Can a Bone Density Test Detect Cancer? A Complete Medical Insight
- Understanding What a Bone Density Test Measures
- Can Bone Density Tests Reveal Early Signs of Cancer?
- Symptoms That Might Prompt a Bone Density Test in Cancer Patients
- Limitations of Bone Density Scans in Detecting Cancer
- When Should a Bone Density Test Raise Concern About Cancer?
- Comparing Diagnostic Imaging Tools for Bone Cancer Detection
- How Cancer Treatments Affect Bone Density
- Secondary Bone Cancer vs. Osteoporosis: How to Tell the Difference
- Bone Density Testing in Cancer Survivors: A Tool for Long-Term Monitoring
- Can Bone Density Changes Signal Cancer Recurrence?
- Are There Blood Tests That Complement Bone Density for Cancer Detection?
- What to Expect During a Bone Density Test and How to Prepare
- Preventing Bone Loss in Cancer Patients: Practical Strategies
- Advances in Bone Imaging Technology
- How Bone Density Testing Is Integrated Into Routine Oncology Care
- The Importance of a Multidisciplinary Approach
- FAQ – Frequently Asked Questions About Bone Density Tests and Cancer

Understanding What a Bone Density Test Measures
A bone density test, or dual-energy X-ray absorptiometry (DEXA), measures the mineral content in bones—most often in the hip, spine, or forearm. The result, reported as a T-score, indicates how much bone mass a person has compared to a healthy young adult. Scores below –1 suggest decreased density, while scores below –2.5 indicate osteoporosis.
The scan is non-invasive, quick, and low in radiation exposure, making it ideal for screening large populations or monitoring gradual bone changes over time. However, the DEXA scan does not create detailed three-dimensional images like CT or MRI. Instead, it provides a density value, which reflects the mineral concentration—not tissue architecture, bone shape, or structural abnormalities.
When it comes to detecting cancer, this presents both strengths and limitations. While the test can hint at underlying problems, it cannot independently identify tumors. Instead, it may raise red flags that trigger further testing, especially when results are unexpected or asymmetric.
Can Bone Density Tests Reveal Early Signs of Cancer?
In some cases, yes—but not directly. While bone density tests are not designed to diagnose cancer, they can reveal abnormalities that prompt further investigation. For instance, a sudden and unexplained drop in bone density, especially in a localized area, may suggest a secondary issue such as bone metastasis.
Certain cancers—most notably breast, prostate, and lung cancers—are known to spread to bone. These metastatic lesions can cause the bone to weaken (lytic lesions), harden (blastic lesions), or fluctuate in density (mixed lesions). Although DEXA doesn’t distinguish between types of lesions, a rapid change in density or significant asymmetry between limbs may alert clinicians to the need for advanced imaging.
Moreover, for patients already diagnosed with cancer, bone density monitoring can be an essential part of long-term care. Chemotherapy, radiation, and hormone therapy—especially aromatase inhibitors in breast cancer—can accelerate bone loss. Detecting these changes early allows for prompt intervention.
As discussed in our article on c reactive protein and cancer, elevated inflammatory markers alongside bone changes may further strengthen the suspicion of metastatic or systemic disease, especially in patients with ongoing fatigue, weight loss, or unexplained pain.
Symptoms That Might Prompt a Bone Density Test in Cancer Patients
Cancer patients, particularly those with known risk factors or established malignancy, often report nonspecific bone-related symptoms. These may include persistent back or hip pain, height loss, frequent fractures, or even generalized weakness. While these symptoms are not cancer-specific, they frequently overlap with both osteoporosis and skeletal metastases.
In such cases, a bone density test serves two functions. First, it can evaluate the degree of bone thinning—critical in patients at risk for fractures. Second, it can detect abrupt, asymmetric, or focal drops in bone density that are inconsistent with age-related osteoporosis.
If a patient presents with sudden-onset vertebral compression, bone pain at rest, or radiologic signs of cortical thinning, clinicians may follow up a DEXA scan with bone scintigraphy, MRI, or PET-CT to rule out or confirm cancer involvement.
