Best Sleeping Position for Lower Back Pain: Expert Advice for Pain-Free Rest
- Understanding Lower Back Pain: Why It Gets Worse at Night
- Common Symptoms of Lower Back Pain That Interfere with Sleep
- Stages of Lower Back Pain: From Acute to Chronic
- Why Sleep Position Matters for Lumbar Health
- Sleeping on Your Back: How to Do It Safely
- Side Sleeping: Pros, Pitfalls, and Positioning Tweaks
- Is Fetal Position Safe for Your Back?
- Sleeping on Your Stomach: Why It Often Makes Pain Worse
- Mattress Matters: Finding the Right Firmness for Your Spine
- Pillow Placement and Height: Crucial Yet Overlooked
- Comparing Sleep Positions for Lower Back Pain Relief
- How Stress and Sleep Posture Interact
- Morning Routine to Counteract Nighttime Stiffness
- How Lifestyle and Daily Habits Affect Sleep and Back Health
- When to Consult a Specialist for Persistent Back Pain
- Building a Sustainable, Personalized Sleep Strategy
- FAQ

Understanding Lower Back Pain: Why It Gets Worse at Night
Lower back pain is one of the most common musculoskeletal complaints worldwide. While daytime activities like sitting or lifting often get blamed, many people experience worsening symptoms at night—or even feel the pain most acutely while trying to sleep or upon waking. That’s because when the body is at rest, gravity and poor sleep posture can exert unrelieved pressure on the lumbar spine and surrounding muscles.
When you lie down, the natural curve of your spine can become exaggerated or flattened, depending on your position and mattress quality. If your spine isn’t properly aligned, the soft tissues around the lower back—ligaments, discs, and muscles—remain strained throughout the night, resulting in stiffness and pain the next morning.
Other nighttime triggers include tight hip flexors, weak core muscles, and inflammation that settles in joints when you’re still. Understanding the biomechanics of sleep positions is essential to not only relieve pain, but also support spinal healing over time.
Common Symptoms of Lower Back Pain That Interfere with Sleep
Lower back pain can manifest in different ways depending on the cause, but several symptoms frequently disrupt sleep. Many people report a dull, aching pain in the lower spine that worsens in certain positions, especially when lying flat on the back or stomach. Others feel radiating pain or numbness into the hips, glutes, or legs—often from nerve irritation like sciatica.
Tossing and turning is another frequent complaint, as discomfort prevents people from settling into one position. Some individuals experience sharp, stabbing sensations when transitioning from side to back, while others feel deep morning stiffness due to inflammation or tight fascia.
This kind of pain can also lead to poor sleep quality, which contributes to a vicious cycle: the less restorative your sleep, the less your tissues can heal, and the more tension accumulates throughout the day.
Stages of Lower Back Pain: From Acute to Chronic
Back pain doesn’t follow a single pattern—it evolves depending on how it’s managed. In the acute stage, pain appears suddenly, often from lifting, twisting, or long hours in poor posture. At this point, inflammation is dominant, and rest combined with gentle care can often resolve the problem in days or weeks.
If pain persists beyond six weeks, it may be considered subacute or recurrent. This stage is marked by lingering stiffness, muscle imbalances, or unresolved inflammation. Many people in this phase begin modifying their movements to avoid pain, which can cause new imbalances.
Chronic back pain (lasting more than 12 weeks) often involves both physical and psychological factors. Pain may become less intense but more persistent, influenced by sleep disruption, nervous system sensitivity, and poor postural habits. Understanding your stage is key—chronic cases often require a combination of biomechanical correction, lifestyle changes, and nervous system regulation similar to those used in natural anxiety management.

Why Sleep Position Matters for Lumbar Health
Your spine is designed to maintain a gentle S-curve, and sleep posture plays a critical role in preserving that alignment during rest. When that curve is flattened or exaggerated, pressure builds in the lumbar discs, facet joints, and paraspinal muscles—leading to inflammation, microtrauma, and tension.
Sleeping on your stomach, for example, forces your lower back into hyperextension while twisting the neck and shoulders, making it the most problematic position for low back pain. Conversely, lying flat on the back with no support under the knees can also cause the lumbar spine to arch excessively.
The best positions are those that maintain neutral alignment, reducing unnecessary strain. But ideal positioning doesn’t stop with sleep—it includes pillow placement, mattress support, and nighttime movement patterns. Just as targeted routines help with foot conditions like plantar fasciitis, a sleep strategy must be proactive, not passive, to truly improve spinal comfort overnight.
Sleeping on Your Back: How to Do It Safely
Sleeping on your back can be one of the best positions for lower back pain—if done correctly. This posture naturally distributes body weight and avoids unnatural twisting of the spine. However, many people who sleep flat on their back experience increased pain if the lumbar curve is unsupported.
