Understanding Breast Cancer Without a Lump: A Comprehensive GuideBreast Cancer no Lump
- Recognizing Non-Lump Symptoms of Breast Cancer
- The Role of Imaging in Detecting Non-Palpable Breast Cancer
- Understanding Inflammatory Breast Cancer (IBC)
- The Importance of Regular Screening and Self-Examination
- Diagnostic Challenges in Absence of a Lump
- Types of Breast Cancer Likely to Present Without a Lump
- Treatment Options for Non-Lump Presenting Breast Cancer
- Comparing Imaging Modalities: Strengths and Limitations
- Understanding Breast Cancer Staging Without a Lump
- The Role of Hormone Receptors and HER2 in Non-Lump Cancers
- Risk Factors for Non-Lump Breast Cancers
- Psychological Impact and Delayed Diagnosis
- Navigating Treatment When a Mass is Not Visible
- Lifestyle Modifications and Post-Treatment Monitoring
- Ongoing Research and Clinical Trials
- Why Awareness of Non-Lump Breast Cancer Matters
- Frequently Asked Questions (FAQ)
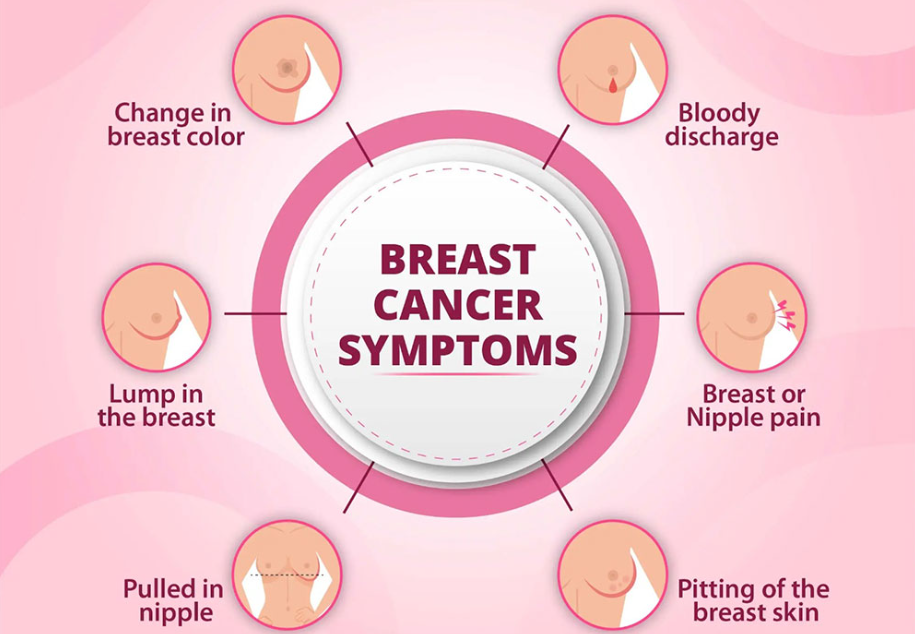
Recognizing Non-Lump Symptoms of Breast Cancer
While a lump in the breast is a well-known indicator of breast cancer, it’s crucial to understand that not all breast cancers present this way. In fact, certain types of breast cancer, such as inflammatory breast cancer (IBC) and ductal carcinoma in situ (DCIS), often do not form a distinct lump. Instead, they may exhibit other signs that are equally important to recognize.
Symptoms to be aware of include:
- Changes in breast size or shape
- Skin dimpling or puckering
- Redness or a rash on the breast
- Nipple inversion or discharge
- Persistent breast pain
- Swelling in the armpit or around the collarbone
These symptoms can be subtle and may be mistaken for benign conditions. Therefore, it’s essential to consult a healthcare provider if any of these changes are observed.
