates, millions are placed each year in the United States alone. They’re one of the most routine yet versatile tools in the dental arsenal. If you’ve had a root canal, a large filling, or a cracked tooth, chances are your dentist recommended a crown to keep things from unraveling.
Crowns are also used in cosmetic dentistry to reshape or align teeth, or even just to whiten a discolored one that bleaching can’t help. They’re not just functional—they’re also aesthetic.
But all this ubiquity has a hidden side. You might be wondering: If so many people are getting them, shouldn’t we be completely sure they’re safe?
That’s exactly the kind of question worth asking.
What Are Crowns Made Of—and Does It Matter?
Absolutely, it matters. And this is where the topic begins to unfold into something more nuanced. Dental crowns come in a variety of materials, each with its own strengths, limitations, and—crucially for this discussion—potential health implications.
Here’s a brief rundown:
- Metal Crowns: Often made of gold alloy, base-metal alloy (like nickel or chromium), or palladium. They’re incredibly durable and resistant to wear, but not exactly subtle in appearance.
- Porcelain-Fused-to-Metal (PFM): Combines the strength of metal with the natural look of porcelain. Still, the metal base can sometimes show through as a dark line near the gums.
- All-Ceramic or All-Porcelain: The go-to for front teeth due to their lifelike appearance. They’re metal-free, which appeals to many patients seeking biocompatible solutions.
- Zirconia: The new kid on the block. Extremely strong and also metal-free, zirconia crowns are becoming more popular for people concerned about sensitivity or allergic reactions.
Now, you may be thinking, Wait—did you say nickel? As in the metal that can cause allergic reactions? Isn’t that also something we’ve heard controversial things about in terms of health risks?
Yes. And it’s precisely those whispers—the possible toxic or carcinogenic properties of some materials—that we’ll be diving into in the sections ahead. For now, what’s important is this: not all crowns are created equal, and the composition of your dental restoration is a critical piece of the puzzle when evaluating long-term health outcomes.
People also ask whether titanium is safe, so if you’re comparing materials, the piece on titanium implants and cancer risk might round things out.
Should You Be Worried?
Let’s be honest: it’s easy to fall down the rabbit hole of online speculation. A headline here, a Reddit thread there, and suddenly you’re wondering whether your dental crown is leaching harmful substances into your bloodstream. While it’s wise to be cautious and informed, it’s also essential to distinguish genuine scientific concern from sensationalized fear.

The goal of this article is not to stoke anxiety—it’s to empower. To give you a comprehensive, evidence-based view of what dental crowns are, how they interact with your body, and what the science says about any potential link to cancer.
Because when it comes to something as intimate and long-lasting as a foreign material being placed inside your mouth, you deserve the full picture—not just the marketing brochure.
In the next section, we’ll zoom out and take a broader look at cancer risks in dentistry: where they come from, how they’re studied, and what’s actually known versus speculated. Spoiler alert: the answers aren’t black and white—but they are crucial to understanding the full story.
Let’s get into it.
Understanding Cancer Risks in Dentistry
Let’s shift gears for a moment.
Before we zoom in on dental crowns themselves, it’s worth asking: how does cancer even intersect with dentistry in the first place? That might sound like an odd pairing—teeth and tumors—but in fact, the relationship between dental interventions and cancer risk is more layered than many people realize.
What Is “Oral Cancer,” Anyway?
When people hear the phrase oral cancer, they often think of the tongue or maybe the inside of the cheek—but the term actually covers a broad range of malignancies. It includes cancers of the lips, tongue, floor of the mouth, hard and soft palate, sinuses, throat, and even the salivary glands.

It’s not rare either. According to the American Cancer Society, tens of thousands of people are diagnosed with oral and oropharyngeal cancers each year in the U.S. alone. And while traditional culprits like tobacco and heavy alcohol use account for a significant chunk of cases, there’s a growing body of evidence pointing to other contributors, like human papillomavirus (HPV) infections and chronic inflammation.
Which brings us back to dentistry.
Can Dental Work Contribute to Cancer Risk?
This is the crux of the question, isn’t it? Can something as seemingly mundane and routine as a dental crown plant the seeds for something as devastating as cancer?
Let’s start by acknowledging this: the mouth is a sensitive and biologically active environment. It’s not just a static space where teeth sit. It’s constantly exposed to mechanical forces, fluctuating pH levels, bacterial activity, and a steady stream of foreign substances—some intentional (like toothpaste), some less so (like micro-leakage from dental materials).
So yes, in theory, introducing foreign materials or appliances into the oral cavity could play a role in increasing cancer risk. But the devil, as always, is in the details.
What About Carcinogens in Dental Materials?