The key to back sleeping is placing a pillow under the knees. This small adjustment flattens the lower spine slightly and reduces tension in the hip flexors and lumbar extensors. Some individuals benefit from adding a rolled towel under the lower back to fill the natural curve, depending on spinal shape and mattress firmness.
A medium-firm to firm mattress typically works best for back sleepers with low back pain. Soft beds may allow the hips to sink too deeply, increasing arching in the lumbar area. If you already sleep on your back but wake up sore, it’s likely due to poor alignment, not the position itself.
Side Sleeping: Pros, Pitfalls, and Positioning Tweaks
Sleeping on your side is often recommended for people with back pain, especially when combined with proper support. When done well, it keeps the spine neutral and relieves pressure from the back, hips, and shoulders. But done poorly, it can lead to spinal rotation, pelvic imbalance, and worsening pain.
The ideal side-sleeping posture includes placing a pillow between the knees to keep the hips level. Without this support, the top leg may fall forward, causing the spine to twist and the lower back to strain. Some people also benefit from hugging a body pillow to prevent shoulder rounding and provide emotional comfort.
Side sleeping on the left side is often preferable, as it may also improve digestion and reduce acid reflux. However, switching sides throughout the night can prevent muscle imbalances. As with all positions, the mattress must support the shoulders and hips without collapsing or overextending the curves.
Is Fetal Position Safe for Your Back?
The fetal position—curled on your side with knees drawn toward the chest—is a common choice for people with back discomfort, and in many cases, it provides genuine relief. This posture gently opens the spinal joints, relieves nerve pressure (especially in sciatica), and reduces lumbar muscle tension. It can be especially helpful during acute pain phases when movement is limited.
However, curling too tightly can round the upper back and overstretch the neck, leading to discomfort elsewhere. The trick is to soften the curl and support key points: place a pillow between the knees and under the head to maintain alignment. Keep shoulders relaxed and avoid crossing arms tightly, which can strain the upper spine.
The fetal position is especially beneficial for those recovering from disc-related injuries or who experience increased pain when lying flat. It shares some alignment principles with protective postures used in early-stage plantar fasciitis recovery: minimal strain, maximum support.
Sleeping on Your Stomach: Why It Often Makes Pain Worse
Of all sleeping positions, lying face-down is the most problematic for lower back pain. It causes the lumbar spine to hyperextend, compressing facet joints and placing extra stress on the pelvis. To make matters worse, the neck is twisted to the side, disrupting alignment from the skull to the sacrum.
That said, some people find stomach sleeping comforting due to habit or emotional reasons. If switching to another position is too difficult, modifying the posture can reduce harm. Placing a thin pillow under the lower abdomen can help reduce lumbar arching, and using a very flat or no pillow under the head keeps the neck more aligned.
Ultimately, the goal is to gradually transition to a more neutral position. This may involve side sleeping with a body pillow, or temporarily resting in a semi-prone posture that provides similar sensory comfort without the same structural strain. Just like in natural anxiety reduction strategies, small shifts made consistently over time lead to lasting change.
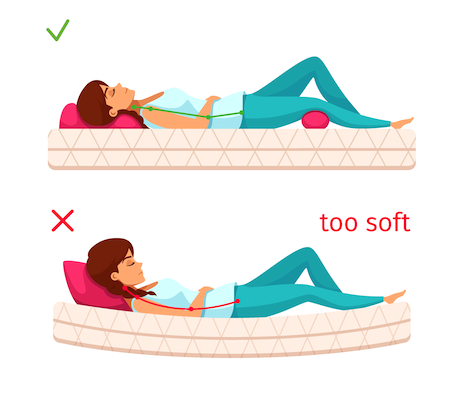
Mattress Matters: Finding the Right Firmness for Your Spine
Your mattress can make or break your back—especially during the 6 to 8 hours your body spends lying on it each night. A mattress that’s too soft can allow the hips to sink, throwing off spinal alignment and overextending the lower back. On the other hand, a mattress that’s too firm may force the spine into unnatural pressure points and increase stiffness by morning.
Most people with lower back pain do best on a medium-firm mattress that cushions the hips and shoulders but supports the lumbar curve. Memory foam and hybrid models tend to offer the best combination of support and contouring, especially when paired with proper pillow support.
What’s often overlooked is how a mattress interacts with your body shape and preferred sleeping position. For instance, side sleepers may need more pressure relief, while back sleepers require firmer support under the lumbar spine. Don’t be afraid to test different surfaces—many companies now offer sleep trials. A good mattress is not just about comfort; it’s a long-term investment in spinal health and pain prevention.
Pillow Placement and Height: Crucial Yet Overlooked
While mattresses support the whole body, pillows fine-tune alignment, especially for the cervical and lumbar spine. A pillow that’s too high or too flat can misalign the neck, creating compensatory strain in the lower back. This tension often travels down the spine, disrupting sleep and reinforcing tightness by morning.