The Role of Imaging in Detecting Non-Palpable Breast Cancer
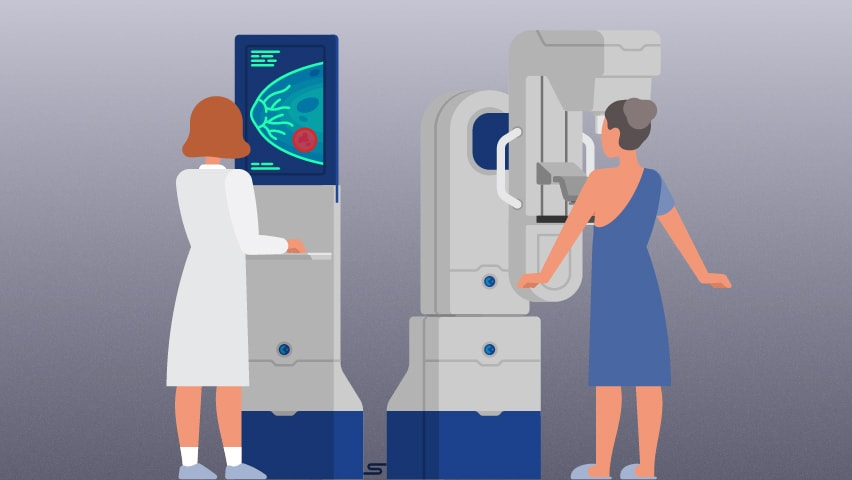
Detecting breast cancer without a palpable lump relies heavily on imaging techniques. Mammography remains a standard screening tool; however, its effectiveness can be limited in individuals with dense breast tissue. In such cases, additional imaging modalities like ultrasound and magnetic resonance imaging (MRI) are employed to enhance detection rates.
For instance, a UK study highlighted that enhanced cancer screening for women with very dense breasts could detect additional breast cancer cases annually and potentially save lives.
These imaging techniques can reveal abnormalities such as architectural distortions, asymmetries, or microcalcifications that may not be palpable during a physical examination. Early detection through imaging is vital for initiating timely treatment and improving prognosis.
Understanding Inflammatory Breast Cancer (IBC)
Inflammatory breast cancer is a rare but aggressive form of breast cancer that often lacks a distinct lump. Instead, it presents with symptoms resulting from cancer cells blocking lymph vessels in the skin. These symptoms can include:
- Redness and warmth in the breast
- Swelling and heaviness
- Skin thickening resembling an orange peel (peau d’orange)
- Nipple inversion
Due to its rapid progression and atypical presentation, IBC is often diagnosed at a more advanced stage. Prompt recognition of these signs and immediate medical evaluation are crucial for effective management.
The Importance of Regular Screening and Self-Examination
Regular breast cancer screening is vital, especially for detecting cancers that do not present with a lump. Mammograms can identify early signs of cancer, such as microcalcifications or structural changes, before symptoms develop. For individuals with dense breast tissue, supplemental screening methods like ultrasound or MRI may be recommended.
In addition to professional screenings, self-examination plays a critical role in early detection. Individuals should become familiar with the normal look and feel of their breasts to identify any unusual changes promptly. Early detection through these methods significantly increases the chances of successful treatment outcomes.
Diagnostic Challenges in Absence of a Lump
Diagnosing breast cancer without a palpable lump presents unique difficulties for both patients and clinicians. Because many assume that breast cancer always forms a noticeable mass, other warning signs can be overlooked or misattributed to benign conditions like mastitis, dermatitis, or hormonal changes.
In cases such as inflammatory breast cancer or early-stage ductal carcinoma in situ (DCIS), physical findings may be limited to skin changes, localized discomfort, or nipple abnormalities. These symptoms are often subtle and progress rapidly, leaving little time for delayed evaluation.
Mammograms may reveal early indicators like microcalcifications, which are often the first detectable sign of malignancy in non-palpable cancers. These calcifications appear as tiny, white specks and can suggest abnormal cell growth, even before invasive cancer develops. Similar diagnostic relevance is seen in other endocrine malignancies — for example, medullary thyroid cancer microcalcifications often guide early intervention and reflect biologic aggressiveness.
To overcome these diagnostic obstacles, a combination of high-sensitivity imaging, tissue biopsy, and clinical vigilance is essential. Radiologists and primary care physicians must be trained to recognize non-traditional presentations, particularly in high-risk populations or those with dense breast tissue.
