Bile Duct Cancer ICD-10: Accurate Classification and Clinical Guidance
- What Is Bile Duct Cancer and Why Coding Accuracy Matters
- ICD-10 Code Overview for Bile Duct Cancer
- Differentiating Between Intrahepatic and Extrahepatic Cholangiocarcinoma
- Role of Histological Confirmation in ICD-10 Assignment
- Coding for Ampullary Carcinoma: Distinct Entity in ICD-10
- Understanding Overlapping and Unspecified Codes: C24.8 and C24.9
- Incorporating Z-Codes for Treatment Follow-Up and History
- ICD-10 Coding and Surgical Procedures: Matching CPT and ICD
- Role of Radiologic Imaging in ICD-10 Code Accuracy
- When and How to Code for Metastasis in Bile Duct Cancer
- Coding in the Context of Liver Transplant and Palliative Procedures
- Importance of Multidisciplinary Documentation in Rare Biliary Tumors
- ICD-10 Coding in Pediatric Versus Adult Bile Duct Tumors
- Table of Common ICD-10 Codes for Bile Duct Cancer and Related Conditions
- Common Coding Pitfalls and How to Avoid Them
- Future Directions in ICD Coding for Biliary Malignancies
- Frequently Asked Questions (FAQ)
What Is Bile Duct Cancer and Why Coding Accuracy Matters
Bile duct cancer, also known as cholangiocarcinoma, is a rare but aggressive malignancy that originates in the bile ducts, which transport bile from the liver and gallbladder to the small intestine. It is classified into intrahepatic (within the liver), perihilar (at the junction of right and left ducts), and distal (closer to the small intestine) types. Early diagnosis is often difficult because symptoms such as jaundice, itching, and abdominal discomfort usually appear at advanced stages.
Precise coding using the ICD-10 system is critical in documenting the type and location of bile duct cancers. This accuracy ensures effective communication between clinicians, improves data for cancer registries, supports correct reimbursement, and allows researchers to track disease patterns.
ICD-10 Code Overview for Bile Duct Cancer
In ICD-10-CM, bile duct cancers are primarily classified under C24 – Malignant neoplasm of other and unspecified parts of biliary tract. This category is subdivided to reflect anatomical regions of the bile duct. For example:
- C24.0 – Malignant neoplasm of extrahepatic bile duct
- C24.1 – Malignant neoplasm of ampulla of Vater
- C24.8 – Overlapping lesion of biliary tract
- C24.9 – Malignant neoplasm of biliary tract, unspecified
Using the correct code ensures that both clinical records and insurance claims are properly aligned. A lack of anatomical specificity—such as using C24.9 when C24.0 is more accurate—can lead to administrative delays and inaccurate clinical data.
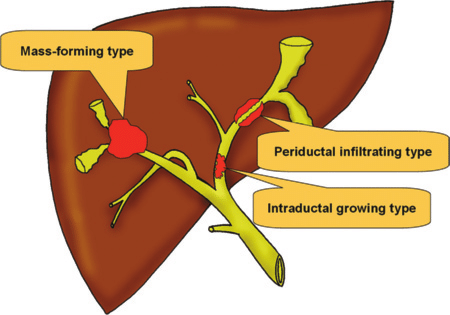
Differentiating Between Intrahepatic and Extrahepatic Cholangiocarcinoma
Intrahepatic bile duct cancers, although arising in the bile ducts, are coded separately under C22.1 (intrahepatic bile duct carcinoma) rather than within the C24 family. This distinction is essential, as these two entities differ in terms of surgical management, prognosis, and staging systems. While C24 codes refer to tumors outside the liver, C22.1 captures those starting in the intrahepatic biliary tree.
This is somewhat similar to the need for precise classification in skin cancer documentation, such as distinguishing between basal cell carcinoma of the eyelid versus an unspecified skin site.
Understanding this coding split helps avoid common clinical mistakes, where intrahepatic lesions may be incorrectly grouped with C24.0 codes. Proper documentation of imaging, biopsy, and pathology is key.
Role of Histological Confirmation in ICD-10 Assignment
Accurate coding of bile duct cancer relies not only on the tumor’s location but also on histological confirmation. Without biopsy-proven evidence, assigning a malignant ICD-10 code may be premature. For suspected lesions without pathology, Z-codes such as Z03.89 (encounter for observation for other suspected diseases) may be used.
Once confirmed, the histology can further guide treatment and coding. For example, adenocarcinoma is the most common subtype of cholangiocarcinoma and can be noted in clinical documentation to support the use of a C24 code. If a tumor exhibits rare histological patterns, like squamous or neuroendocrine features, coders must consult additional pathology documentation.
This reflects the same challenges seen in less common cancers like Bartholin gland cancer, where proper coding also depends on histological confirmation and anatomical precision.
