Can a FibroScan Detect Liver Cancer? A Comprehensive Medical Overview
- What Does a FibroScan Measure, and How Does It Work?
- Can FibroScan Indirectly Signal the Presence of Liver Cancer?
- When Is FibroScan Most Useful in Liver Cancer Evaluation?
- Symptoms of Liver Cancer That FibroScan Cannot Reveal
- Comparing FibroScan to Other Diagnostic Tools in Liver Oncology
- FibroScan vs. Other Liver Cancer Diagnostics
- How Underlying Conditions Affect FibroScan Accuracy
- FibroScan in the Setting of Liver Cancer Surveillance Programs
- Can FibroScan Help Stage Liver Cancer?
- The Role of FibroScan in Guiding Liver Cancer Treatment Decisions
- How Bone Metastases Influence Liver Cancer Workup
- Limitations of FibroScan in Diagnosing Early Liver Cancer
- FibroScan in Patients with Concurrent Liver and Pancreatic Concerns
- Potential Risks, Misinterpretations, and False Alarms with FibroScan
- The Future Role of FibroScan in Cancer Detection and Management
- When to Use FibroScan, and When Not To
- FAQ

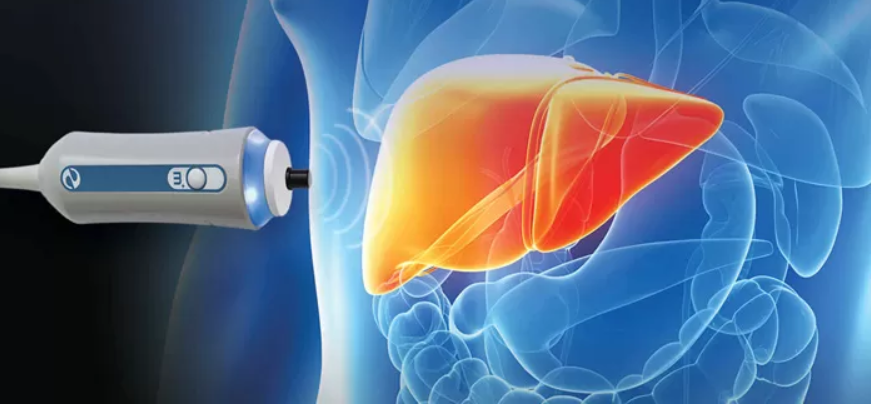
What Does a FibroScan Measure, and How Does It Work?
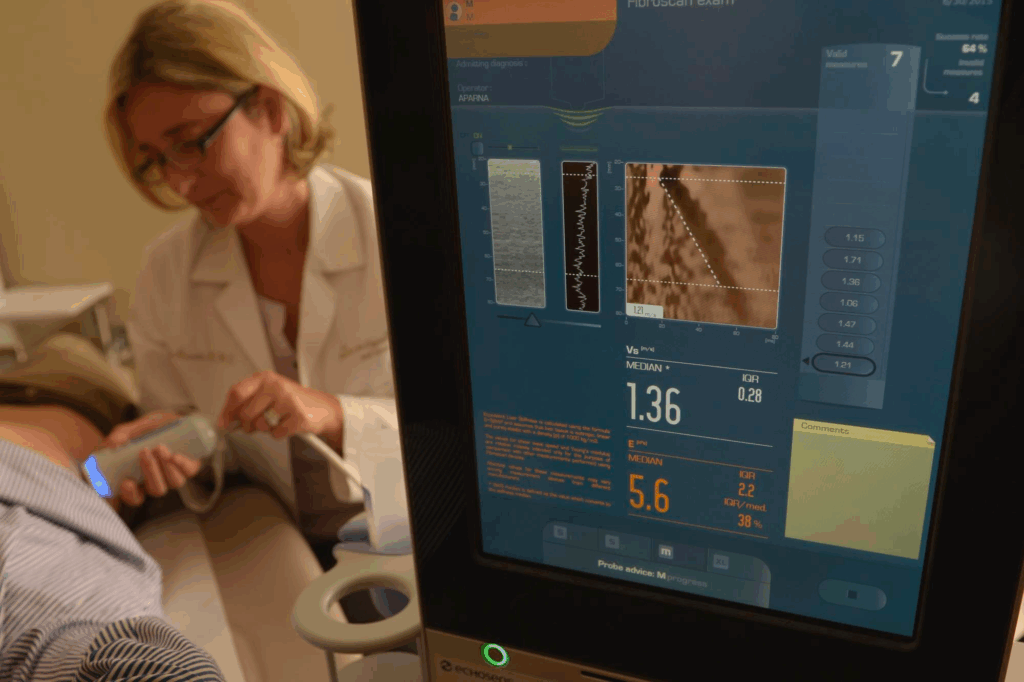
FibroScan measures liver stiffness by emitting a painless pulse of energy into the liver and calculating the speed of wave propagation through the tissue. Stiffer liver tissue, often a result of fibrosis or cirrhosis, conducts the wave faster. The results are reported in kilopascals (kPa) and correlate with fibrosis stages from F0 (no fibrosis) to F4 (cirrhosis).