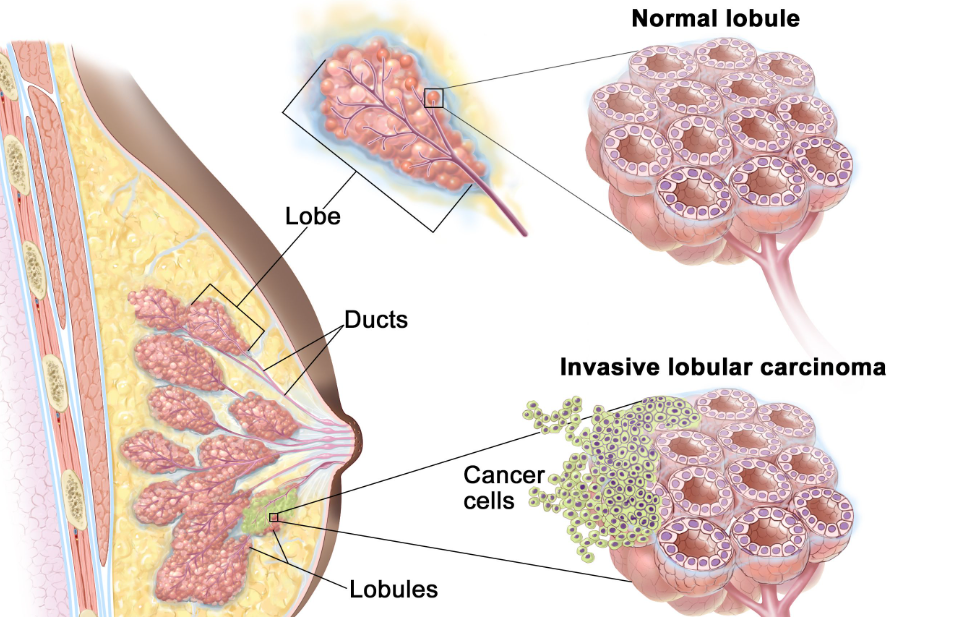
Types of Breast Cancer Likely to Present Without a Lump
While any form of breast cancer could theoretically present without a lump in its earliest stage, some subtypes are more commonly associated with this presentation. Among them are:
- Inflammatory breast cancer (IBC): Rare, fast-growing, and often diffuse with skin involvement
- Ductal carcinoma in situ (DCIS): Non-invasive and typically detected through mammography rather than physical findings
- Lobular carcinoma in situ (LCIS): A marker for increased risk rather than a true cancer, but often invisible clinically
- Paget’s disease of the nipple: Presents as eczematous changes, crusting, or burning localized to the nipple-areola complex
- Occult breast cancer: Cancer first discovered through metastasis to axillary lymph nodes without any visible primary tumor in the breast
These subtypes may go unnoticed during self-exams or routine checkups, making imaging and awareness critical. Moreover, their management may differ slightly, as surgical decisions, systemic therapies, and follow-up protocols must account for limited physical manifestation.
Treatment Options for Non-Lump Presenting Breast Cancer
Once breast cancer is diagnosed — even in the absence of a lump — the treatment plan follows established oncological principles, tailored to the cancer type, stage, and biology. Most treatment strategies include a multimodal approach:
- Surgery is often performed to remove identified cancerous tissue, even when the lesion is non-palpable. Wire-guided or MRI-guided localization may be necessary during surgery for accurate targeting.
- Radiation therapy is commonly used post-lumpectomy or when the skin is involved, as seen in inflammatory breast cancer.
- Systemic therapy, including chemotherapy, hormonal therapy, and targeted agents (e.g., HER2 inhibitors), is chosen based on molecular subtype and staging.
In some cases, neoadjuvant therapy (treatment before surgery) is recommended to shrink the disease or control inflammatory spread. The absence of a lump does not reduce the cancer’s severity — in fact, some types like IBC are considered more aggressive and require urgent treatment.