In patients who are post-treatment and experiencing skeletal pain, a bone density test may also be used to determine whether the discomfort is due to therapy-related osteopenia or more serious oncologic concerns.
Limitations of Bone Density Scans in Detecting Cancer
Despite their utility, bone density tests are not designed to detect malignancy. The test lacks the spatial resolution and tissue contrast needed to visualize tumors or metastatic lesions directly. It provides no information about the soft tissue structures, bone marrow, or tumor margins.
Additionally, cancer can exist in the bone without causing changes in mineral density—especially in early stages. Some lytic lesions may develop subtly or in areas not covered by routine DEXA protocols, such as the ribs, skull, or upper extremities.
DEXA scans also cannot differentiate between causes of low density. A reading that suggests osteopenia might reflect natural aging, medication effects, nutritional deficiencies, or underlying cancer—but it cannot tell which without further context.
For these reasons, bone density tests are considered supportive tools rather than diagnostic instruments in oncology. They raise flags, guide treatment safety, and help monitor therapy side effects—but they must be combined with other clinical data to guide definitive conclusions.
When Should a Bone Density Test Raise Concern About Cancer?
Although bone density tests are not diagnostic for cancer, there are specific scenarios where their results may suggest the need for additional cancer-focused investigations. A sudden, dramatic loss in bone mineral density over a short period—particularly in a younger patient or someone with no risk factors for osteoporosis—warrants further evaluation.
Focal changes in density, such as significant loss in one hip but not the other, or a compressed vertebra in an otherwise healthy bone matrix, may also indicate potential underlying pathology. Similarly, if a patient undergoing cancer treatment shows rapid declines in bone health despite supportive therapy, metastasis should be considered in differential diagnosis.
In such cases, the bone density test acts as an early signal—not a standalone diagnostic—but an invitation to expand the clinical view with CT, MRI, or bone-specific nuclear imaging.

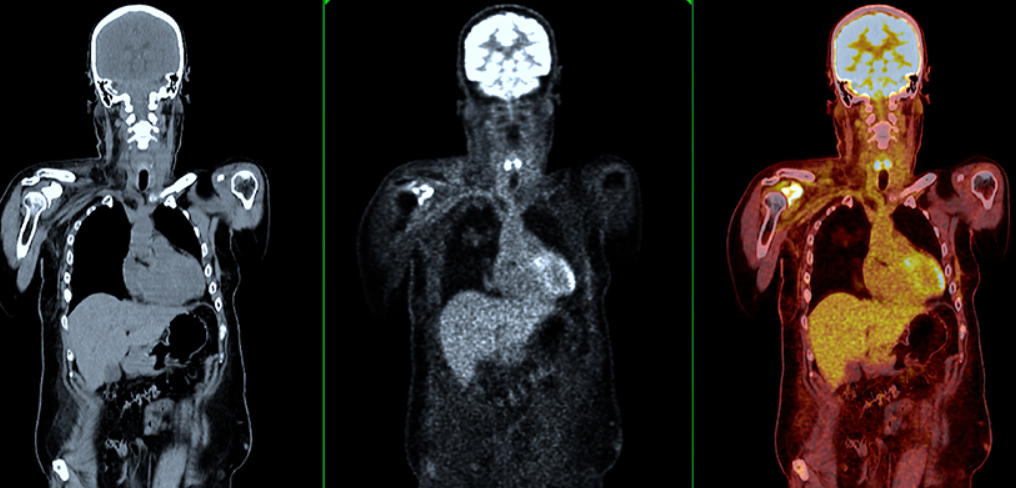
Comparing Diagnostic Imaging Tools for Bone Cancer Detection
The table below summarizes how bone density testing compares to other imaging modalities used in the evaluation of cancer affecting the bones:
| Imaging Modality | Primary Use | Strengths | Limitations |
| DEXA (Bone Density Scan) | Measures bone mineral density | Quick, low-radiation, good for monitoring bone loss | Cannot detect tumors or differentiate lesion types |
| X-ray | Detects fractures, large lesions | Widely available, fast | Poor at visualizing early or subtle bone changes |
| CT Scan | Detailed bone and soft tissue anatomy | Good spatial resolution | Higher radiation exposure, less soft tissue contrast |
| MRI | Soft tissue and marrow involvement | Best for detecting bone marrow and soft tissue tumors | Time-consuming, expensive |
| Bone Scintigraphy (Bone Scan) | Whole-body detection of metastases | Highly sensitive to changes in bone metabolism | Not specific—false positives possible |
| PET-CT | Functional and structural imaging combined | Detects active tumor metabolism and spread | Expensive, not ideal for initial screening |
The choice of imaging depends on clinical suspicion, cancer type, and availability. Bone density scans provide a safe, accessible entry point, but their results must be interpreted alongside other tests when cancer is suspected.