Unlike ultrasound or MRI, FibroScan doesn’t produce an image or detect masses. It is a functional test, offering insight into the mechanical properties of the liver parenchyma. For this reason, it excels at quantifying diffuse liver damage but cannot directly identify nodules, tumors, or vascular abnormalities.
However, liver stiffness is closely linked to cancer risk. Chronic fibrosis and cirrhosis are the most significant risk factors for hepatocellular carcinoma. In that sense, FibroScan plays an indirect but essential role in liver cancer surveillance—by identifying patients at high risk who need further imaging and monitoring.
Can FibroScan Indirectly Signal the Presence of Liver Cancer?
While FibroScan cannot detect liver tumors per se, extreme or rapidly increasing stiffness values—especially in patients with previously stable scores—may signal a need for deeper evaluation. A sudden rise in stiffness could reflect inflammation, congestion, or tumor infiltration, even though the device cannot distinguish the cause.
In patients with chronic hepatitis B or C, alcoholic liver disease, or nonalcoholic steatohepatitis (NASH), the transition from fibrosis to cirrhosis significantly raises liver cancer risk. FibroScan results above 12–14 kPa in such patients typically warrant enrollment in a surveillance protocol, which includes imaging and alpha-fetoprotein (AFP) testing.
Some studies have noted that extremely elevated stiffness values (above 75 kPa) in cirrhotic patients may correlate with the presence of a liver mass. However, these findings are not specific to malignancy and can also be seen with acute hepatic inflammation, thrombosis, or cholestasis.
To confirm cancer, clinicians must rely on imaging studies and tissue sampling. Lab markers like AFP and inflammatory indicators such as C-reactive protein may support the overall clinical picture. This is discussed further in the article c reactive protein and cancer.
When Is FibroScan Most Useful in Liver Cancer Evaluation?
FibroScan is most useful at the surveillance and stratification stages. It helps clinicians identify patients with significant fibrosis or cirrhosis who are at increased risk for developing liver cancer. In particular, it allows for noninvasive monitoring of fibrosis progression in chronic liver disease, which is the backbone of HCC risk prediction.
For example, in a patient with hepatitis C who has not yet progressed to cirrhosis, a FibroScan result of 8–9 kPa may justify lifestyle interventions and antiviral therapy, but not immediate cancer screening. In contrast, a patient with a value over 14 kPa is often considered cirrhotic and enters a high-risk category requiring routine imaging every six months.
This preemptive use of FibroScan allows doctors to initiate regular ultrasound and AFP testing before cancer becomes clinically apparent. While it doesn’t replace CT, MRI, or biopsy, it supports smarter use of these tools by selecting the right patients at the right time.
Symptoms of Liver Cancer That FibroScan Cannot Reveal
One of the most important limitations of FibroScan is that it does not assess clinical symptoms. Liver cancer may present with fatigue, abdominal fullness, early satiety, unexplained weight loss, jaundice, or right upper quadrant pain. None of these are measurable by FibroScan, nor are they necessarily correlated with liver stiffness.
In some cases, tumors may develop in patients whose liver stiffness is low or stable—particularly in noncirrhotic forms of liver cancer. These are often missed if physicians rely solely on FibroScan results without considering systemic signs or physical changes.
Additionally, symptoms like portal vein thrombosis or vascular invasion may not significantly change stiffness values, even though they are hallmarks of advanced HCC. A comprehensive approach, combining labs, imaging, physical examination, and patient history, is essential to avoid underdiagnosis.
Comparing FibroScan to Other Diagnostic Tools in Liver Oncology
FibroScan is just one component in the broader diagnostic arsenal for liver cancer. Its noninvasive nature and reproducibility make it valuable for screening and fibrosis monitoring, but its inability to image lesions limits its standalone use in oncology.