This is reminiscent of aggressive treatment regimens used in other fast-progressing cancers, such as the dense dose doxorubicin and cyclophosphamide protocol in high-risk breast cancers.
Comparing Imaging Modalities: Strengths and Limitations
Accurate imaging is essential in cases where a lump is absent but suspicion of breast cancer remains. The choice of modality depends on patient-specific factors such as age, breast density, and previous findings.
| Imaging Modality | Advantages | Limitations |
| Mammography | Effective for detecting calcifications and structural changes | Less sensitive in dense breasts; may miss subtle non-mass lesions |
| Ultrasound | Good for evaluating palpable areas and guiding biopsy | Operator-dependent; limited for detecting small or diffuse abnormalities |
| MRI (with contrast) | Highly sensitive for non-palpable and dense-tissue cases | Expensive; may lead to false positives or overdiagnosis |
| Tomosynthesis (3D) | Enhances lesion visibility and reduces tissue overlap | Still evolving as standard; access may be limited in smaller centers |
A combined approach often yields the best diagnostic outcome. For example, MRI is frequently employed in patients with known genetic mutations or prior inconclusive mammograms. Similarly, digital breast tomosynthesis offers improved spatial resolution in difficult cases.
The strategic use of imaging is as central in breast cancer as MRI-guided ablation in prostate cancer therapies like TULSA-PRO, where the lesion may also be invisible to touch but not to technology.
Understanding Breast Cancer Staging Without a Lump
Staging breast cancer helps determine the extent of disease and guides treatment planning. When cancer presents without a palpable lump, staging becomes more reliant on imaging, biopsy findings, and pathology reports than physical measurements of tumor size.
The TNM system — Tumor size, Node involvement, and Metastasis — is still used, but “T” (tumor) is measured by imaging or microscopic analysis. For example, ductal carcinoma in situ (DCIS) is considered Stage 0, while inflammatory breast cancer is classified at least Stage III due to skin and lymphatic involvement.
In cases like occult breast cancer, the absence of a primary tumor in the breast but presence of metastatic cells in axillary lymph nodes may still result in staging from II to IV, depending on spread.
It’s important to understand that even a cancer without a mass can be biologically aggressive, depending on its molecular subtype. Therefore, clinical staging may not always reflect prognosis accurately, and genomic assays are often used in tandem for more precise decision-making.
The Role of Hormone Receptors and HER2 in Non-Lump Cancers
Breast cancers — regardless of whether they present as a lump — are often classified by receptor status. The three most important biomarkers are estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2).
These receptors define the molecular subtype of the tumor and influence systemic therapy decisions:
- ER/PR-positive tumors are often responsive to hormonal therapy such as tamoxifen or aromatase inhibitors.
- HER2-positive cancers are treated with targeted therapies like trastuzumab or pertuzumab.
- Triple-negative cancers, which lack all three receptors, are typically more aggressive and treated with chemotherapy.
Non-lump cancers like inflammatory breast cancer or Paget’s disease can occur across any of these subtypes. Their receptor status is determined by core biopsy, and this information is critical to tailoring treatment — especially since physical findings may be limited.
Risk Factors for Non-Lump Breast Cancers
The risk factors for developing breast cancer without a lump are largely similar to those for other types of breast cancer but may also include unique clinical and genetic patterns. These include:
- Genetic mutations such as BRCA1/2 or TP53, which increase the risk of aggressive or early-onset cancers
- High breast density, which reduces sensitivity of mammography and may delay detection
- Family history, especially in first-degree relatives
- Radiation exposure, particularly during adolescence
- Previous history of atypical ductal or lobular hyperplasia
It’s worth noting that many non-lump presentations are discovered incidentally during high-risk surveillance. This highlights the importance of advanced screening tools and genetic counseling in women with known risk factors.
Interestingly, similar principles apply in other cancers — for example, medullary thyroid cancer often presents without a visible nodule but can be identified early through targeted screening and imaging. Awareness of risk patterns across specialties can lead to earlier, life-saving diagnoses.