Now, let’s address the elephant in the room: certain materials used in dental work—particularly older ones or those used in budget procedures—have come under scrutiny for containing substances that are classified as potential carcinogens.
Take nickel, for instance. It’s found in many metal-based dental alloys and is a known allergen. But more to the point, the International Agency for Research on Cancer (IARC) has classified certain nickel compounds as Group 1 carcinogens, meaning there’s sufficient evidence they can cause cancer in humans—under certain conditions and in certain forms.
But does that mean your nickel-containing crown is a ticking time bomb?
Not so fast. The context matters. Just because a compound is classified as carcinogenic doesn’t mean every use of it is dangerous. In the case of dental alloys, the nickel is typically bound in a way that limits its bioavailability—it’s not just leaching freely into your tissues. Still, in individuals who are sensitive or allergic to nickel, chronic irritation or immune responses might, in theory, create conditions conducive to cellular changes over time.
So the concern isn’t entirely unfounded—but neither is it open-and-shut.
Is Chronic Irritation a Risk Factor?
This one gets surprisingly little airtime in most online discussions, but it’s worth shining a light on. Chronic irritation—say, from a poorly fitting crown that’s constantly rubbing against the inside of your cheek—can, over time, lead to cellular changes. There’s even a term for this phenomenon: traumatic ulceration. If it goes on long enough without healing, it may contribute to a microenvironment of persistent inflammation, and chronic inflammation is a known risk factor for cancer development.
So what’s the takeaway? Fit matters. Technique matters. It’s not just what material is in your mouth—it’s how it interacts with your tissues over time.
Fluoride, X-Rays, and Other Common Worries
While we’re here, let’s briefly touch on some other cancer-related concerns that often get bundled into discussions about dental care.
- Fluoride: This one’s perennially controversial. Fluoride in community water and dental products has been credited with drastically reducing tooth decay, but some groups have raised questions about its potential links to bone cancer. So far, large-scale studies have found no convincing evidence of such a link, and the consensus among major health authorities remains that fluoride is safe at recommended levels.
- Dental X-rays: Radiation exposure is a well-documented cancer risk—but the levels used in modern dental imaging are incredibly low. Still, best practices call for minimizing exposure when possible, especially in children and pregnant individuals.
- Mercury in fillings: Amalgam fillings contain mercury, which is a known neurotoxin. The cancer risk, however, appears negligible. Mercury in its elemental form (as used in fillings) behaves differently from methylmercury, the organic compound associated with toxicity in fish and industrial exposure.
So… Are Dentists Playing With Fire?
Not at all. Dentists are medical professionals held to high safety and ethical standards. But like any field, dentistry evolves. Materials improve. Protocols get updated. And patient concerns—particularly about long-term health effects—drive research and regulation.
The dental community isn’t hiding from these issues. In fact, the best practitioners welcome questions like yours. They know that informed patients aren’t paranoid—they’re proactive.
In the next section, we’ll finally drill into the heart of the matter (pun fully intended): what does the actual science say about dental crowns and cancer? Is there a proven link? Are certain materials more suspect than others? And what can you do—realistically—to protect yourself without spiraling into over-caution?
Let’s examine the evidence together.
Examining the Evidence: Do Dental Crowns Cause Cancer?
Now we’re at the core of the question—the one that’s likely been nagging you since you started reading: Is there actual evidence that dental crowns cause cancer? Not speculation, not anecdotes, not Internet panic—but real, hard science.
Let’s take this slowly and thoroughly, because this is where clarity really matters.
First Things First: What Does the Research Say?
Here’s the headline you won’t see on a fearmongering blog: there is currently no definitive evidence that dental crowns cause cancer. That’s not to say the idea came out of nowhere, but the available studies—including epidemiological surveys, toxicological analyses, and long-term safety data—have yet to establish a direct causal link between receiving a dental crown and developing any type of cancer.
And that’s not for lack of trying. The scientific community has looked into this—particularly when it comes to the materials used in crowns, such as nickel, chromium, beryllium, and, more recently, zirconia and ceramics. But no large-scale, peer-reviewed study has shown that crowns—by themselves—trigger malignant transformation in the surrounding tissues or in systemic organs.
But hold on—absence of evidence isn’t the same as evidence of absence, right?
Exactly. And this is where a nuanced discussion becomes essential.
Interpreting “Lack of Evidence” the Right Way
Just because something hasn’t been proven harmful doesn’t automatically make it safe for every person in every context. That’s why researchers and regulatory bodies evaluate risk—not just binary “yes or no” answers.
Think of it like this: we know that chewing tobacco can cause oral cancer. We also know that a dental crown might contain a trace of nickel, which is a possible carcinogen in certain forms. But that doesn’t mean the crown functions like a slow-release poison. The difference lies in exposure levels, biological availability, and how the material behaves once embedded in the body.