For side sleepers, a thick pillow that fills the space between the head and shoulder keeps the neck neutral. For back sleepers, a medium pillow that supports the natural curve of the neck works best. If your chin is tilted up or your head drops too far back, your pillow may be the culprit.
Importantly, lower back pain often improves when a pillow is placed under the knees (back sleepers) or between the knees (side sleepers). This relieves pressure from the pelvis and sacrum, which often bear the brunt of tension during the night. The positioning concept is similar to support techniques used in the home treatment of plantar fasciitis, where elevation and padding protect stressed tissues.

Comparing Sleep Positions for Lower Back Pain Relief
To help visualize which sleeping positions best support spinal health, here’s a comparative overview:
| Position | Pros | Cons | Support Tips |
| Back Sleeping | Promotes even weight distribution and spinal alignment | May worsen arch if legs not supported | Use pillow under knees; firm mattress |
| Side Sleeping | Relieves pressure from discs and soft tissue | Risk of hip and spine rotation | Pillow between knees; switch sides during night |
| Fetal Position | Eases nerve compression, calms tension | Can over-round shoulders or neck | Use body pillow; keep curl gentle |
| Stomach Sleeping | May feel comforting at first | Hyperextends spine and twists neck | Thin pillow under pelvis; avoid long-term use |
This table isn’t one-size-fits-all—but it can help you start fine-tuning your sleep position to suit your body’s needs.
How Stress and Sleep Posture Interact
Stress doesn’t just live in the mind—it shapes how your body holds tension, including during sleep. People experiencing chronic stress or anxiety often unconsciously clench muscles at night, particularly in the hips, lower back, and jaw. This muscular rigidity carries over into sleep posture, often locking the body into tense positions that prevent full relaxation.
This connection explains why people with persistent lower back pain often have accompanying sleep disorders or report waking up still tired. The body remains in a hypervigilant state, even during rest, limiting tissue repair and reducing the calming effects of sleep.
Incorporating calming rituals before bed—like deep breathing, gentle mobility work, or low-light journaling—can reduce this tension and help the spine decompress naturally. If anxiety is contributing to your pain, consider reviewing natural strategies to reduce anxiety without medication, as emotional support and physical recovery are deeply intertwined.
Morning Routine to Counteract Nighttime Stiffness
Waking up with tightness or pain in the lower back is often a sign that your fascia, joints, or muscles remained static and slightly compressed overnight. Implementing a short morning routine can help release stiffness, restore fluid movement, and realign the spine before daily stress builds up.
Start by lying on your back and gently pulling one knee to the chest, then the other, holding each stretch for 20–30 seconds. You can then transition to pelvic tilts or gentle spinal rotations from side to side. Avoid sudden bending or twisting—morning tissue is less hydrated and more vulnerable.
Breathing deeply while moving helps stimulate the parasympathetic nervous system, aiding both spinal relaxation and mental readiness. Just as morning toe stretches assist in plantar fasciitis recovery, these morning back-release movements help prevent pain flare-ups from the very first steps.
How Lifestyle and Daily Habits Affect Sleep and Back Health
Even with the best sleeping posture, poor daytime habits can undermine progress. Slouching at a desk, skipping movement breaks, or carrying heavy bags unevenly builds tension throughout the day—tension that often expresses itself overnight as pain.
Frequent sitting, particularly in deep or unsupportive chairs, shortens the hip flexors and weakens the glutes—both of which impact lower back stability. Incorporating micro-movements throughout the day, using ergonomic seating, and wearing shoes with good arch support create a more balanced musculoskeletal system.
These strategies don’t just reduce pain at night—they set the tone for better rest. Much like in magnesium deficiency, where multiple symptoms overlap, back pain often reflects a full-body imbalance. Improving daytime awareness supports nighttime recovery.
When to Consult a Specialist for Persistent Back Pain
If your back pain disrupts sleep for more than 4–6 weeks, spreads to the legs, or is accompanied by numbness or loss of function, it’s time to consult a specialist. Pain that worsens rather than improves with postural changes or remains constant throughout the night may indicate disc issues, spinal stenosis, or inflammation requiring medical evaluation.
A physical therapist can help retrain your body mechanics and tailor sleep adjustments to your anatomy. In some cases, imaging (MRI or X-ray) may be needed. However, most sleep-related back pain is mechanical, not structural—and improves dramatically with consistent alignment and mobility strategies.
Getting professional input doesn’t mean giving up on home care. Instead, it helps fine-tune your approach and catch underlying contributors before they become long-term problems.
Building a Sustainable, Personalized Sleep Strategy
The best sleeping position for lower back pain is the one that you can maintain consistently and that allows your spine to rest in a neutral, supported state. That may mean back sleeping with a knee pillow, side sleeping with full-body support, or combining techniques that evolve with your needs.