Psychological Impact and Delayed Diagnosis
One of the most challenging aspects of non-lump breast cancer is the emotional toll it can take on patients — especially when diagnosis is delayed due to misleading or absent physical signs. Many patients report feeling dismissed or misunderstood during early clinical visits, as visible skin changes or nipple issues are often attributed to benign causes.
This delay not only increases anxiety but may also affect prognosis if treatment is not initiated promptly. For conditions like inflammatory breast cancer or Paget’s disease, where time is a critical factor, any delay in diagnosis may allow for significant progression.
Moreover, receiving a cancer diagnosis without having felt a “lump” can lead to confusion, distrust in medical systems, and fear of missing symptoms again in the future. Comprehensive patient education, empathetic communication, and psychological support are essential throughout the diagnostic and treatment journey.
Survivorship programs and mental health counseling — often overlooked in oncology care — can play a vital role in restoring confidence and emotional resilience, especially in these atypical breast cancer presentations.

Navigating Treatment When a Mass is Not Visible
When there is no defined mass, treatment decisions rely on imaging findings, biopsy pathology, receptor status, and extent of skin or lymph node involvement. Surgical planning often requires advanced localization techniques such as:
- Wire localization, where a thin wire is placed under imaging guidance to mark the area of concern
- Radio-guided seed localization, which uses a small radioactive seed to help the surgeon find the exact tissue
- MRI-guided surgery, particularly in cases involving dense breast tissue or lesions seen only on MRI
Surgical removal may be followed by radiation, chemotherapy, or targeted therapy, depending on the stage and subtype. Importantly, the absence of a palpable tumor does not lessen the intensity of treatment — especially in aggressive subtypes like inflammatory breast cancer.
Medical teams use multidisciplinary input — radiology, pathology, surgical oncology, medical oncology, and radiation oncology — to ensure precision. This collaborative model mirrors the approach seen in prostate cancer procedures like TULSA-PRO, where integrated imaging and procedural planning improve outcomes.
Lifestyle Modifications and Post-Treatment Monitoring
After treatment, patients with non-lump breast cancer follow similar post-therapy monitoring plans as those with conventional presentations. This typically includes:
- Regular physical exams by an oncologist every 3–6 months for the first 2 years, then less frequently
- Annual mammography (or MRI if indicated)
- Hormone therapy monitoring (if applicable)
- Blood tests or imaging if new symptoms emerge
Lifestyle changes such as reducing alcohol intake, engaging in regular physical activity, and maintaining a healthy body weight are strongly encouraged. These behaviors help reduce recurrence risk and improve overall well-being.
Survivors are also educated to be vigilant for subtle changes, even in the absence of a mass, since recurrence in the skin or lymph nodes may again appear without forming a lump. Education plays a critical role in empowering patients post-treatment.
Ongoing Research and Clinical Trials
There is increasing interest in studying breast cancers that do not present with a lump, especially rare subtypes like IBC or occult carcinoma. Clinical trials are exploring:
- New imaging methods such as contrast-enhanced mammography and molecular breast imaging
- Immunotherapies for triple-negative and HER2-positive subtypes
- AI-enhanced diagnostics for subtle mammographic and MRI changes
- Personalized vaccines and circulating tumor DNA (ctDNA) tests to detect microscopic recurrence
Patients diagnosed with these non-traditional forms of breast cancer may qualify for specialized clinical trials focused on their unique presentation. Engagement in such research may lead to earlier detection strategies and better survival outcomes in the future.
In much the same way that dense dose doxorubicin and cyclophosphamide transformed the treatment of high-risk breast cancer, future studies aim to improve care in less obvious but equally serious cases of non-lump disease.
Why Awareness of Non-Lump Breast Cancer Matters
Understanding that not all breast cancers present with a lump is crucial — both for clinicians and the general public. The signs may be subtle, misinterpreted, or attributed to benign conditions, which can lead to delayed diagnosis.
Whether it’s redness, nipple inversion, skin dimpling, or axillary swelling, these signs deserve urgent evaluation. Thanks to advancements in imaging, biopsy techniques, and systemic therapies, breast cancer can be effectively diagnosed and treated — even when a lump isn’t present.