Most metals used in dentistry, including those in crowns, are alloyed in ways that reduce reactivity. They’re designed to be biocompatible—stable, inert, and unlikely to corrode or leach under normal oral conditions. That doesn’t mean they’re perfect. It just means they’re vetted.
Still, there are exceptions worth discussing.
So Why the Concern?
There are a few legitimate reasons the question about cancer risk persists—and deserves scrutiny.
One is bioaccumulation. Over time, materials that are not fully inert could theoretically degrade or corrode, especially in the moist, acidic environment of the mouth. This is particularly relevant in older metal-based crowns or in individuals with galvanic reactions (when dissimilar metals in the mouth cause small electric currents). While rare, these situations might contribute to chronic inflammation or allergic responses, which—if left unchecked—could potentially influence cellular behavior.
Another factor is genetic sensitivity. Some people may metabolize or respond to environmental exposures differently. A material that’s perfectly tolerated by 99% of the population could, in theory, trigger pathological processes in someone with a particular vulnerability—be it immunological, epigenetic, or otherwise.
And then there’s chronic irritation, which we touched on earlier. A crown that’s not properly contoured, polished, or seated can irritate surrounding gum tissue day after day, year after year. That persistent microtrauma isn’t just uncomfortable; it can, in theory, promote dysplastic changes—especially if compounded by poor oral hygiene or co-existing conditions like HPV infection.
But here’s the thing: none of this equates to proof of causation. At most, it points to theoretical risk under specific conditions, not a general indictment of crowns as carcinogenic devices.
What About Those Reports You See Online?
Let’s talk about that blog post you saw at 2 a.m. Or the viral TikTok video claiming someone’s dental crown “gave them cancer.” Anecdotes are powerful, but they’re not data. And while personal stories should never be dismissed out of hand—especially when people are genuinely suffering—they often lack the rigorous controls needed to determine what actually happened.
Did the crown cause the cancer? Or did it coincide with a malignancy that was already developing? Was the patient exposed to other risk factors—smoking, alcohol use, family history, viral infections? Without those controls, we’re in the territory of correlation, not causation.
This is why scientific conclusions are slow, methodical, and sometimes frustratingly noncommittal. But that’s a good thing. It means the bar for declaring something a health hazard is deliberately high.
The Role of Regulatory Oversight
It’s worth noting that dental materials don’t just get released into the wild without oversight. In the United States, the FDA classifies dental alloys and ceramics as medical devices and requires manufacturers to provide safety data, including potential toxicity. In the EU, the Medical Device Regulation (MDR) is even stricter.
That doesn’t mean risks are nonexistent—it means they’re being managed.
And yet, these systems rely on continuous post-market surveillance. That’s why if new data ever does emerge linking a material to elevated cancer risk, it will be taken seriously and acted upon. Science is self-correcting—but it needs time and data.
So Where Does This Leave Us?
You’re not wrong to be asking these questions. And you’re not paranoid for wanting answers that don’t sound like spin.
The evidence we have right now says that dental crowns are safe for the vast majority of people, especially when placed with care and crafted from high-quality, biocompatible materials. But like all medical interventions, they’re not entirely risk-free. The key lies in context—your medical history, your dentist’s technique, the materials used, and your ongoing oral health practices.
The next step is to dig deeper into these materials themselves. What’s actually in a crown, molecule by molecule? Which ones are more stable, more inert, or more prone to triggering unwanted biological responses? If you’re going to have something semi-permanent in your mouth, you deserve to know what it’s made of.
So let’s get specific. In the next section, we’ll break down the material-specific risks—because not all crowns carry the same profile, and choosing the right one can make all the difference.
For those with broader concerns about dentistry and cancer, root canals and their rumored links are also discussed in another evidence-focused explainer.
Material-Specific Risks
At this point, we’ve established that the question of whether dental crowns cause cancer isn’t as simple as “yes” or “no.” It depends on context—your biology, your dental history, and, crucially, the materials used in your crown.

Because let’s face it: a dental crown isn’t a magical object. It’s a manufactured product. And like any product you put into or onto your body—from skincare to surgical implants—what it’s made of matters. You wouldn’t shrug off the ingredients in a medication. The same caution applies here.
So let’s take the curtain down on what’s really inside these crowns and examine what we know—and what we still don’t.
Metal-Based Crowns: The Original Workhorse
Let’s start with the old-school choice: metal crowns. These have been in use for decades, and for good reason—they’re durable. In fact, for back molars that take the brunt of chewing forces, metal remains one of the most structurally reliable materials.
But—and this is a meaningful “but”—not all metals are created equal.
Some crowns are made of high-noble alloys, primarily composed of gold, platinum, or palladium. These tend to be well-tolerated and show low reactivity with human tissue. You rarely hear of someone reacting poorly to a gold crown—other than, perhaps, aesthetically.