Other tools like abdominal ultrasound are often used first to visualize the liver, detecting masses as small as 1 cm. Contrast-enhanced MRI and multiphasic CT scans provide superior anatomical detail, revealing tumor size, vascular involvement, and intrahepatic spread. Positron Emission Tomography (PET) may also help identify distant metastasis or treatment response.
Biopsy remains the gold standard for confirming malignancy but carries bleeding risks, especially in cirrhotic livers. Tumor markers like AFP, des-gamma-carboxy prothrombin (DCP), and even newer molecular markers are used adjunctively.
The key is integration: using FibroScan to determine who’s at risk, ultrasound to scan for tumors, and CT/MRI for staging. This tiered approach improves efficiency and reduces overtesting in low-risk populations.
FibroScan vs. Other Liver Cancer Diagnostics
| Tool/Modality | Detects Cancer Directly | Measures Fibrosis | Assesses Vascular Involvement | Suitable for Screening | Requires Contrast |
| FibroScan (Elastography) | ❌ | ✅ | ❌ | ✅ (risk stratification) | ❌ |
| Ultrasound (US) | ✅ (limited) | ❌ | ❌ | ✅ (cost-effective) | ❌ |
| CT Scan (Triphasic) | ✅ | ❌ | ✅ | ⚠️ (radiation exposure) | ✅ |
| MRI with Gadolinium | ✅ | ❌ | ✅ | ⚠️ (cost, time) | ✅ |
| Liver Biopsy | ✅ | ✅ | ⚠️ (histologic only) | ❌ | ❌ |
| AFP Blood Test | ⚠️ (non-specific) | ❌ | ❌ | ✅ (adjunct use) | ❌ |
This table underscores the complementary—not competing—nature of diagnostic tools in liver oncology. FibroScan may open the door, but confirmation and staging require more targeted investigations.
How Underlying Conditions Affect FibroScan Accuracy
FibroScan results can be influenced by factors unrelated to cancer or fibrosis. For example, acute hepatitis causes inflammation that increases liver stiffness transiently. Cholestasis, liver congestion (as in right heart failure), and hepatic steatosis may also elevate stiffness measurements.
Similarly, ascites or obesity can interfere with proper probe placement, reducing accuracy. XL probes are available for obese patients, but technical failure still occurs in about 5–10% of cases.
In clinical practice, this means abnormal FibroScan results must always be interpreted in context. A single high value does not mean cancer—and a low value does not guarantee safety. Instead, it prompts a broader evaluation.
In complex cases—like a patient with cryptogenic cirrhosis and unclear imaging—a strategic colonoscopy might even be considered to rule out metastatic spread or synchronous cancers. As discussed in can a colonoscopy detect pancreatic cancer, thorough diagnostics often cross organ boundaries.
FibroScan in the Setting of Liver Cancer Surveillance Programs
For patients with known cirrhosis, FibroScan is often integrated into long-term surveillance protocols. The American Association for the Study of Liver Diseases (AASLD) and European guidelines recommend biannual ultrasound with or without AFP in high-risk groups.
FibroScan helps determine who belongs in these groups. It’s especially useful in chronic hepatitis B patients with minimal symptoms, where imaging may be deferred without fibrosis confirmation. Once FibroScan indicates advanced fibrosis or cirrhosis, these patients are enrolled into rigorous surveillance programs.
It also plays a role in de-escalating care. A patient whose stiffness drops significantly after antiviral therapy or weight loss (e.g., in NASH) may be re-stratified to a lower-risk category, reducing imaging burden.
Thus, FibroScan serves both to escalate and de-escalate follow-up, depending on its trend over time. It’s not just a one-time measure but part of a longitudinal care model.
Can FibroScan Help Stage Liver Cancer?
Staging liver cancer requires detailed anatomical and vascular imaging—typically via MRI or CT—not stiffness measurements. However, FibroScan contributes indirectly by assessing underlying liver function and reserve.
Stiffness values help estimate the severity of fibrosis or cirrhosis, which is critical in staging models like the Barcelona Clinic Liver Cancer (BCLC) system. Patients with well-preserved liver architecture (lower kPa) can tolerate more aggressive therapies, including surgery or ablation.
In contrast, patients with very high stiffness (especially >25–30 kPa) may have decompensated cirrhosis, which limits treatment options and alters prognosis. In such cases, systemic therapies or palliative care may be prioritized.
So while FibroScan does not classify tumor stage, it plays a foundational role in determining treatment eligibility—a key staging element in practical oncology.
The Role of FibroScan in Guiding Liver Cancer Treatment Decisions
Treatment of liver cancer depends not only on tumor characteristics but also on liver reserve. This is where FibroScan becomes a valuable planning tool.