Coding for Ampullary Carcinoma: Distinct Entity in ICD-10
Ampullary carcinoma is a distinct type of cancer originating from the ampulla of Vater, the region where the bile duct and pancreatic duct merge and empty into the duodenum. While technically not a bile duct tumor, it is classified under the biliary system in ICD-10 as C24.1 – Malignant neoplasm of ampulla of Vater.
This separation is important because ampullary carcinoma presents differently from extrahepatic bile duct tumors, often causing earlier symptoms like jaundice, which leads to faster diagnosis. The treatment, prognosis, and surgical approach also differ significantly. Therefore, coders must carefully review radiology and pathology reports to differentiate true bile duct cholangiocarcinoma from ampullary origin.
Clinical notes that lack this detail may result in improper classification under C24.0 or C24.9, which could impact not only reimbursement but also the accuracy of cancer registries and national statistics.
Understanding Overlapping and Unspecified Codes: C24.8 and C24.9
When a bile duct tumor affects more than one contiguous area of the biliary tract (e.g., both the common bile duct and the ampulla), ICD-10 provides C24.8 – Overlapping lesion of biliary tract. This code captures tumors that cross anatomic boundaries and cannot be assigned to a single specific site.
In contrast, C24.9 – Malignant neoplasm of biliary tract, unspecified should only be used when the origin of the cancer cannot be determined, such as in poor-quality or incomplete documentation. While C24.9 is technically valid, its use should be minimized, especially when imaging or biopsy data provide more precise anatomical detail.
The distinction is akin to challenges found in dermatologic coding, such as between basal cell skin cancer with precise localization and one classified as “unspecified.” Basal cell skin cancer icd 10 – in the context of specificity versus non-specificity of codes.
By default, clinicians should be encouraged to clearly document all known anatomical sites involved in the tumor process.
Incorporating Z-Codes for Treatment Follow-Up and History
In patients with a previous diagnosis of bile duct cancer, or those undergoing post-treatment surveillance, ICD-10 allows for the use of Z-codes to indicate non-active cancer status or monitoring protocols. Commonly used Z-codes include:
- Z85.818 – Personal history of malignant neoplasm of other digestive organs
- Z08 – Follow-up examination after completed treatment for malignant neoplasm
- Z09 – Follow-up after treatment for conditions other than cancer
These codes are never used as primary diagnoses but help paint a more complete clinical picture. They also serve as critical indicators in oncology databases that monitor recurrence patterns and survivorship trends.
Failing to use these codes may result in confusion regarding the patient’s treatment status, especially in long-term follow-up.
ICD-10 Coding and Surgical Procedures: Matching CPT and ICD
While ICD-10 codes document diagnoses, the actual procedures performed—such as biliary resections, Whipple procedures, or palliative bypasses—are coded using CPT (Current Procedural Terminology) or ICD-10-PCS codes in inpatient settings.
A correct diagnosis code (e.g., C24.0 for distal bile duct cancer) must correspond with the surgical procedure being reported. For example, if a Whipple procedure (pancreaticoduodenectomy) is performed for a cancer coded as ampullary (C24.1), it must align with operative and pathology findings.
Mismatches between ICD-10 and CPT/PCS codes can lead to insurance denials, delays in reimbursement, or coding audits. Coders and clinicians must work together to ensure that:
- Preoperative imaging confirms the tumor location
- Operative notes are detailed
- Histological confirmation supports diagnosis
This coding dynamic is especially important in large cancer centers, where multidisciplinary teams may interpret anatomy and pathology differently if documentation is ambiguous.
Role of Radiologic Imaging in ICD-10 Code Accuracy
Radiologic imaging, particularly MRCP (Magnetic Resonance Cholangiopancreatography), CT scans, and endoscopic ultrasound, plays a pivotal role in identifying the exact location and extent of bile duct tumors. Accurate imaging reports can clarify whether the lesion is intrahepatic (C22.1), extrahepatic (C24.0), ampullary (C24.1), or overlapping (C24.8).
Coders often rely on imaging results when pathology is pending or incomplete. For example, if an MRI clearly states “mass at the distal common bile duct,” coders can confidently assign C24.0 instead of defaulting to C24.9, which lacks site specificity.
However, imaging alone is insufficient without clear documentation in the clinician’s progress notes or surgical report. Radiologists should describe tumor boundaries using anatomical terms consistent with ICD-10 categories to streamline the coding workflow.