Others, however, use base metal alloys, which often include nickel, chromium, cobalt, or beryllium. And this is where things get interesting.
Nickel, as we’ve already mentioned, is a known allergen and a suspected carcinogen in certain industrial forms. Chromium has its own risks, particularly in its hexavalent state (think of Erin Brockovich). And beryllium? Rare, but toxic in airborne particles. Again, these elements are typically bound in solid form within the crown, limiting their reactivity—but the concern lies in long-term exposure and individual sensitivity.
If you’ve ever had skin allergies to cheap earrings or belt buckles, you might want to think twice before opting for a nickel-containing crown.
And galvanic reactions—when dissimilar metals in the mouth create small electrical currents—can cause discomfort and potentially accelerate corrosion, which could increase the chance of metal ions being released into the surrounding tissue.
So yes, metal crowns are strong. But their safety profile isn’t one-size-fits-all.
Porcelain-Fused-to-Metal (PFM): A Compromise With Complications
PFMs were once considered the best of both worlds: the strength of metal underneath, the aesthetics of porcelain on top. And they do look more natural than plain metal, at least until the gum line recedes and that telltale gray rim shows up.
But structurally, they’re a sandwich—two materials fused together. And sometimes sandwiches fall apart.
Porcelain can fracture. The underlying metal can corrode, especially if the porcelain chips and exposes it. And let’s not forget: PFMs still contain metal—usually nickel or chromium—which means they carry similar long-term exposure risks as full-metal crowns.
What makes PFMs especially tricky is their uneven wear pattern. They can be rough on opposing teeth and don’t always age gracefully. For many, they’ve been replaced by more modern options.
All-Ceramic and Porcelain Crowns: A Cleaner Choice?
Enter all-ceramic crowns. Made entirely of tooth-colored materials like lithium disilicate or feldspathic porcelain, these crowns skip the metal altogether. That’s a major plus if you’re worried about potential reactivity or want to avoid even trace heavy metals in your mouth.
These crowns are also more biocompatible—meaning your body is less likely to react negatively to them. They integrate well with gum tissue and offer superior aesthetics, especially in the front of the mouth where appearance matters most.
So what’s the downside?
Fragility. Ceramic crowns are more likely to chip or fracture under high stress. They’ve gotten stronger over the years, thanks to advances in material science, but they’re still not ideal for every bite.
Also, while porcelain itself is considered biologically inert, the bonding agents used to cement it can contain resins or compounds like bisphenol-A (BPA), which has its own set of controversies when it comes to endocrine disruption and potential long-term toxicity.
This is not to suggest that your porcelain crown is leaching hormone disruptors into your bloodstream—but again, context and quality matter.
Zirconia Crowns: The Poster Child of “Biocompatible”
Let’s talk about zirconia—arguably the most buzzed-about crown material in modern dentistry.
Zirconia is a type of ceramic derived from zirconium, a transition metal that’s chemically altered to become extraordinarily tough and highly resistant to fracture. It doesn’t contain nickel, chromium, or mercury. It doesn’t corrode. It’s also naturally white, so it looks reasonably tooth-like without needing an outer layer of porcelain.
And it’s been labeled “biocompatible” by just about every regulatory body that matters.
But is it perfect? Not exactly.
While rare, some studies have suggested that zirconia may not bond as easily to tooth structure without special primers or cements. There have also been isolated reports of sensitivity or inflammation around poorly fitted zirconia crowns—although these seem to be the exception, not the rule.
Still, zirconia appears to strike the best balance between strength, safety, and aesthetics—making it a top choice for patients who want something both tough and biologically quiet.
So What Should You Choose?
Ultimately, choosing a crown material is not just about avoiding cancer. It’s about balancing safety, function, durability, and aesthetics—and making that decision in collaboration with a dentist who understands both the science and your personal needs.
If you have metal allergies, autoimmune conditions, or a history of chronic inflammation, you might opt for ceramic or zirconia. If you grind your teeth like a cement mixer and don’t mind a flash of silver in the back of your mouth, high-noble metal may still serve you best.
What matters is informed choice. Know what’s going in your body. Ask questions. Don’t accept a material just because it’s “standard.” Standards shift—and they should, as our understanding evolves.
Next, we’ll explore something even more essential: how proper technique and long-term care make a crown safe or unsafe—often more so than the material itself. Because even the best material, if poorly placed or left unmonitored, can become a problem waiting to happen. Let’s dig into how to protect your mouth for the long haul.
Importance of Proper Dental Practices
By now, it’s clear that not all dental crowns are equal. Material matters, yes. But there’s another dimension to this equation that often gets less attention—and yet it may be just as influential, if not more so, when it comes to long-term safety.
