Can a DEXA Scan Show Cancer? Discover the Truth Behind DEXA Scans
- What Is a DEXA Scan and How Does It Work?
- Can a DEXA Scan Directly Detect Cancer?
- Situations Where DEXA Scans Raise Suspicion of Cancer
- How DEXA Scans Differ from Other Imaging in Cancer Detection
- The Role of DEXA in Monitoring Bone Metastasis
- When a DEXA Scan Might Miss Bone-Related Cancer Indicators
- Complementary Imaging Tools for Confirming Suspected Cancer
- Clinical Scenarios Where DEXA Aids in Cancer Management
- How DEXA Differs from Other Bone Imaging Modalities
- DEXA Scan as a Preventive Tool in Cancer Survivorship
- Cases Where DEXA Results Prompt Additional Cancer Work-Up
- Comparison of DEXA and Other Imaging Modalities in Cancer Context
- DEXA Scanning in the Management of Myeloma and Lytic Lesions
- Limitations of DEXA in Detecting Cancer Directly
- Clinical Guidelines and Recommendations for Use of DEXA in Oncology
- Future Developments in Bone Imaging and AI Integration
- FAQ
What Is a DEXA Scan and How Does It Work?
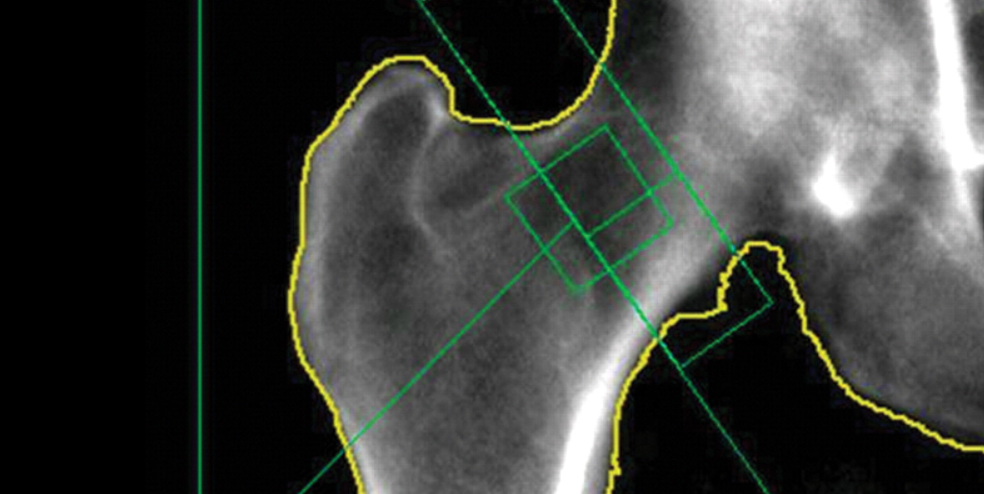
A DEXA scan, or dual-energy X-ray absorptiometry, is primarily a diagnostic tool used to assess bone mineral density. It functions by emitting two low-dose X-ray beams at different energy levels to measure the amount of calcium and other minerals in bones. Commonly used to diagnose osteoporosis, the test focuses on areas prone to fracture, including the lumbar spine, hip, and sometimes the forearm.
Unlike CT or MRI scans, DEXA offers no detailed anatomical images but provides highly accurate numerical data on bone density. It is non-invasive, quick, and exposes the patient to minimal radiation. Clinicians rely on the results to evaluate fracture risk, monitor treatment progress for bone-related conditions, and occasionally flag abnormalities that warrant deeper investigation.
Can a DEXA Scan Directly Detect Cancer?
Direct detection of cancer is beyond the capabilities of a DEXA scan. It cannot visualize soft tissue masses, detect tumors, or identify malignancies in organs. However, the test can reveal indirect signs of concern in the skeletal system. For example, if bone density drops rapidly or asymmetrically, it might suggest underlying pathology.
In the case of cancers known to metastasize to the bone—such as breast, prostate, and lung cancers—such changes might indicate the need for further imaging. DEXA cannot distinguish whether the cause is metastatic disease or osteoporosis, but it often serves as a trigger for advanced tests like bone scintigraphy, MRI, or PET scans.
In fact, when evaluating patients with unfavorable intermediate risk prostate cancer, oncologists may use DEXA as a supplementary assessment tool to monitor skeletal stability during androgen deprivation therapy.