How Cancer Treatments Affect Bone Density
Many cancer therapies negatively impact bone health. Chemotherapy can interfere with bone remodeling, while hormone therapies—such as androgen deprivation in prostate cancer or aromatase inhibitors in breast cancer—accelerate bone loss. Radiation to the pelvis or spine may also damage bone cells directly, leading to localized osteopenia or even necrosis.
These changes can be insidious, which is why patients undergoing long-term systemic therapy often undergo baseline and follow-up DEXA scans. Identifying bone loss early allows for timely intervention with calcium, vitamin D, bisphosphonates, or RANK-ligand inhibitors to prevent fractures and maintain function.
Interestingly, new forms of cancer immunotherapy, such as those being explored in the development of the breast cancer vaccine 2025, are being evaluated for their potential to reduce systemic inflammation while preserving bone integrity—suggesting a dual benefit in oncologic care.

Secondary Bone Cancer vs. Osteoporosis: How to Tell the Difference
Distinguishing between osteoporosis and secondary bone cancer can be challenging, especially since both conditions may produce similar symptoms like fractures, back pain, or height loss. However, there are key clinical and radiologic differences that guide diagnosis:
Osteoporosis usually presents with diffuse bone loss that is symmetric and age-related. Fractures often occur at predictable sites—spine, hip, wrist—and lab values tend to be normal aside from calcium and vitamin D levels.
Bone metastases, on the other hand, may cause localized bone destruction (lytic lesions), abnormal bone hardening (blastic lesions), or irregular cortical disruptions visible on advanced imaging. Blood work may show elevated alkaline phosphatase or inflammatory markers.
When a patient with known cancer presents with new skeletal complaints or abnormal DEXA results, physicians will typically move quickly to rule out metastasis before assuming benign causes.
Bone Density Testing in Cancer Survivors: A Tool for Long-Term Monitoring
Survivors of cancer often face long-term side effects from treatment, and skeletal health is one of the most vulnerable areas. After chemotherapy, radiation, or hormonal therapy, many patients—especially women—experience accelerated bone loss that persists even after remission.
Bone density tests are invaluable in this context. They provide baseline and follow-up data to help track changes in bone mineral content over time. For postmenopausal women treated for breast cancer, regular DEXA scans are often integrated into survivorship care plans to prevent fractures and maintain mobility.
These tests also help oncologists determine whether supportive interventions like bisphosphonates, denosumab, or weight-bearing exercise are having a protective effect. By identifying osteopenia early, patients can avoid severe osteoporosis and the associated risk of fractures.
Can Bone Density Changes Signal Cancer Recurrence?
In some cases, yes—particularly when combined with other clinical signs. A sudden drop in bone density, particularly at a single site or over a short time frame, can signal metastatic recurrence in patients with prior cancers known to spread to the skeleton.
This is especially relevant for breast, prostate, lung, and renal cancers, which have a high affinity for bone. If a patient with a history of breast cancer shows localized bone density loss at the hip, spine, or pelvis, and reports new bone pain or fatigue, it may indicate recurrence.
In those previously treated for breast cancer metastasis to skin [вставить ссылку по смыслу], the appearance of new bone symptoms or rapidly declining DEXA values may mark systemic progression. While a DEXA scan won’t confirm metastasis, it plays a role in raising clinical suspicion, prompting timely CT or PET-CT scanning.
Are There Blood Tests That Complement Bone Density for Cancer Detection?
