BPH vs Prostate Cancer: PSA Levels Explained
- What is PSA and Why It Matters in Prostate Screening
- How PSA Levels Behave in BPH Versus Prostate Cancer
- Typical PSA Values: Understanding the Gray Area
- Table of PSA Patterns in BPH and Prostate Cancer
- How Age Affects PSA and Risk Assessment
- PSA Velocity and Doubling Time: Indicators Beyond Numbers
- Role of Free vs Total PSA in Differentiating BPH and Cancer
- When PSA Testing Is Not Enough: Imaging and Biopsy
- How DRE Complements PSA Testing in Diagnosing Prostate Conditions
- PSA Levels After Prostate Procedures: What to Expect
- PSA and Its Limitations in Prostate Cancer Screening
- Comparative PSA Profiles in BPH vs Prostate Cancer (таблица)
- Age-Related Changes in PSA: Normal or Worrisome?
- Understanding PSA Density and Why It Matters
- PSA Doubling Time: A Clue to Malignancy Progression
- Risk Factors That Influence PSA Interpretations
What is PSA and Why It Matters in Prostate Screening
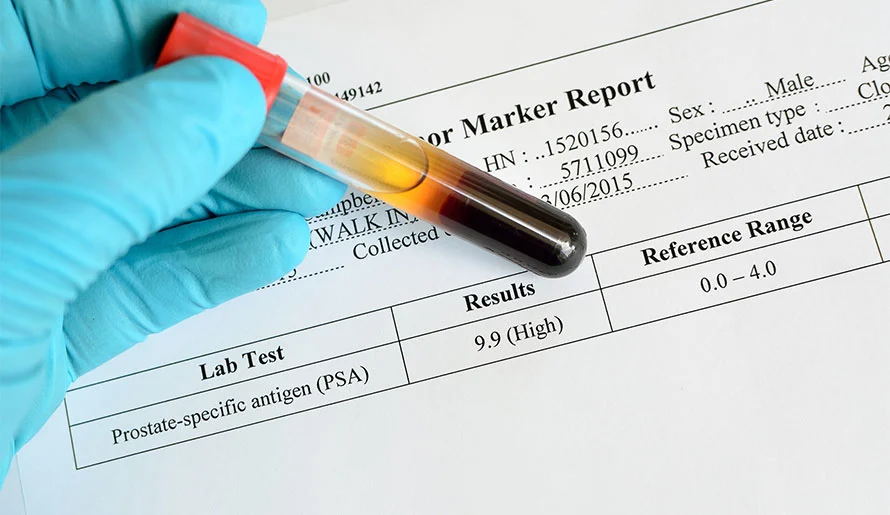
PSA, or prostate-specific antigen, is a glycoprotein produced almost exclusively by the epithelial cells of the prostate gland. Its primary biological function is to liquefy seminal fluid, aiding sperm motility. While this role is well understood in reproductive biology, the reason PSA draws attention in medicine is its leakage into the bloodstream, especially when the prostate is inflamed, enlarged, or cancerous.
When performing blood tests, physicians often monitor serum PSA levels to screen for abnormalities in the prostate. However, PSA is not a cancer-specific marker—it can be elevated in benign conditions like BPH or prostatitis. Nonetheless, it remains one of the most widely used early warning signs of possible malignancy in the prostate.