Situations Where DEXA Scans Raise Suspicion of Cancer
While not definitive, there are scenarios where a DEXA scan can raise suspicion of bone malignancy or metastasis. One red flag is a significant localized density loss in a patient without known osteoporosis risk factors. If this occurs in areas not typically affected by age-related bone loss—such as the humerus or ribs—it may prompt concern.
Moreover, in cancer survivors undergoing long-term treatment, DEXA may show patterns of bone weakening that align with treatment-induced skeletal changes. These findings, especially if abrupt or asymmetric, could indicate possible metastatic involvement or secondary bone tumors.
How DEXA Scans Differ from Other Imaging in Cancer Detection
The role of DEXA in cancer imaging is distinct from modalities like MRI, CT, or PET scans. While DEXA quantifies bone density, other techniques provide anatomical and metabolic information that can pinpoint tumors, assess their size, and evaluate spread. Here’s a comparison:
| Feature | DEXA Scan | CT/MRI | PET Scan |
| Primary Use | Bone density measurement | Structural imaging | Functional/metabolic imaging |
| Can detect cancer directly? | No | Yes (anatomical tumors) | Yes (metabolic activity) |
| Detects soft tissue tumors? | No | Yes | Yes |
| Measures treatment effects? | Limited (on bone only) | Yes | Yes |
| Radiation exposure | Low | Moderate to high | High |
| Time required | ~10 minutes | 15–60 minutes | 30–60 minutes |
As this table shows, DEXA’s strength lies in identifying structural bone changes rather than malignancy. But its ease of use and low cost make it valuable in routine monitoring, especially in post-treatment cancer care or when other imaging is inconclusive.
The Role of DEXA in Monitoring Bone Metastasis
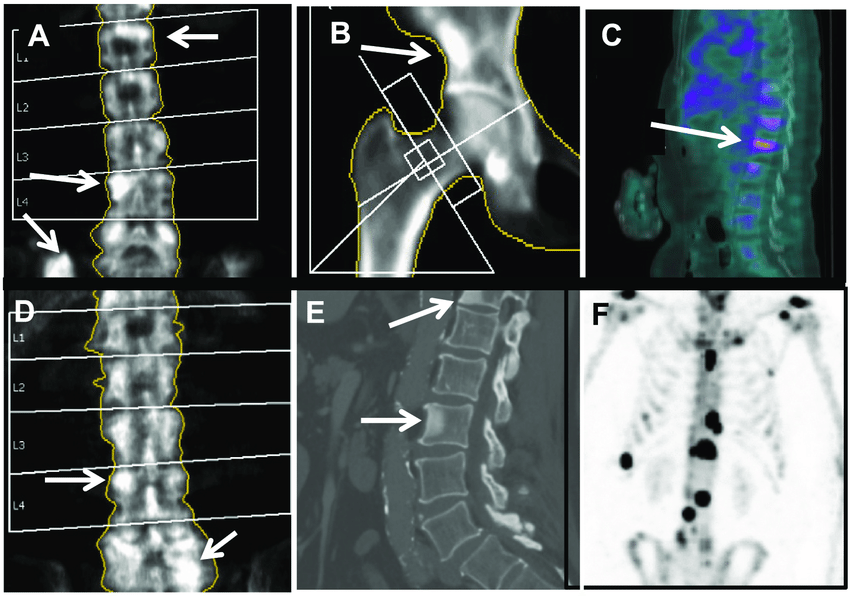
Although DEXA scans are not suitable for identifying primary cancer tumors, they are often utilized as a supplementary tool in patients with known cancer diagnoses—especially those with a high risk of bone metastasis. For cancers such as breast, lung, prostate, and multiple myeloma, metastases to the skeleton are common and may result in altered bone mineral density.
Oncologists may order regular DEXA scans to monitor changes in bone strength and density over time. A progressive decline in localized regions may suggest the development or progression of metastasis, particularly in conjunction with symptoms such as bone pain or elevated calcium levels. When subtle changes are detected, additional imaging like MRI or bone scintigraphy is typically recommended to confirm or rule out cancer involvement.
It’s important to differentiate this clinical role from using DEXA as a diagnostic tool. In essence, DEXA provides supporting evidence in a broader diagnostic process rather than a standalone cancer detection method.
When a DEXA Scan Might Miss Bone-Related Cancer Indicators
While useful, DEXA has limitations that can result in missed indicators of bone involvement in cancer. For one, it focuses on BMD (bone mineral density) and does not detect lesions, cortical destruction, or soft-tissue extension that is often seen in metastatic bone disease. This makes it less reliable in cases of small or early lesions that haven’t yet caused significant mineral loss.