We’re talking about technique. Skill. Ongoing care. Because here’s a truth that applies far beyond dentistry: even the best materials, placed badly, can cause problems—and even average materials, applied with precision and monitored correctly, can last a lifetime without incident.
In other words, your dentist’s hand is just as important as the crown itself.
Fit Is Not Cosmetic—It’s Biological
Let’s start with something deceptively simple: the fit of the crown. When done properly, a crown should hug the tooth snugly, aligning perfectly at the margins where it meets the gumline. That junction—called the cervical margin—is a hot zone. If there’s a tiny gap, a ledge, or overhang, it becomes a magnet for plaque, food particles, and bacterial buildup. That sets the stage for gingival inflammation, periodontal disease, or even secondary decay.
Worse, a poorly fitted crown can create subtle but chronic mechanical irritation. Day after day, your cheek or tongue rubs against a rough edge or an ill-placed surface. You may not even notice it at first. But your body does. This kind of chronic low-grade trauma is one of the lesser-known risk factors for abnormal cell growth, and in the long term, it could—under the right circumstances—contribute to precancerous changes in the surrounding tissues.
Does that mean a rough margin will give you cancer? No. But does it mean you should accept “good enough” from your dentist? Also no.
Cementation: The Invisible Weak Link
The way a crown is cemented can be just as critical. If there’s a void in the cement layer, or if a poorly chosen adhesive breaks down over time, micro-leakage can occur. This allows bacteria to infiltrate the space between the crown and the natural tooth. The result? Not only decay, but potentially a slow, ongoing immune response in the surrounding gum tissue.
Certain cements have also been scrutinized for their chemical makeup. Some older or low-quality products may contain compounds that degrade into formaldehyde or other irritants, especially under acidic conditions like dry mouth or reflux. Again, this doesn’t spell doom—but it does illustrate how invisible details influence biological outcomes.
Your dentist should be using cements that are biocompatible, durable, and suited to the specific crown material. It’s not a one-size-fits-all decision.
Occlusion: A Silent Saboteur
Then there’s occlusion—how your teeth meet when you bite. A crown that’s too high, too flat, or not harmonized with the opposing tooth can wreak havoc over time. It might cause jaw pain or headaches. But it can also cause the crown to crack, the underlying tooth to fracture, or nearby teeth to shift—each of which introduces new areas of trauma and inflammation.
Poor occlusion can even accelerate wear on enamel or disrupt the natural flow of saliva. It seems minor, but over years, small misalignments create big problems.
Your dentist should be checking and adjusting your bite meticulously. Not just with carbon paper and a quick tap-tap, but with attention to how your jaw moves through a full chewing cycle. This is an art as much as a science.
Follow-Up: What Happens After Placement Is Just as Important
A crown isn’t a “set it and forget it” device. The mouth is a dynamic environment—acidity shifts, gums recede, habits evolve. What fit perfectly today might need adjusting in two years. That’s why regular dental checkups aren’t optional—they’re essential.
A dentist monitoring your crown should be checking for:
- Signs of marginal leakage
- Gingival inflammation near the crown
- Hairline cracks or material fatigue
- Changes in occlusion due to wear or shifting
- Early mucosal changes or lesions
These evaluations can catch small issues before they become serious. They’re your early warning system—and, in some cases, your cancer prevention strategy.
And Then There’s You
Let’s not pretend all the responsibility falls on the dentist. You play a central role here, too.
Brushing and flossing matter even more when you’ve got a crown. So does your diet. If you’re regularly bathing your teeth in sugar, acid, or processed junk, you’re not just feeding cavities—you’re stressing the biological interface between crown and tissue.
And if you smoke or vape? That adds another layer of complication. Both habits alter the oral microbiome, reduce blood flow, and impair immune response. If there’s any latent irritation from a crown, smoking acts like gasoline on a smoldering ember.
Be proactive. If something doesn’t feel right—if you notice swelling, persistent soreness, bleeding gums, or a burning sensation near a crown—say something. Earlier is always better.
The Human Factor
Let’s not forget: no two mouths are the same. Your immune system, your genetics, your saliva composition—they all play a role in how your body interacts with a foreign object like a crown.
This is why “biocompatibility” isn’t universal. Something that’s inert in one patient might provoke a subtle reaction in another. This doesn’t mean crowns are inherently dangerous—it means dentistry, like all of medicine, is moving toward individualized care. You deserve materials and practices that respect your body’s unique biology.
So while we’ve spent a lot of time talking about potential risks, here’s the reassuring part: with high-quality materials, proper technique, regular checkups, and good oral hygiene, the vast majority of dental crowns serve their purpose safely, beautifully, and for years—sometimes decades.