How PSA Levels Behave in BPH Versus Prostate Cancer
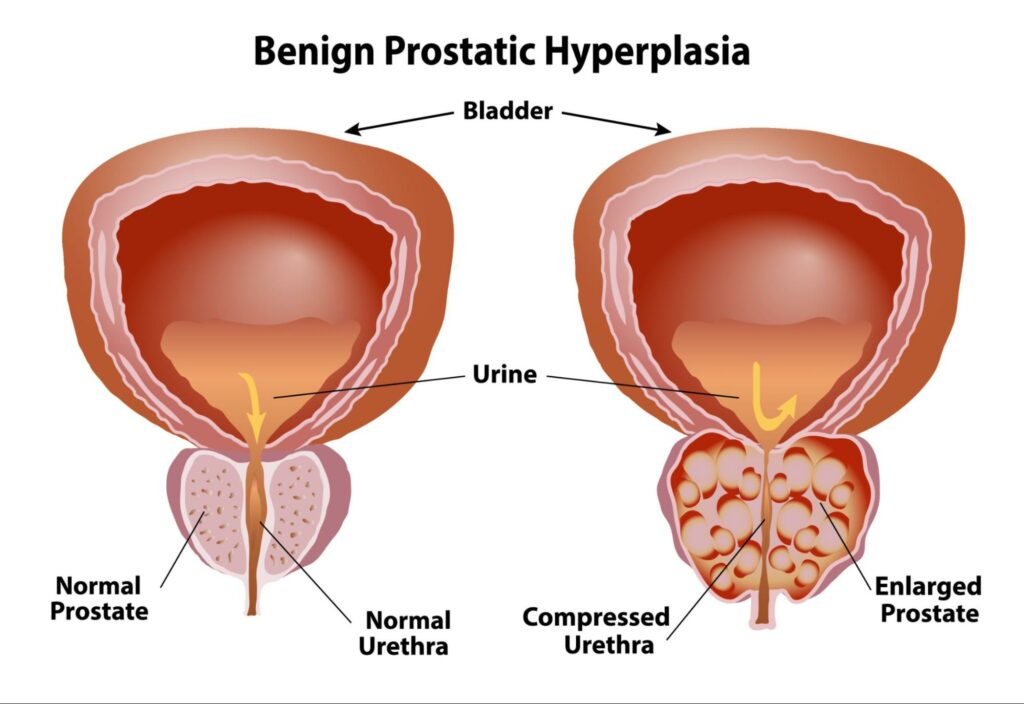
In benign prostatic hyperplasia (BPH), the prostate enlarges gradually due to aging or hormonal changes, and this increase in gland size typically causes a proportional rise in PSA levels. The PSA secreted by each benign cell remains stable, but as the number of cells increases, so does the overall PSA.
In contrast, prostate cancer often causes PSA levels to rise more sharply and unpredictably. Malignant cells tend to produce more PSA per cell than benign ones. Also, these cancerous tissues can disrupt the prostate architecture, making it easier for PSA to enter the bloodstream. Still, it’s important to note that there’s a significant overlap—someone with BPH may have a PSA of 6–8 ng/mL, similar to early-stage prostate cancer.
Typical PSA Values: Understanding the Gray Area
Most laboratories use 4.0 ng/mL as the traditional upper limit of “normal,” but this threshold is controversial. Men over 50 may naturally have higher PSA levels due to BPH, while some men with prostate cancer show only slightly elevated or even normal levels.
The gray zone, typically defined as 4.1–10 ng/mL, can indicate either condition. Physicians often use PSA density (PSA divided by prostate volume), PSA velocity (rate of increase over time), and free vs total PSA ratios to improve diagnostic precision. For example, a slow-rising PSA with a high percentage of free PSA leans more toward BPH, while rapid increases or low free PSA suggest malignancy.
Table of PSA Patterns in BPH and Prostate Cancer
| Parameter | BPH | Prostate Cancer |
| Typical PSA range | 4–10 ng/mL | 4–20+ ng/mL |
| Rate of PSA change | Slow (stable over years) | Fast (significant within months) |
| PSA density | Usually <0.15 | Often >0.15 |
| Free PSA % | Higher (>25%) | Lower (<10–15%) |
| Associated symptoms | Frequent urination, weak stream | Often asymptomatic early on |
| Digital rectal exam (DRE) | Enlarged but smooth | Firm or nodular areas |
How Age Affects PSA and Risk Assessment
Age is one of the most important contextual factors when interpreting PSA levels. As men age, the prostate typically grows in volume due to benign hyperplasia, and this naturally leads to a gradual increase in baseline PSA. Therefore, what might be considered a normal PSA for a 70-year-old could be seen as suspicious in a 45-year-old man.
Age-specific reference ranges have been proposed to reduce false positives and avoid unnecessary biopsies in older men. For instance, a PSA level of up to 2.5 ng/mL may be acceptable for a man in his 40s, while 4.5 ng/mL might be appropriate for a man in his 60s. This nuanced approach helps tailor screening to the individual rather than relying on a one-size-fits-all cutoff.
PSA Velocity and Doubling Time: Indicators Beyond Numbers
Rather than focusing solely on a single PSA value, many urologists consider the rate at which PSA rises over time. PSA velocity refers to how much the level increases per year. A velocity greater than 0.35 ng/mL/year may raise concern, particularly if the baseline PSA is already elevated.
Similarly, PSA doubling time—the period it takes for the PSA to double in value—offers prognostic insights. In prostate cancer, a rapid doubling time (less than 12 months) often suggests aggressive disease. In contrast, BPH-related PSA tends to rise slowly and may remain relatively stable over many years. Monitoring these trends helps distinguish benign changes from malignant transformation.