Additionally, DEXA measures density in specific zones (spine, hip, and forearm), meaning lesions outside these areas may go unnoticed. This limitation is critical when evaluating patients with cancers prone to metastasize to unusual skeletal locations. For example, in multiple myeloma, bone lesions may appear throughout the body—including the skull, ribs, and pelvis—which may or may not be covered by routine DEXA zones.

Complementary Imaging Tools for Confirming Suspected Cancer
When DEXA results indicate unexpected or asymmetric density changes, the next step involves more advanced imaging to clarify the nature of those findings. These include:
- MRI (Magnetic Resonance Imaging): Best for identifying marrow infiltration and small lesions.
- CT (Computed Tomography): Useful for visualizing cortical bone destruction.
- PET-CT (Positron Emission Tomography): Excellent for detecting metabolically active tumors.
- Bone Scintigraphy: Ideal for whole-skeleton imaging in search of widespread metastatic disease.
Each of these techniques plays a unique role in verifying or ruling out malignancy. DEXA is often the gateway—it flags abnormalities, prompting physicians to escalate diagnostic evaluation. Particularly in high-risk individuals, DEXA is part of a broader strategy that balances efficiency, cost, and radiation exposure.
Clinical Scenarios Where DEXA Aids in Cancer Management
There are several clinical settings where DEXA, while not diagnostic, supports cancer management protocols. These include:
- Pre-treatment assessment in hormone-sensitive cancers: For example, men with prostate cancer starting androgen deprivation therapy (ADT) often undergo a baseline DEXA to monitor skeletal health.
- Monitoring postmenopausal women with breast cancer: Especially if they’re on aromatase inhibitors that lower estrogen and contribute to bone loss.
- Long-term cancer survivorship plans: In patients at risk of osteoporosis due to treatment history, nutrition issues, or sedentary lifestyle.
In these cases, DEXA becomes part of the long-term surveillance strategy, helping clinicians balance cancer therapy benefits with risks to bone health. It also aids in determining the need for bone-protective agents like bisphosphonates or denosumab.
How DEXA Differs from Other Bone Imaging Modalities
Understanding how DEXA compares with other imaging modalities is critical for clinicians deciding on a diagnostic pathway. Unlike MRI or PET-CT, which provide detailed anatomical or functional data, DEXA is a dual-energy X-ray absorptiometry tool that focuses solely on bone mineral density (BMD). Its purpose is not to highlight structural lesions or abnormal cellular metabolism but to track quantitative bone loss over time.
This limitation makes DEXA less suited for initial cancer detection. However, its precision in measuring subtle changes in density makes it valuable in longitudinal cancer care, particularly in diseases where bone health is compromised by treatment. For example, patients with hormone-driven prostate cancer often suffer significant bone thinning during androgen deprivation therapy, which can be monitored effectively through DEXA.
DEXA Scan as a Preventive Tool in Cancer Survivorship
In oncology survivorship programs, prevention of secondary conditions like osteoporosis is a growing focus. DEXA scans are increasingly used to screen survivors for early signs of bone loss due to cancer treatment. Common scenarios include:
- Women on long-term anti-estrogen therapy after breast cancer.
- Men post-prostatectomy or receiving ADT.
- Childhood cancer survivors who received cranial irradiation or chemotherapy affecting bone development.
These groups may not show symptoms until fragility fractures occur. Regular DEXA scans allow early detection, ensuring interventions like calcium supplementation, vitamin D correction, or physical therapy can begin promptly. For survivors of cancers that did not originate in or metastasize to the bone, DEXA helps preserve long-term quality of life.
Cases Where DEXA Results Prompt Additional Cancer Work-Up
In rare cases, unexpected findings from a DEXA scan may prompt further investigation that ultimately leads to a cancer diagnosis. For example, an unusually low density in a young patient with no risk factors may raise concern for an underlying malignancy affecting bone metabolism, such as leukemia, lymphoma, or multiple myeloma.
The scan might also reveal asymmetrical density loss or localized deficits inconsistent with generalized osteoporosis. These findings don’t confirm cancer, but they often lead clinicians to order blood tests (such as serum protein electrophoresis or tumor markers) and advanced imaging to rule out occult disease.
As noted in our review of “Unfavorable intermediate risk prostate cancer,” layered diagnostic strategies like this are essential for nuanced cases.