But vigilance matters. And as research into long-term effects continues to evolve, staying informed is part of how you stay safe.
Next, we’ll turn our attention forward: what’s happening in dental research now? What new materials, innovations, and safety measures are coming down the pipeline—and how might they change the crown conversation for the better? Let’s take a look at the future.
Emerging Research and Future Trends
So far, we’ve looked backward and inward—tracing the materials, methods, and mechanisms behind crowns and their potential risks. But what about the horizon? If you’re the kind of person who’s asking, “Could dental crowns cause cancer?” then you’re probably also wondering, “Are they getting safer? Smarter? More advanced?”
The short answer is: yes. And while dental crowns of the past were largely functional devices designed to “patch” a damaged tooth, today’s crowns—and those coming just around the bend—are becoming precision-engineered, biologically aware restorations that reflect a whole new philosophy of care.
Let’s explore where that’s going.
Biocompatibility Is No Longer a Bonus—It’s a Baseline
There’s a quiet revolution underway in dental materials science. Where we once focused primarily on structural durability, we’re now just as concerned with how materials interact with the body over time. This isn’t just about avoiding allergies or immune responses—it’s about understanding and minimizing inflammatory potential at the molecular level.
Zirconia, for instance, has opened the door to crowns that are both strong and exceptionally tissue-friendly. But researchers aren’t stopping there. Modified ceramics with antibacterial surfaces, fluoride-releasing capabilities, or even embedded nanoparticles designed to discourage plaque accumulation are all being explored. Think of it as a dental crown that not only fills the gap but actively promotes oral health.
We’re also seeing greater scrutiny of what goes into dental cements, bonding agents, and glazes—tiny ingredients that might only make up a fraction of the restoration but can have outsized biological effects, especially over time. The push is clear: materials that are bioinert, non-leaching, and predictable in long-term behavior.
The implications? Fewer inflammatory lesions. Lower risk of local irritation. Possibly even a reduced role in precancerous environments.
Digital Dentistry Is Changing Everything
When we talk about future trends, we can’t ignore the digital renaissance sweeping through dentistry. Crowns are no longer hand-crafted in the back room of a lab using wax molds and intuition. Today, high-resolution intraoral scanners, CAD/CAM milling, and 3D printing are becoming the norm.
Why does that matter for your health?
Because precision matters. A better-fitting crown isn’t just more comfortable—it’s less likely to trap bacteria, irritate soft tissue, or cause misalignment in your bite. All of which reduces the inflammatory burden in your mouth—and by extension, your systemic risk.
Moreover, digital records allow for perfect reproducibility. If something does go wrong or needs adjusting, there’s no guesswork. Your exact crown file can be reviewed, tweaked, and remade with sub-millimeter precision. That’s an entirely different landscape from the analog days, where small inconsistencies were accepted as part of the process.
Better precision means fewer mistakes. And fewer mistakes mean lower risk of the kinds of chronic irritation that could, over time, lead to pathology.
Smart Materials Are on the Horizon
Here’s where things start to feel like science fiction.
Researchers are now exploring responsive dental materials—crowns that can sense changes in the oral environment and respond in real time. Imagine a crown that slowly releases anti-inflammatory compounds if the surrounding gum tissue becomes irritated, or one that detects pH drops (a precursor to decay) and delivers a microdose of buffering agents to restore balance.
There are early prototypes of dental materials embedded with biosensors—tiny devices capable of monitoring temperature, pressure, and even biomarkers of inflammation or infection. In the long run, these could alert both patients and dentists to problems before symptoms arise, transforming crowns from passive hardware into active healthcare devices.
We’re not there yet—but we’re closer than you think.
Greater Personalization Through Genomics
Here’s something you don’t hear much about in mainstream dental conversations: genetic compatibility. But it’s coming.
As our understanding of genomics grows, so does our ability to predict how individuals will respond to specific materials. Some people may be predisposed to inflammatory responses from a certain alloy, while others might metabolize resin-based bonding agents differently. Personalized dentistry—matching materials not just to the mouth, but to the person—is becoming a realistic goal.
Eventually, you may not just be picking a crown based on appearance or cost—you could be choosing one based on your immune profile, your microbiome, even your epigenetic risk factors for conditions like oral cancer.
It’s a radical idea. But if you’re serious about long-term safety, it’s also a profoundly logical one.
Safer Doesn’t Mean Risk-Free
None of these advancements eliminate all risks, of course. Dentistry—like any field involving the human body—is subject to complexity. A perfect material in the wrong environment can still cause problems. And not every promising innovation makes it through clinical trials, let alone into routine practice.
But what’s changing is the framework. We’re moving away from a purely mechanical mindset toward a biological and systemic one. Crowns are no longer just about covering a tooth—they’re about integrating into a living system without disrupting it. That’s a seismic shift.