When and How to Code for Metastasis in Bile Duct Cancer
Bile duct cancer, particularly at advanced stages, frequently metastasizes to the liver, peritoneum, lungs, or lymph nodes. ICD-10 allows these secondary sites to be coded with C78–C79 categories, such as:
- C78.7 – Secondary malignant neoplasm of liver
- C77.0 – Secondary and unspecified malignant neoplasm of lymph nodes of head, face and neck (for perihilar spread)
- C79.5 – Secondary malignant neoplasm of bone and bone marrow
These codes should be used in addition to the primary code (e.g., C24.0) to fully represent the patient’s oncologic status. Coders must review oncologist notes and imaging to confirm metastatic spread before assigning secondary cancer codes.
Failure to include secondary site codes underreports disease severity and can lead to under-treatment, clinical miscommunication, or missed eligibility for advanced therapies like targeted biologics or immunotherapy.
Coding in the Context of Liver Transplant and Palliative Procedures
In selected patients with localized or borderline resectable bile duct cancer, liver transplantation may be considered, especially in centers with aggressive protocols. In such cases, coding requires clear indication of the primary malignancy (e.g., C24.0) alongside procedural codes for transplant surgery.
In contrast, many patients—particularly those with metastatic or advanced cholangiocarcinoma—undergo palliative interventions, such as:
- Biliary stenting (via ERCP)
- Percutaneous biliary drainage
- Gastrojejunostomy bypass
These do not cure the cancer but relieve obstructive symptoms. Coding in such cases must reflect both the underlying malignancy and the palliative nature of treatment, using Z-codes such as Z51.5 (palliative care) or procedure-specific ICD-10-PCS codes.
Such coding precision mirrors other cases of supportive treatment in cancer, including non-curative excisions or drainage procedures seen in rare tumors like Bartholin gland carcinoma. bartholin cyst cancer – as an analogue in the choice between radical and palliative approaches.
Importance of Multidisciplinary Documentation in Rare Biliary Tumors
Given its complexity and rarity, bile duct cancer is almost always managed by multidisciplinary teams, including hepatobiliary surgeons, gastroenterologists, oncologists, pathologists, and radiologists. From a coding perspective, each specialty must document findings with sufficient clarity to support the correct ICD-10 code.
Pathology must confirm malignancy and specify margins and histology; radiology must map tumor boundaries and nodes; surgeons must describe intraoperative anatomy in relation to bile duct segments. All of this data allows coders to choose among:
- C22.1 (intrahepatic)
- C24.0 (extrahepatic)
- C24.1 (ampullary)
- C24.8 (overlapping)
- C24.9 (unspecified)
This collaborative model also enhances patient care, guiding decisions about resection margins, neoadjuvant therapy, or palliative strategy. Without such coordination, coding errors become more likely, delaying treatment and misrepresenting disease in registries and insurance documentation.
ICD-10 Coding in Pediatric Versus Adult Bile Duct Tumors
Bile duct cancers are exceedingly rare in the pediatric population but may occur as part of congenital or genetic syndromes, such as Caroli disease, biliary atresia, or in association with primary sclerosing cholangitis. When encountered, coding must reflect both the malignancy and the underlying predisposition.
In such cases, ICD-10 allows the use of additional Q-codes (for congenital conditions), or Z-codes for genetic screening and monitoring. In contrast, adult bile duct cancers—especially in those over 50—are typically sporadic and associated with risk factors like liver fluke infections, chronic inflammation, or cirrhosis.
Documenting age-related differences is critical, as it influences treatment pathways, screening protocols, and the interpretation of clinical data in registries and insurance databases.
Table of Common ICD-10 Codes for Bile Duct Cancer and Related Conditions
| ICD-10 Code | Description |
| C22.1 | Intrahepatic bile duct carcinoma |
| C24.0 | Malignant neoplasm of extrahepatic bile duct |
| C24.1 | Malignant neoplasm of ampulla of Vater |
| C24.8 | Overlapping lesion of biliary tract |
| C24.9 | Malignant neoplasm of biliary tract, unspecified |
| C78.7 | Secondary malignant neoplasm of liver |
| C77.0 | Secondary malignant neoplasm of lymph nodes (head/neck) |
| C79.5 | Secondary malignant neoplasm of bone and bone marrow |
| Z85.818 | Personal history of malignant neoplasm of other digestive organs |
| Z51.5 | Encounter for palliative care |
This reference aids both clinicians and coders in quickly selecting accurate codes based on clinical findings and anatomical context. It also helps ensure billing and documentation consistency across healthcare systems.
Common Coding Pitfalls and How to Avoid Them
Even experienced coders can make errors when assigning ICD-10 codes for bile duct cancer, particularly when documentation is vague or incomplete. Among the most common mistakes:
- Using C24.9 (unspecified site) when specific imaging or biopsy data exist
- Failing to code metastatic sites
- Omitting relevant Z-codes for follow-up, history, or palliative care
- Misclassifying intrahepatic tumors under extrahepatic categories
Avoiding these pitfalls requires a collaborative effort between physicians, coders, and administrative staff. Coders should not hesitate to query providers when documentation lacks sufficient detail to support a definitive code.