Comparison of DEXA and Other Imaging Modalities in Cancer Context
| Imaging Type | Best For | Limitations | Radiation Exposure | Availability |
| DEXA | Bone mineral density; fracture risk | Cannot detect lesions; no tumor visualization | Very low | Widely available |
| MRI | Marrow infiltration; small lesions | Expensive; not good for cortical bone | None | Moderately available |
| CT | Cortical destruction; structural integrity | Higher radiation dose | Moderate to high | Widely available |
| PET-CT | Active tumor metabolism | Expensive; limited anatomical resolution | High | Specialized centers |
| Bone Scan | Widespread metastasis screening | Low specificity | Moderate | Widely available |
This table helps visualize when DEXA fits into clinical pathways and when other imaging methods are more appropriate, especially for oncology diagnostics.
DEXA Scanning in the Management of Myeloma and Lytic Lesions
DEXA scanning plays a supporting role in the management of multiple myeloma, particularly in assessing the risk of fractures and monitoring skeletal integrity during treatment. While it cannot directly visualize lytic lesions—which are hallmark signs of myeloma—it can provide essential data on bone mineral density (BMD), which often declines due to disease progression or corticosteroid therapy. The presence of widespread lytic damage is typically evaluated with more advanced imaging modalities, such as whole-body low-dose CT or MRI. However, DEXA remains valuable when used longitudinally to detect generalized bone loss in asymptomatic stages or to assess the success of bone-preserving strategies like bisphosphonates.
In some clinical pathways, DEXA is used alongside biochemical markers (such as serum calcium and β2-microglobulin) to help construct a comprehensive picture of disease burden and systemic bone weakening. Though not diagnostic of cancer itself, changes in BMD captured by DEXA may signal the need for urgent reevaluation or imaging escalation. For instance, if a patient with stable myeloma suddenly exhibits a marked decrease in BMD, this may prompt investigation for new lytic activity or disease relapse. Given the familial patterns sometimes observed in myeloma, as discussed in the article Is myeloma cancer hereditary, DEXA scans can serve as an early screening consideration for at-risk individuals.
Limitations of DEXA in Detecting Cancer Directly
Despite its widespread use in evaluating bone density, a DEXA scan is fundamentally limited when it comes to detecting cancer. Its resolution is insufficient to identify focal lesions, tumor masses, or metastatic deposits. DEXA images are low-contrast and provide only quantitative data on mineral content—not structural detail. Thus, while a significant reduction in BMD may raise clinical suspicion in the right context, the scan cannot indicate whether this change is due to osteoporosis, cancer, infection, or other metabolic bone diseases.
Another limitation is its inability to localize pathology. For example, a DEXA scan might report low BMD in the lumbar spine, but it cannot differentiate whether the cause is a benign compression fracture or lytic invasion by metastatic colon cancer. As such, abnormal findings require follow-up with diagnostic tools like MRI or PET-CT for localization and characterization. Clinicians must also be cautious not to overinterpret DEXA data when managing oncology patients—especially when multiple factors, such as age, nutrition, and medication use, affect bone health.n metastatic gastrointestinal cancers, such as those involving the peritoneum, the limitations of DEXA are especially evident, necessitating higher-resolution imaging as outlined in Colon cancer metastasis peritoneum.
Clinical Guidelines and Recommendations for Use of DEXA in Oncology
Professional societies such as the American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) have issued clear guidance on the appropriate use of DEXA in cancer management. These guidelines primarily recommend DEXA scanning for patients at increased risk of bone loss, including those undergoing:
- Hormone therapies (e.g., aromatase inhibitors, androgen deprivation therapy)
- Chemotherapy regimens affecting calcium metabolism
- Long-term corticosteroid use
In these contexts, DEXA serves not as a diagnostic test for cancer itself, but rather as a surveillance tool for assessing secondary effects of treatment on skeletal health. It enables clinicians to initiate early interventions such as vitamin D supplementation, bisphosphonates, or weight-bearing exercise protocols. Importantly, the timing of scans is also emphasized. A baseline DEXA is typically obtained before treatment initiation, with follow-up every 12 to 24 months based on patient-specific factors.
It’s crucial that oncologists interpret DEXA results not in isolation but as part of a broader clinical picture. For example, a drop in BMD in a patient receiving androgen deprivation therapy must be weighed against the therapy’s benefits in controlling high-risk prostate cancer.
Future Developments in Bone Imaging and AI Integration
Emerging technologies promise to extend the role of DEXA beyond traditional bone density measurement. One of the most exciting areas is artificial intelligence (AI), which could enhance the interpretation of DEXA scans by identifying subtle patterns that correlate with disease progression or fracture risk. Machine learning algorithms may soon allow automated analysis that adjusts for age, race, and comorbidities, offering predictive insights far beyond current capabilities.