So, if you’re wondering whether to worry about your crown, or to worry about getting one in the future, here’s some perspective: you have more control than ever. Better materials, better technology, better techniques, and better science are all converging to make crowns not just safer, but smarter.
In the next section, we’ll ground all this theory in something deeply human: lived experience. Because while studies and trends matter, what we often remember—and respond to—are real stories. What does this all look like in practice? What have patients experienced, and what can we learn from their outcomes?
Let’s turn toward the clinical lens and see how this all plays out in real lives.
Patient Testimonials and Case Studies
We’ve covered science, materials, biological responses, and even glimpses of the future. But for many people, understanding risk isn’t about data points or chemical formulas—it’s about stories. It’s about what happened to someone else like them. Because, let’s be honest, clinical language can sometimes flatten what is, in reality, a very personal experience.
When you sit in the dental chair and hear, “We’ll need to put a crown on that,” your brain doesn’t start running epidemiological risk assessments. It starts asking: Will this hurt? Will this last? Will I be okay?
And that’s why patient stories matter.
The Case of the Hypersensitive Engineer
Let’s start with Marcus—a 43-year-old mechanical engineer with an impeccable health record and a mouth full of old amalgams from his twenties. When his dentist recommended replacing a cracked molar with a porcelain-fused-to-metal crown, Marcus didn’t blink. The procedure went smoothly, and within a few weeks, the crown had settled in—except for a persistent tingling on the inside of his cheek.
He chalked it up to healing. But months later, the tingling hadn’t gone away. It turned into a burning sensation, especially after eating spicy foods. His dentist was puzzled. The crown looked perfect. The margins were sealed. The bite was balanced. But Marcus knew something felt off.
Eventually, after a second opinion, patch testing revealed a nickel sensitivity. The metal under his porcelain crown—harmless to most—was provoking a localized immune response in his tissues. It wasn’t cancer. It wasn’t dangerous. But it was chronic inflammation. The crown was replaced with a zirconia alternative, and within two weeks, the burning disappeared.
What does Marcus’ story tell us? Not that crowns are dangerous, but that even well-placed restorations can cause problems in the wrong biological context. And sometimes, “normal” isn’t universal.
A Hygienist’s Perspective on Long-Term Safety
Then there’s Annette, a 57-year-old dental hygienist who has spent her entire career watching people cycle through restorative work—some gracefully, some not. She’s seen decades-old gold crowns that still function flawlessly, and ceramic crowns that fractured within five. Her own mouth? A combination of high-noble metal in the back, zirconia in the front.
What Annette emphasizes isn’t fear—it’s maintenance.
She points to cases where crowns were blamed for problems that actually stemmed from poor hygiene, missed check-ups, or just wear-and-tear left unaddressed. When she sees inflamed tissue or deep pockets around a crown, it’s rarely about the material—it’s about neglect.
From her perspective, the bigger threat to oral health isn’t a rogue molecule from a crown—it’s apathy.
Annette’s lived experience reminds us: a crown is a prosthetic. It needs care, attention, and monitoring, just like any implanted device in the body. Crowns themselves aren’t inherently toxic. But they’re not invincible either.
When Pathology and Prosthetics Intersect
Now let’s look at a more complicated case—Linda, a 61-year-old retired teacher who was diagnosed with oral squamous cell carcinoma three years after receiving a series of crown placements.
It would be tempting to connect the dots: dental work, then cancer. But Linda’s history included two decades of smoking, untreated GERD, and a chronic white patch on the lateral tongue that she’d ignored for years. The crowns? Well placed, no inflammation, no defects.
Her oncology team found no link between the dental work and the tumor. In fact, the crowns themselves weren’t even in the cancerous zone. But Linda’s story underscores something important: when oral pathology does develop, everything in the mouth gets scrutinized—and often unfairly implicated.
Her case doesn’t exonerate crowns or condemn them. It just highlights the complex, multi-factorial nature of oral disease. Cancer rarely has a single cause. It’s a cascade—and dental work is usually a footnote, not the trigger.
The Outliers: When Things Truly Go Wrong
Of course, there are the outliers. Cases where biocompatibility tests were ignored. Where inferior materials were imported from questionable suppliers. Where dentists cut corners or failed to monitor long-term outcomes.
Yes, these exist. A few have made headlines, and a few more are quietly recorded in medical literature. But they represent exception, not rule. That distinction matters.
Because if you’re trying to assess your own risk, you don’t need to dwell on sensational stories—you need context, clarity, and critical thinking.
So What Do These Stories Add?
Why dwell on anecdotes in an article grounded in science? Because risk is personal. And so is reassurance.