Role of Free vs Total PSA in Differentiating BPH and Cancer
PSA circulates in the blood in two main forms: free (unbound) and complexed (bound to proteins). In healthy prostates and BPH, a higher proportion of PSA is free. Conversely, prostate cancer tends to release more complexed PSA, lowering the ratio of free to total PSA.
A free PSA percentage above 25% typically suggests benign enlargement, while a value below 10% raises suspicion for cancer. This metric is especially useful for men with PSA values in the “gray zone” (4–10 ng/mL). The free-to-total PSA ratio helps physicians decide whether to recommend a biopsy or continue monitoring.
When PSA Testing Is Not Enough: Imaging and Biopsy
While PSA remains a frontline tool for prostate assessment, it is not definitive. Elevated levels, particularly in the 4–10 ng/mL range, do not automatically mean cancer. In such cases, further diagnostic procedures are required to clarify the picture. A digital rectal exam (DRE) is usually the next step. If abnormalities are felt, imaging or biopsy may follow.
Multiparametric MRI (mpMRI) has become an increasingly valuable tool for visualizing suspicious areas in the prostate before proceeding to biopsy. MRI-guided or fusion biopsies can then provide more accurate sampling. These approaches help reduce unnecessary biopsies in men with BPH and ensure timely detection in those with malignancies. Similarly, additional diagnostics are also crucial when symptoms overlap between unrelated conditions, as in the case of evaluating gastrointestinal discomfort in transverse colon cancer.
How DRE Complements PSA Testing in Diagnosing Prostate Conditions
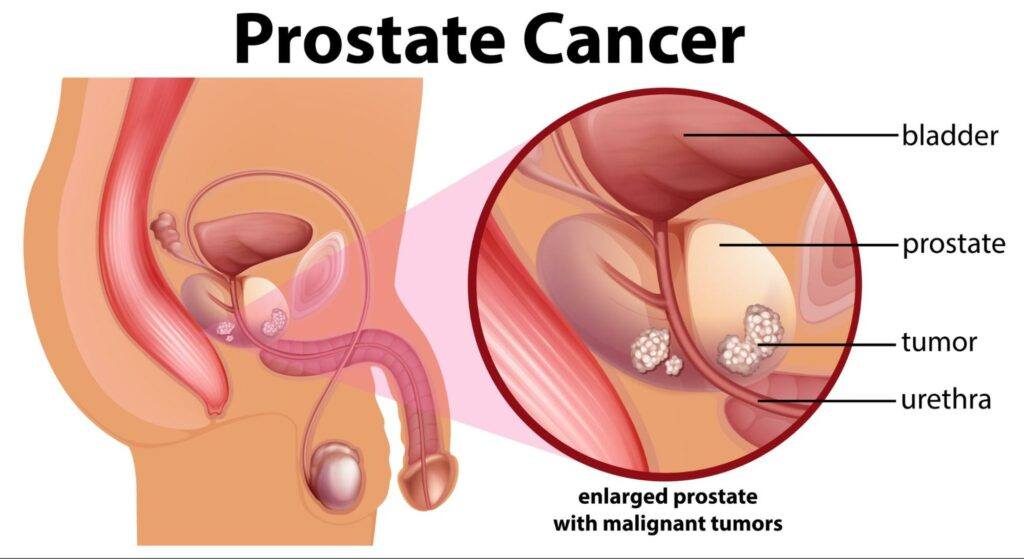
The digital rectal exam (DRE) is a crucial companion to PSA testing when evaluating prostate health. During this manual examination, the physician inserts a gloved, lubricated finger into the rectum to feel the shape, size, and consistency of the prostate. While not as sensitive as imaging, DRE offers immediate, low-cost insight into whether the gland feels enlarged, firm, nodular, or asymmetrical—features that could indicate cancer.
In BPH, the prostate is typically uniformly enlarged but soft in texture. Prostate cancer, however, may present with hard nodules or irregularities. DRE findings help guide whether further investigation, such as biopsy, is warranted. This dual approach of PSA and DRE has long been the standard protocol in urology clinics.
PSA Levels After Prostate Procedures: What to Expect
Medical or surgical interventions on the prostate—such as a transurethral resection (TURP), biopsy, or even ejaculation—can transiently elevate PSA levels. It’s important for patients to understand that PSA should not be measured shortly after such procedures, as the results may be misleading.