Another innovation is 3D-DXA technology, which attempts to reconstruct volumetric models of bone from standard 2D scans. This could allow for more accurate assessment of trabecular and cortical bone architecture—important in cancer patients who may experience asymmetric or focal bone loss.
There is also growing interest in combining DEXA data with genomic and biochemical markers to create comprehensive risk profiles. This integrative approach may one day identify patients not only at risk for osteoporosis, but also for skeletal complications of cancer, long before symptoms appear. While these developments are still in research phases, they represent a future where bone imaging becomes more dynamic, individualized, and informative.
FAQ
Can a DEXA scan detect cancer directly?
No, a DEXA scan cannot detect cancer directly. It is designed to measure bone mineral density, not soft tissue masses or malignant lesions. Although certain abnormalities on a DEXA scan—like unexpected bone loss—might raise suspicion, the scan lacks the resolution and specificity to identify cancerous growths on its own.
What does a DEXA scan actually measure?
DEXA measures bone mineral density (BMD), providing a quantitative assessment of bone strength. It compares a patient’s results to standardized references, producing a T-score and Z-score that indicate risk levels for conditions like osteoporosis or osteopenia.
Why might a cancer patient need a DEXA scan?
Many cancer patients are at risk of treatment-induced bone loss. For example, those on chemotherapy, hormone therapy (like tamoxifen or androgen deprivation), or corticosteroids may experience decreased bone density. A DEXA scan is used to monitor and manage this risk.
Can a DEXA scan show bone metastasis?
No, it cannot visualize metastatic lesions. Bone metastases require imaging like PET, MRI, or CT to be accurately detected. However, if there’s substantial bone loss due to metastasis, the DEXA scan may show reduced BMD, prompting further evaluation.
Is DEXA scanning useful for multiple myeloma?
While DEXA is not the primary diagnostic tool for multiple myeloma, it can monitor bone density in patients at risk of fractures or osteoporosis caused by the disease or its treatment. Other tools, such as whole-body CT or skeletal surveys, are more informative for direct lesion visualization.
Are there cancers associated with significant bone density changes?
Yes. Breast, prostate, and multiple myeloma often affect bone density. Bone metastases can cause bone destruction, while treatments for these cancers can also decrease BMD. Monitoring with DEXA is crucial in long-term care for these patients.
Can a DEXA scan distinguish between benign and malignant bone changes?
No. DEXA does not offer the imaging detail necessary to distinguish the cause of bone density changes. It cannot differentiate between changes caused by benign conditions like osteoporosis and those from malignancy.
Does a low T-score mean you have cancer?
Not necessarily. A low T-score suggests decreased bone density, often due to aging or hormonal changes, not cancer. However, in some contexts—especially in younger individuals or those with unexplained bone loss—it might warrant further cancer screening.
How often should cancer patients receive a DEXA scan?
This depends on cancer type and treatment. Patients on therapies known to reduce bone density may need baseline scans before treatment and follow-up every 1–2 years. Guidelines vary by age, sex, and clinical factors.
What other imaging is used alongside DEXA in cancer care?
Other imaging includes MRI, PET-CT, whole-body bone scans, and X-rays. These are used to detect metastasis, evaluate tumor burden, and guide treatment planning. DEXA plays a supplementary role, particularly in bone health surveillance.
Is DEXA covered by insurance for cancer patients?
In many cases, yes—especially when there’s a clinical indication such as hormone therapy, chemotherapy, or corticosteroid use. Coverage varies depending on country, insurer, and clinical guidelines, so pre-authorization is often needed.
How does a DEXA scan compare to CT or MRI in cancer detection?
DEXA is limited to measuring bone density, while CT and MRI provide detailed anatomical views and are capable of detecting masses, tissue changes, and bone lesions. DEXA is not a substitute but rather a complementary tool for bone monitoring.
What risks are associated with DEXA scans?
DEXA uses very low levels of radiation—far less than CT or standard X-rays. It is considered extremely safe, even for repeated use, which makes it ideal for long-term monitoring.
Can DEXA be used for early cancer screening?
Not directly. It is not a screening tool for cancer. However, in certain scenarios, abnormal findings on a DEXA scan may prompt clinicians to investigate further, especially if the pattern of bone loss is unusual or rapid.
What’s the future of DEXA in oncology?
As artificial intelligence becomes integrated, DEXA may play a larger role in cancer risk modeling. New technologies could allow 3D imaging and improved lesion detection when used in combination with other data sources, expanding its utility beyond bone density alone.