Yes, several blood-based biomarkers can support the interpretation of bone density findings, especially when malignancy is suspected. These include:
- Alkaline phosphatase (ALP): Often elevated in cases of bone metastasis or high bone turnover.
- Calcium: Hypercalcemia may occur in cancers with bone involvement, such as multiple myeloma or advanced breast cancer.
- C-telopeptide (CTX) and N-telopeptide (NTX): Markers of bone resorption, elevated in both osteoporosis and bone-destructive tumors.
- Parathyroid hormone (PTH): Assesses calcium regulation, which may be altered in cancer.
These labs are not diagnostic on their own, but when viewed alongside DEXA results and imaging, they contribute to a more complete picture. If blood markers are abnormal and DEXA reveals focal loss, metastatic workup becomes an immediate priority.
What to Expect During a Bone Density Test and How to Prepare
Undergoing a bone density scan is a straightforward process. The patient lies on a padded table while a scanning arm passes over the lower spine and hips, capturing X-ray images at two energy levels to calculate bone mineral content.
No injections, contrast agents, or special preparation are required. The entire test takes about 15 minutes and is painless. Patients are advised to avoid taking calcium supplements within 24 hours prior to the scan, as this can affect accuracy.
Test results are typically available within a few days and include T-scores and Z-scores. These values are interpreted by radiologists and forwarded to the primary care physician or oncologist, who will explain their relevance in the context of the patient’s age, medical history, and cancer treatment.
Preventing Bone Loss in Cancer Patients: Practical Strategies
While not all bone density changes are preventable, many patients—especially those undergoing long-term treatment—can significantly reduce their risk of fractures and osteoporosis with proactive care. This includes lifestyle measures, pharmacologic support, and ongoing monitoring.
Key strategies involve adequate calcium and vitamin D intake, resistance and weight-bearing exercises, smoking cessation, and limiting alcohol consumption. Medications like bisphosphonates or denosumab are often prescribed to high-risk individuals, particularly those on aromatase inhibitors or corticosteroids.
Patients should also be educated about fall prevention, including proper footwear, vision correction, and home safety adaptations. Integrating these measures into oncology care plans ensures that bone health is protected alongside tumor control.

Advances in Bone Imaging Technology
Though DEXA remains the gold standard for bone density assessment, new technologies are emerging to improve diagnostic sensitivity and functional analysis. High-resolution peripheral quantitative CT (HR-pQCT) allows for microstructural evaluation of bones, identifying early signs of weakness not detectable by DEXA.
Magnetic resonance imaging (MRI) is also being optimized for bone marrow analysis, helping distinguish between degenerative changes and neoplastic infiltration. Some PET tracers now target bone metabolism specifically, offering a hybrid view of function and anatomy in cancer patients.
These technologies are especially helpful when DEXA results are inconclusive but clinical suspicion remains high. While not used routinely, they are invaluable tools in complex oncology cases or for patients with recurrent skeletal symptoms despite normal DEXA scores.
How Bone Density Testing Is Integrated Into Routine Oncology Care
In modern oncology, bone density evaluation is becoming routine—especially for breast and prostate cancer patients. Baseline DEXA scans are often ordered before initiating hormone-modulating therapy, and follow-up scans are timed to detect early decline.
Results are used to guide supplementation protocols, lifestyle recommendations, and the initiation of bone-strengthening drugs. For older adults or those with additional risk factors (e.g., sedentary lifestyle, low BMI, corticosteroid use), bone monitoring becomes a key aspect of survivorship planning.
The integration is not limited to monitoring. In certain cases, abnormal bone density trends can help unmask hidden disease progression or justify switching systemic therapies. Oncologists now view DEXA not only as a fracture-prevention tool but also as a potential indicator of broader oncologic status.
The Importance of a Multidisciplinary Approach
Managing bone health in cancer patients requires coordinated care among multiple specialists. Oncologists oversee systemic therapy and determine monitoring frequency. Endocrinologists address underlying bone disorders, such as hyperparathyroidism or treatment-induced osteoporosis. Radiologists interpret imaging results with a trained eye for subtle abnormalities.