For example, TURP removes part of the prostate, leading to a reduced PSA baseline. Conversely, a biopsy may cause a temporary spike. Patients and doctors must wait several weeks after such events to accurately interpret PSA trends. Understanding these nuances is essential for avoiding unnecessary alarm or misdiagnosis.
PSA and Its Limitations in Prostate Cancer Screening
While PSA testing has improved early detection of prostate cancer, it’s not infallible. Elevated PSA can result from BPH, prostatitis, or even recent sexual activity. Likewise, some men with prostate cancer may have normal PSA values—particularly in the early stages or in slow-growing tumors.
This limitation has led to criticisms about overdiagnosis and overtreatment. For this reason, PSA is no longer recommended as a blanket screening tool for all men. Instead, doctors are encouraged to assess risk based on personal and family history, race, age, and other biomarkers. The test is most useful when combined with clinical judgment and other diagnostic tools. Some critics of PSA screening have drawn parallels with other debated medical interventions, such as the safety concerns that have arisen in areas like does tattoo removal cause cancer.
Comparative PSA Profiles in BPH vs Prostate Cancer (таблица)
| Characteristic | BPH | Prostate Cancer |
| PSA Level | Mild to moderately elevated | Elevated, especially >10 ng/mL |
| PSA Velocity | Slow, steady increase over years | Rapid increase over short period |
| Free PSA Ratio | Usually >25% | Often <10% |
| Doubling Time | Long (may take years) | Short (often <12 months) |
| DRE Findings | Uniform enlargement, soft texture | Nodular, firm, or irregular |
| Response to Finasteride | PSA reduced by ~50% | Limited or no effect on PSA |
| Post-Treatment PSA Drop | Less relevant, not monitored closely | Used to assess recurrence or response |
This comparison helps both patients and providers discern which direction further testing should take. Similarly, molecular pathways can help differentiate conditions, such as in the role of What is PTP1B in breast cancer when assessing cell signaling in tumors.
Age-Related Changes in PSA: Normal or Worrisome?
PSA levels naturally increase with age due to the gradual enlargement of the prostate, a common feature of benign prostatic hyperplasia (BPH). For men in their 40s, a PSA above 2.5 ng/mL may raise concern, while in men over 70, levels up to 6.5 ng/mL may still be considered within a benign range. However, this age-adjusted interpretation often creates confusion among patients.
The key lies in tracking PSA changes over time, not just relying on a single result. A stable PSA that rises slightly over the years is usually consistent with BPH, whereas a sudden jump over a few months can be a red flag for malignancy. Physicians now increasingly use age-specific PSA reference ranges to improve diagnostic accuracy and reduce unnecessary biopsies.
Understanding PSA Density and Why It Matters
PSA density refers to the PSA level in relation to the volume of the prostate, typically measured via transrectal ultrasound or MRI. This parameter is calculated by dividing the total PSA by the prostate volume. In men with BPH, the PSA density is usually low because the gland is large but not cancerous.
A high PSA density—above 0.15 ng/mL/cm³—is more suggestive of prostate cancer. This measurement adds depth to PSA interpretation, especially in patients with borderline PSA levels. It helps distinguish between a large benign prostate secreting more PSA and a smaller prostate possibly harboring cancer. Urologists often rely on PSA density to decide whether a biopsy is necessary, especially in patients with a negative DRE.
PSA Doubling Time: A Clue to Malignancy Progression
One of the most valuable metrics in prostate cancer surveillance is PSA doubling time—the time it takes for PSA levels to double. A slow doubling time of more than 2 years usually suggests a benign condition or indolent cancer. In contrast, a rapid doubling time of under 12 months is highly associated with aggressive cancer.
This parameter becomes especially important after initial diagnosis or treatment. In active surveillance protocols, a shift in doubling time may prompt a change in management. Even in BPH, PSA can increase, but typically over a much longer timespan. The consistency of monitoring is vital for recognizing harmful trends early.
Risk Factors That Influence PSA Interpretations
Interpreting PSA results is not done in isolation. Several personal and environmental risk factors can affect PSA levels and how they’re understood. These include age, ethnicity (e.g., higher baseline PSA in African American men), family history of prostate cancer, smoking status, and even certain infections or medications.