Routine audits and coder education sessions focused on complex gastrointestinal malignancies can dramatically reduce documentation errors and support better clinical outcomes.
Future Directions in ICD Coding for Biliary Malignancies
As medicine advances, ICD systems are evolving to include more granularity, especially in oncology. For bile duct cancers, future updates may reflect:
- Genomic classifiers (e.g., FGFR2 mutations)
- Immunotherapy markers
- Detailed anatomic staging (e.g., perihilar vs. distal cholangiocarcinoma)
- Specific coding for recurrence and residual disease
Such refinements are necessary to support precision oncology, clinical trials, and outcome-based reimbursement models. The integration of artificial intelligence, natural language processing, and electronic health records will likely streamline this coding process in the years ahead.
This mirrors trends seen in other cancers, such as skin cancer, where molecular markers and histological variants are beginning to influence classification and code structure. Basal cell skin cancer icd 10 – as an example of the dynamics of codes in oncology.
Frequently Asked Questions (FAQ)
What is the ICD-10 code for bile duct cancer?
The general ICD-10 code for extrahepatic bile duct cancer is C24.0. Other options include C22.1 for intrahepatic, C24.1 for ampullary, C24.8 for overlapping sites, and C24.9 for unspecified bile duct cancer. Choosing the right code depends on precise anatomical and pathological documentation.
How is intrahepatic bile duct cancer coded?
Intrahepatic bile duct cancer is classified under C22.1, as it is technically a subtype of liver cancer. This differs from extrahepatic bile duct tumors, which fall under the C24 category.
Is C24.9 an acceptable code to use?
Yes, but it should be used cautiously. C24.9 should only be applied when the specific location of the bile duct tumor cannot be determined, often due to incomplete imaging or documentation. Otherwise, site-specific codes are preferred.
What is the code for ampullary carcinoma?
The appropriate ICD-10 code for cancer of the ampulla of Vater is C24.1. This is distinct from other biliary tumors and should be clearly documented in imaging and surgical reports.
Can metastasis be coded separately from the primary bile duct tumor?
Yes. Metastatic sites, such as the liver (C78.7) or bone (C79.5), should be coded in addition to the primary code to represent the full extent of disease.
What Z-codes are useful in bile duct cancer cases?
Z-codes such as Z85.818 (history of digestive organ cancer), Z08 (follow-up after treatment), and Z51.5 (palliative care) provide important clinical context and should be used alongside C24 codes when applicable.
How should bile duct cancer with multiple sites be coded?
Use C24.8 – Overlapping lesion of biliary tract when the tumor involves multiple contiguous areas, such as the common bile duct and ampulla. This avoids ambiguity and improves registry accuracy.
What is the difference between C24.0 and C24.8?
C24.0 applies to extrahepatic bile duct cancers confined to a single location, while C24.8 is used when the tumor overlaps multiple contiguous parts of the biliary tract.
Are pediatric cases of bile duct cancer coded differently?
While the base code remains the same, pediatric cases may require additional codes for underlying congenital conditions or syndromes, such as Q-codes for biliary anomalies or Z-codes for genetic screening.Do I need pathology confirmation to code C24?
Do I need pathology confirmation to code C24?
Ideally, yes. While imaging and clinical suspicion can be documented, a biopsy confirmation is necessary before assigning a definitive malignant neoplasm code. Otherwise, observational Z-codes may be more appropriate.
Can palliative procedures like stenting be coded with bile duct cancer?
Yes, procedural codes (CPT or PCS) should be used to reflect interventions, and Z51.5 can accompany the C24 diagnosis to indicate palliative care.
Is liver transplant included in bile duct cancer coding?
If performed for bile duct cancer, the diagnosis code (e.g., C24.0) should be paired with a procedural transplant code. Transplant is rare but relevant in selected cases of localized perihilar cholangiocarcinoma.
What happens if imaging shows bile duct mass but location is unclear?
In such cases, coders may temporarily use C24.9, but should query the provider or wait for clarification through follow-up imaging or biopsy to allow more specific classification.
How does bile duct cancer coding differ from other GI cancers?
Bile duct cancers have unique anatomical classifications and distinct codes from liver, pancreatic, or gallbladder cancers. Accurate site documentation is critical to avoid misclassification.
Can ICD-10 coding for bile duct cancer affect treatment options?
Yes. Accurate coding ensures proper authorization for targeted therapies, surgeries, and advanced imaging. It also supports inclusion in registries and access to clinical trials, where site-specific data is often a requirement.