Awareness campaigns must continue to evolve, emphasizing symptom diversity and addressing misconceptions. Patients deserve accurate, timely assessments, and clinicians must be equipped to recognize atypical presentations.
Ultimately, early action saves lives — and in breast cancer without a lump, that action begins with knowing what to look for.
Frequently Asked Questions (FAQ)
Can breast cancer really develop without a lump?
Yes, not all breast cancers begin with a noticeable lump. Certain types like inflammatory breast cancer, ductal carcinoma in situ (DCIS), or Paget’s disease may instead cause skin changes, nipple abnormalities, or swelling without forming a discrete mass.
What are early signs of breast cancer without a lump?
Early signs may include redness, skin dimpling, persistent pain, nipple discharge, inversion, or a feeling of heaviness in the breast. Swelling in the armpit or collarbone area can also be an indication of lymph node involvement even before a primary mass is felt.
How can I detect breast cancer if there’s no lump?
Imaging plays a key role. Mammography, ultrasound, and MRI can detect subtle changes like microcalcifications, architectural distortions, or skin thickening. Regular screenings, self-awareness, and reporting any unusual symptoms are essential.
Are microcalcifications a sign of cancer?
Microcalcifications are small calcium deposits visible on mammograms. While not always malignant, certain patterns — particularly tight clusters or linear distributions — may suggest early breast cancer such as DCIS and require biopsy for confirmation.
Does inflammatory breast cancer always show a lump?
No. Inflammatory breast cancer often lacks a distinct lump and instead causes redness, swelling, and skin thickening that resembles an infection. These symptoms are caused by cancer blocking lymph vessels under the skin.
Can you have breast cancer with normal mammograms?
Yes, particularly in patients with dense breast tissue. Cancers can hide behind overlapping tissue, making them difficult to detect. Supplemental imaging like ultrasound or MRI may be necessary in these cases.
What is the treatment for breast cancer without a mass?
Treatment depends on the type and stage. It may involve surgery (with localization if no mass is visible), radiation, systemic therapy (hormone therapy, chemotherapy, targeted therapy), or combinations thereof — even if no lump was ever found.
Is breast pain a sign of cancer?
Breast pain alone is rarely a sign of cancer, but persistent, localized pain that doesn’t change with the menstrual cycle should be evaluated. Pain combined with other symptoms, like skin changes, raises suspicion for non-lump cancers.
How does skin dimpling relate to cancer?
Skin dimpling can indicate underlying tumor involvement with the suspensory ligaments of the breast or lymphatic obstruction, both seen in more advanced or inflammatory forms of breast cancer, even when no lump is detected.
What is the role of nipple discharge in diagnosis?
Spontaneous, bloody, or clear discharge from one nipple may be a sign of ductal carcinoma, especially if persistent and not associated with squeezing. It warrants immediate evaluation and imaging.
Can men get breast cancer without a lump?
Yes. Though rare, male breast cancer can present with nipple retraction, skin changes, or axillary swelling instead of a lump. Any persistent breast change in men should be taken seriously and assessed medically.
How fast do non-lump cancers grow?
It depends on the subtype. Inflammatory breast cancer grows rapidly and is considered aggressive, while DCIS may develop more slowly. Absence of a lump doesn’t equate to slower progression — some are more dangerous due to late recognition.
What should I do if I notice changes but no lump?
Any new or persistent changes in breast appearance, skin, or nipple should be reported to a healthcare provider immediately, even if no lump is present. Early detection significantly improves treatment outcomes.
Can a biopsy be done if there’s no lump?
Yes. Radiologists can perform image-guided biopsies using ultrasound, mammogram, or MRI to target abnormal tissue seen on imaging. These techniques are especially important in non-palpable cancers.
How is this different from other cancers without visible symptoms?
Like medullary thyroid cancer, which can be detected through calcitonin levels and microcalcifications before a nodule forms, breast cancer without a lump requires high clinical suspicion and diagnostic precision to ensure early treatment.