Patient experiences tell us where things go right and where they don’t—not just in terms of materials or technique, but in terms of follow-through. They show that success is often found in the details: choosing the right crown, asking the right questions, staying engaged with your care.
They also remind us that dental crowns don’t exist in isolation. They’re part of a much bigger system—your immune response, your oral microbiome, your systemic health habits. And they perform best when viewed that way: not as a one-off repair, but as a piece of a larger health ecosystem.
In the next section, we’ll bring everything full circle with a practical, patient-centered FAQ—addressing the most common concerns that inevitably arise after reading everything we’ve covered. And from there, we’ll close with some final thoughts on what all this means for you, your health, and your future decisions.
FAQs
1. Can dental crowns cause cancer?
Let’s address the elephant in the room with everything we now know: there’s no direct, proven causal link between dental crowns and cancer. That bears repeating.
No study has shown that having a crown—of any material—statistically increases your risk of developing oral or systemic cancer. What we have seen are theoretical risks based on material composition (nickel, chromium, etc.), and rare cases of chronic irritation that could, in theory, contribute to an inflammatory microenvironment. But in those cases, the crown is at most one ingredient in a far more complex recipe.
If there’s a takeaway here, it’s that materials matter, placement matters, biology matters—but crowns themselves are not inherently carcinogenic.
2. Are certain materials in crowns more risky than others?
Yes—and no. If you’re allergic or sensitive to metals like nickel or beryllium, then a metal-based crown poses more risk for you than for someone else. But for the general population, these materials are considered safe within the context of dental alloys, especially when properly processed and bonded.
Where concern creeps in is with poor-quality manufacturing, older crown designs, or situations where materials are combined in a way that encourages corrosion or tissue reactivity. In contrast, modern all-ceramic or zirconia crowns tend to show excellent biocompatibility profiles with minimal adverse responses.
That said, even the most inert material can become problematic in the wrong mouth or under the wrong conditions. That’s why personalized consultation and testing matter.
3. How can I minimize any potential risks associated with dental crowns?
This one’s more actionable—and more empowering.
First: choose your provider wisely. A meticulous, evidence-based dentist who uses high-quality labs and customizes materials based on your needs is your first line of defense.
Second: advocate for biocompatible materials. Ask what’s being used. Ask why. If you have known sensitivities, get tested. Don’t settle for a generic solution just because it’s cheaper or faster.
Third: follow up. Get regular checkups. Maintain excellent oral hygiene. Monitor for gum inflammation, changes in tissue texture, or any persistent discomfort around crowned teeth. These aren’t red flags, but yellow lights—subtle cues that it’s time to recheck the map.
And don’t forget systemic health. A crown isn’t an island; it’s part of your broader immune and inflammatory landscape.
4. Should I be concerned about existing crowns?
If your existing crowns are comfortable, stable, and showing no signs of tissue irritation, then the answer is probably no. The body is surprisingly good at signaling distress—especially in the mouth.
But if you’ve experienced odd symptoms—burning, discoloration, persistent soreness, or gum recession—it’s worth getting a second look. That doesn’t mean panic. It means inquiry. And a careful exam from a well-trained dentist can usually spot any structural or biological issues before they become bigger problems.
5. Are there safer alternatives to traditional crowns?
There are always trade-offs. All-ceramic and zirconia crowns represent the current high standard for biocompatibility and aesthetics, with minimal systemic reactivity. For front teeth especially, they’re often the best choice. But they may be more prone to fracture than metal-based options under heavy bite force.
If you’re particularly concerned about systemic exposure to metals or reactive compounds, zirconia is likely your best bet. But material alone isn’t enough. A crown is only as safe as its design, placement, and maintenance.
There’s no universally “safest” crown—only the crown that’s safest for you.
Closing Thoughts
If you’ve read this far, you’re not just curious—you’re intentional. You’re asking smart, uncomfortable questions not out of fear, but out of a desire to make informed choices. And when it comes to something as personal as a dental crown, that mindset matters.
So here’s where the science stands: there is no clear evidence that dental crowns cause cancer. But that doesn’t mean there are no risks. Materials vary, placement matters, and individual biology plays a role. In rare cases, chronic inflammation or poorly managed restorations can contribute to problems—but not because crowns are inherently dangerous. Because the process was flawed.
The good news? Much of this is within your control. Choosing the right material, working with a skilled dentist, asking the right questions, and staying alert to how your body responds—all of it stacks the odds in your favor.
The mouth isn’t isolated from the rest of you. It’s a window into—and a driver of—systemic health. So asking how safe your crown is isn’t trivial. It’s wise.
Now you’re equipped not just with facts, but with perspective. Use it. Ask better questions. Demand better care.
And above all, trust your ability to navigate it. You’re not just getting a crown.
You’re taking ownership of your health.