Physical therapists may help design safe, effective exercise plans to enhance skeletal strength. Nutritionists contribute to optimizing calcium, protein, and vitamin D intake. Primary care physicians play a key role in long-term follow-up and screening.
This multidisciplinary collaboration ensures that bone-related complications are not overlooked in the pursuit of tumor control. It also helps maintain mobility, independence, and quality of life—critical goals for any patient navigating the cancer continuum.
FAQ – Frequently Asked Questions About Bone Density Tests and Cancer
Can a bone density test detect cancer directly?
No, a bone density (DEXA) scan cannot directly detect cancer. It measures bone mineral content and highlights changes in density, but it does not visualize tumors or metastases. However, unusual or asymmetric findings may prompt further cancer-focused imaging.
When might a bone density scan suggest something more serious?
A sudden or localized drop in bone density—especially in a patient with a history of cancer—may suggest bone metastasis or another underlying pathology. If results deviate significantly from expected age-related patterns, additional imaging is often recommended.
Which cancers most commonly affect bone density?
Breast, prostate, and lung cancers are the most likely to spread to bone and cause changes in density. Hematologic cancers like multiple myeloma can also weaken bones, sometimes presenting as the first sign of disease.
Can osteoporosis be confused with bone cancer on a scan?
Yes, particularly in early stages. Both conditions may show reduced bone mass or fragility. However, cancer often causes more focal destruction or irregular patterns, while osteoporosis tends to be diffuse and symmetrical.
Are there blood tests that support bone cancer diagnosis?
Yes. Elevated alkaline phosphatase, abnormal calcium levels, or specific tumor markers can all provide clues. These labs are especially helpful when used alongside DEXA results and other imaging studies like PET or MRI.
Is a bone density test painful or invasive?
No, the test is completely non-invasive and painless. Patients lie on a flat surface for about 10–15 minutes while a scanner measures the spine and hips. There’s no need for injections or contrast material.
How often should cancer patients get a DEXA scan?
That depends on cancer type and treatment. Patients on aromatase inhibitors, androgen deprivation, or long-term corticosteroids typically receive baseline and periodic follow-up scans every 12 to 24 months.
Can a normal bone density test rule out cancer?
No. Cancer may still be present even if bone density is normal, especially in the early stages or if metastases are isolated and small. A normal DEXA result cannot replace other diagnostic methods if symptoms persist.
What symptoms suggest the need for a bone density test in cancer patients?
Back pain, unexplained fractures, height loss, or sudden skeletal weakness should prompt evaluation. In these scenarios, a DEXA scan may serve as an initial tool, particularly when paired with inflammatory or tumor markers like those discussed in c reactive protein and cancer.
Do bone-targeting cancer treatments affect density test results?
Yes. Treatments like bisphosphonates or denosumab can improve bone mineral density and reduce fracture risk. Their effect can be monitored with DEXA scans over time to assess therapeutic benefit.
Can bone density scans detect metastasis in skin-related breast cancer cases?
Not directly, but if patients previously diagnosed with breast cancer metastasis to skin present with new bone symptoms or fragility, a DEXA scan may raise suspicion for further skeletal spread.
Is bone loss reversible after cancer treatment?
In many cases, yes. Early detection through DEXA allows for timely intervention with medications, supplements, and lifestyle changes. Rebuilding bone density is possible, though it requires long-term management.
Can immunotherapy or vaccines affect bone density?
Some emerging therapies, including those like the breast cancer vaccine 2025, are being studied for their interaction with bone health. While not directly designed to protect bone, reduced inflammation may have a secondary benefit.
Is bone density testing safe for repeated use?
Yes. DEXA uses minimal radiation, far less than a chest X-ray, and is safe for regular monitoring. It is approved for use even in elderly or frail patients and can be repeated as clinically indicated.
How is a DEXA scan different from a bone scan?
A DEXA scan measures mineral density, while a bone scan (scintigraphy) detects metabolic activity—often from cancer, infection, or fracture. They are complementary tools and used in different diagnostic scenarios.