For instance, surgical resection is possible only when liver stiffness is within a range that suggests the remaining liver will function adequately. Similarly, patients with early-stage HCC may qualify for curative treatments like radiofrequency ablation (RFA) or transarterial chemoembolization (TACE), provided they have sufficient liver reserve.
In liver transplant candidates, FibroScan supports assessment of baseline cirrhosis severity. Post-transplant, it may also be used to monitor for fibrosis recurrence or graft dysfunction.
Thus, while FibroScan doesn’t decide the treatment, it ensures the patient can safely undergo the chosen therapy. Without this insight, oncologic planning would carry significant risk.
How Bone Metastases Influence Liver Cancer Workup
In advanced stages, liver cancer—particularly hepatocellular carcinoma—can metastasize to bones, lungs, or lymph nodes. When bone pain or abnormal skeletal imaging occurs in a known liver cancer patient, metastatic spread must be considered.
Although FibroScan does not assess bones, elevated stiffness values coupled with systemic symptoms may suggest disease progression. A sudden increase in stiffness and worsening liver function can signal more aggressive tumor behavior.
Interestingly, some cancers that originate outside the liver—such as breast or prostate—can metastasize to the liver. In such scenarios, clinicians often explore parallel diagnostics. As outlined in can a bone density test detect cancer, bone scans and DEXA tools can sometimes hint at underlying malignancy even before symptoms appear.
Cross-organ insight is essential. Patients with known malignancy and liver findings should be evaluated in multidisciplinary teams to distinguish primary HCC from metastasis and guide appropriate treatment.
Limitations of FibroScan in Diagnosing Early Liver Cancer
The main limitation of FibroScan in cancer detection is its insensitivity to small or early-stage tumors. A patient could have a small hepatocellular carcinoma developing in segment VI of the liver while maintaining a stiffness reading under 12 kPa.
Such patients may fall through the cracks if surveillance is based solely on FibroScan results without imaging. This is particularly true in non-cirrhotic liver cancer, where the background liver is not fibrotic, and stiffness readings are normal.
FibroScan also cannot differentiate between benign and malignant causes of increased stiffness. Active hepatitis, steatohepatitis, or cholestasis may elevate readings without malignancy.
Therefore, relying solely on FibroScan without ultrasound, AFP, or MRI leads to underdiagnosis. This reinforces the importance of comprehensive protocols, especially in high-risk individuals or those with new symptoms.
FibroScan in Patients with Concurrent Liver and Pancreatic Concerns
In clinical practice, it is not uncommon for patients to present with overlapping abdominal symptoms involving both the liver and pancreas. For example, elevated liver enzymes, fatigue, or vague right upper quadrant discomfort could stem from either organ—or both.
While FibroScan excels at assessing liver stiffness, it cannot evaluate the pancreas. If symptoms persist despite stable FibroScan readings, or if patients have risk factors like chronic pancreatitis or genetic predisposition, additional evaluation is essential.
A colonoscopy may be ordered to rule out lower GI causes or as part of age-related screening. Occasionally, as noted in the article can a colonoscopy detect pancreatic cancer, this procedure may reveal indirect signs of external compression or GI inflammation that prompt pancreatic imaging.
Thus, FibroScan should never be used in isolation when broader abdominal pathology is suspected. It’s a powerful liver-specific tool, but its strength lies in supporting—not replacing—comprehensive diagnostic thinking.
Potential Risks, Misinterpretations, and False Alarms with FibroScan
Although FibroScan is a noninvasive and generally safe procedure, it is not without diagnostic risks. The most common issue is misinterpretation: assuming high stiffness always means advanced liver cancer, or that normal stiffness guarantees health.
False positives can arise due to acute hepatic inflammation, obstructive cholestasis, or even heart failure. These conditions stiffen the liver temporarily but do not indicate malignancy. Without clinical context, these readings may lead to unnecessary alarm and testing.
Conversely, false negatives may occur in early HCC without significant fibrosis, especially in non-cirrhotic livers. These tumors may grow silently, undetected by stiffness measurements.
Additionally, FibroScan results can be technically unreliable in patients with ascites, morbid obesity, or anatomical variation. Repeat scans and corroborating data are often needed for clarity.
The Future Role of FibroScan in Cancer Detection and Management
FibroScan is rapidly evolving. New developments aim to integrate it with 3D imaging or combine elastography with AI-powered liver maps. This may improve its diagnostic accuracy—not just for fibrosis, but potentially for distinguishing tumor-related stiffness.