For instance, men with a strong family history of prostate cancer might require more aggressive monitoring even if their PSA appears within the acceptable range. Similarly, medications like finasteride or dutasteride, used to treat BPH, can halve PSA levels—meaning the value must be doubled for accurate interpretation. Understanding such individualized risk factors is just as critical as recognizing possible triggers in unrelated cancers, like in parasitic infections potentially linked to do parasites cause breast cancer.
FAQ
What is the normal range for PSA levels in men?
For most men, a PSA level under 4.0 ng/mL is considered within the normal range, though this varies based on age and prostate size. Some younger men may have lower thresholds, while older men can have slightly higher levels without indicating cancer. That said, PSA must always be interpreted alongside other clinical findings because some men with low PSA can still have prostate cancer.
Can BPH cause PSA levels to rise significantly?
Yes, benign prostatic hyperplasia (BPH) can cause a measurable increase in PSA levels due to the enlarged volume of the prostate tissue producing more of the antigen. However, the rise is usually gradual and stable over time, not exceeding 0.75 ng/mL per year. Sudden or sharp increases warrant further testing to rule out malignancy.
How can doctors tell if high PSA is from BPH or cancer?
Doctors use several tools to differentiate the cause, including PSA velocity, PSA density, digital rectal exam (DRE), and imaging like multiparametric MRI. A prostate biopsy may be ordered if these assessments suggest cancer risk. Ultimately, the pattern of PSA change and correlation with imaging is what helps distinguish the source.
Is PSA testing reliable for diagnosing prostate cancer?
PSA testing is a useful screening tool, but it’s not definitive for diagnosis. It must be used with physical exams and imaging to determine whether further steps like a biopsy are necessary. Some men with prostate cancer have normal PSA, and others with high PSA do not have cancer.
Does a high PSA level mean I have cancer?
Not necessarily. PSA can rise due to various factors including BPH, infection (prostatitis), recent ejaculation, or even a prostate exam. While high PSA can signal cancer, it is not conclusive without additional evidence. A thorough evaluation is required to make an accurate diagnosis.
What is PSA density, and why does it matter?
PSA density is calculated by dividing the PSA level by the volume of the prostate. A high PSA density (typically above 0.15 ng/mL/cm³) raises concern for prostate cancer, especially when the prostate is not significantly enlarged. It helps add context to raw PSA numbers.
Can PSA velocity predict prostate cancer?
Yes, PSA velocity—how fast PSA levels rise over time—is a useful indicator. An increase greater than 0.75 ng/mL per year is often a red flag for cancer, particularly if sustained over multiple tests. It provides insight into the biological activity of the prostate.
How often should PSA levels be checked?
For men undergoing screening or monitoring, PSA is typically checked annually. In high-risk cases or those under active surveillance, tests may be done every 6 months. The frequency depends on personal risk factors, age, and previous PSA trends.
Does prostate size affect PSA levels?
Yes. Larger prostates produce more PSA, which is why men with BPH often have elevated levels despite being cancer-free. Imaging like ultrasound or MRI is often used to assess prostate volume and correlate with PSA.
Are there lifestyle factors that influence PSA levels?
Yes, factors like recent sexual activity, bike riding, or certain medications (like 5-alpha-reductase inhibitors) can affect PSA levels. Infections or inflammation can also cause temporary spikes. These should be considered when interpreting test results.
Is a prostate biopsy always needed if PSA is high?
Not always. If other indicators (like DRE or imaging) are normal and PSA is only mildly elevated, doctors may opt for watchful waiting or repeat testing. Biopsy is typically recommended when multiple markers raise concern for malignancy.
Can prostate cancer and BPH coexist?
Yes, it’s common for older men to have both conditions simultaneously. BPH causes urinary symptoms, while prostate cancer may remain asymptomatic. That’s why thorough evaluation is necessary even if symptoms seem benign.
How is PSA interpreted after age 70?
In older men, higher PSA levels can be more acceptable due to natural prostate enlargement. However, persistent increases or abnormal imaging findings still require attention. The benefit-risk balance of aggressive testing changes with age.
Is there a link between inflammation and PSA levels?
Yes, prostatitis or general inflammation can temporarily elevate PSA. This elevation is typically reversible after treatment. It’s essential to rule out infection before jumping to conclusions about cancer risk.
How does PSA testing fit into cancer screening guidelines?
Most guidelines recommend PSA screening after age 50, or earlier for high-risk men (e.g., African-American descent or family history). The decision to screen should be personalized based on the man’s values, life expectancy, and risk profile.