Research is underway to assess whether stiffness patterns differ between fibrotic tissue and tumor-infiltrated liver. If validated, this could make FibroScan a more direct tool in cancer detection, particularly in regions with limited access to advanced imaging.
There’s also growing interest in using FibroScan in post-treatment surveillance. After chemotherapy, radiofrequency ablation, or transplant, changes in liver stiffness could reflect recovery, recurrence, or complication.
While it may never replace biopsy or MRI, FibroScan is poised to become more than just a fibrosis tool—potentially bridging the gap between screening and full-on imaging.
When to Use FibroScan, and When Not To
FibroScan is most valuable in chronic liver disease management, fibrosis staging, and cancer surveillance decision-making. It should be used routinely in:
- Chronic hepatitis B or C patients
- NASH or alcoholic liver disease
- Liver transplant follow-up
- Cirrhotic patients undergoing HCC surveillance
It should not be used as a cancer diagnostic tool in isolation, especially in symptomatic patients or those with normal stiffness but concerning labs or imaging.
Multidisciplinary care remains key. FibroScan tells one part of the story—the mechanical health of the liver. Imaging tells another. Bloodwork, biopsy, symptoms, and clinical context complete the picture.
FAQ
Can FibroScan detect liver cancer directly?
No, FibroScan cannot directly detect liver cancer. It measures liver stiffness, which may suggest underlying fibrosis or cirrhosis—known risk factors for hepatocellular carcinoma—but it cannot visualize or confirm tumors.
What liver stiffness values raise concern for cancer?
Very high stiffness values (typically >25–30 kPa) may raise concern, especially if rising rapidly. However, these values are not specific to cancer and must be confirmed with imaging and lab tests.
Can a normal FibroScan result rule out liver cancer?
Not always. Liver cancer can occur in non-cirrhotic livers, especially in early stages. A normal stiffness reading does not guarantee the absence of malignancy, particularly in patients with risk factors or symptoms.
How often should FibroScan be repeated in high-risk patients?
Patients with chronic liver disease or cirrhosis often undergo FibroScan every 6–12 months to monitor progression. Frequency may vary depending on etiology and clinical course.
What’s the difference between FibroScan and ultrasound for liver cancer?
FibroScan evaluates liver stiffness; ultrasound provides real-time images and can detect masses. They are complementary—FibroScan helps identify risk, ultrasound helps detect visible tumors.
Is FibroScan painful or risky?
No, FibroScan is completely noninvasive and painless. It’s comparable to an abdominal ultrasound and carries no risk of bleeding, radiation, or sedation.
How accurate is FibroScan in obese patients?
In obese patients, accuracy may decrease. Special XL probes improve readings, but in some cases, technical failure still occurs, requiring alternative evaluation.
Can FibroScan guide treatment decisions for liver cancer?
Yes. While it doesn’t show tumors, it informs clinicians about liver reserve. This is crucial for determining whether surgery, transplant, or local therapies are safe options.
Does FibroScan have any role after liver cancer treatment?
It can help monitor the liver post-treatment, especially for recurrence of fibrosis or cirrhosis. Its role in tracking post-ablation or transplant outcomes is under active research.
Can FibroScan results be elevated without cancer?
Yes. Acute hepatitis, bile duct obstruction, or even right-sided heart failure can falsely elevate stiffness values. Interpretation must always consider clinical context.
What other tests are needed to confirm liver cancer?
MRI, triphasic CT, biopsy, and tumor markers like AFP are standard for diagnosing and staging liver cancer. FibroScan helps decide who needs these tests.
Are there cancers that metastasize to the liver but don’t increase stiffness?
Yes. Some small or noninfiltrative metastases may not significantly affect liver stiffness. These require dedicated imaging for detection.
Can liver cancer metastasize to bone, and would FibroScan help?
Yes, advanced liver cancer can spread to bones. However, FibroScan does not assess skeletal metastases. Imaging and bone scans are needed in such cases.
How does FibroScan compare with colonoscopy in cancer diagnostics?
They serve different purposes. FibroScan assesses liver health, while colonoscopy visualizes the colon. For evaluating non-specific GI symptoms, both may be used. As described in the article can a colonoscopy detect pancreatic cancer.
What’s the future of FibroScan in cancer care?
Research is ongoing to expand its role through AI, integration with imaging, and monitoring post-treatment outcomes. While not a direct cancer detector, it may become more predictive in oncology settings.