It’s not just about where you sleep—but how you prepare, move, and support your body through the entire 24-hour cycle. Creating a nighttime wind-down routine, ensuring alignment during the day, and being responsive to morning stiffness are all part of an integrated healing loop.
This is less about chasing perfect posture and more about teaching your body to trust rest again. That trust—like any form of recovery—is built with patience, presence, and consistency.
FAQ
What is the best sleeping position for lower back pain?
The best sleeping position is usually on your side with a pillow between your knees, or on your back with a pillow under your knees. Both support the natural curve of the lumbar spine and reduce tension in the lower back. These positions help distribute weight evenly and avoid twisting or sagging of the spine that worsens discomfort overnight.
Why does my lower back hurt more at night?
Pain can intensify at night due to poor posture during sleep, a worn-out mattress, or tense muscles settling into static positions. Inflammation may also accumulate when the body is still for hours, making stiffness worse in the morning. Stress and anxiety can further aggravate symptoms by increasing muscular tension and reducing sleep quality.
Is it bad to sleep on your stomach with back pain?
Sleeping on your stomach is generally discouraged for lower back pain because it causes the spine to hyperextend and the neck to twist unnaturally. This puts pressure on lumbar joints and can worsen inflammation. If you must sleep on your stomach, placing a thin pillow under the pelvis can reduce strain slightly.
Can a bad mattress cause lower back pain at night?
Yes. A mattress that’s too soft or too firm can misalign the spine, causing or worsening back pain. Ideally, you should use a medium-firm mattress that supports your spine while allowing pressure points like the hips and shoulders to settle comfortably. Your sleeping position should guide the level of firmness you choose.
What type of pillow helps with lower back pain?
A proper pillow supports not just your head but your whole posture. For side sleepers, a thicker pillow that keeps the neck aligned works best. For back sleepers, a medium-height pillow under the head and a smaller one under the knees can relieve lumbar stress. Using pillows to support your knees or hips reduces pelvic rotation and keeps the spine in a healthy alignment.
How can I reduce back stiffness in the morning?
Gentle stretches in bed, such as knee-to-chest pulls, pelvic tilts, or spinal rotations, help release overnight tension. Standing slowly and avoiding quick bends also prevent sudden strain. Think of this like early movement routines used in plantar fasciitis home care—the body needs time to ease back into action after hours of stillness.
Is side sleeping better on the left or right?
Sleeping on the left side may offer additional benefits like better digestion and reduced acid reflux, though both sides can be good for back pain if the spine is properly aligned. Switching sides throughout the night is a good habit to prevent muscular imbalances and pressure buildup on one side of the body.
Can anxiety affect my back pain at night?
Absolutely. Anxiety can increase muscle tension, interfere with deep sleep, and make your nervous system more sensitive to pain. Nighttime clenching of muscles—especially in the hips, jaw, or spine—may worsen back discomfort. Incorporating practices from natural anxiety reduction methods can significantly improve sleep and pain resilience.
How many pillows should I use to sleep better with back pain?
It’s not about quantity but strategic placement. Usually, one pillow under your head and one between or under your knees is sufficient. You might also use a small lumbar roll for back support. Using too many pillows can over-elevate your body and misalign the spine, so focus on neutral positioning instead of stacking.
Why do I wake up sore even after 8 hours of sleep?
Poor spinal alignment during sleep, insufficient mattress support, or lack of movement before bed can leave muscles tight and inflamed despite long sleep duration. Sleep quality matters more than sleep quantity when it comes to musculoskeletal recovery. A few minutes of nighttime stretching or realignment can make a significant difference.
Can sleeping positions help relieve sciatica?
Yes. Sleeping in the fetal position or on your side with a pillow between the knees often reduces sciatic nerve compression by slightly opening the spinal canal. Avoid lying flat on your back with legs extended, as this can aggravate nerve irritation. Proper pillow support is especially important in these cases.
How long does it take to feel better after changing sleep positions?
Many people notice relief within a few nights to one week if they maintain consistent positioning and support. However, full muscular adaptation and reduced inflammation may take 2–4 weeks, especially if the pain has been chronic. Like treating magnesium-related fatigue or pain from deficiency, consistency leads to change over time.
Is it okay to sleep in a recliner for back pain?
For some people—especially those recovering from surgery or experiencing disc pain—sleeping in a reclined position can reduce pressure on the spine. It allows the hips and knees to remain flexed and can relieve nerve tension. However, long-term use of recliners may create other postural issues unless properly cushioned.
Should I stretch before bed to reduce pain overnight?
Yes. Gentle stretching of the hamstrings, hip flexors, and lower back before bed helps release tension and prepare the spine for stillness. Avoid intense or aggressive stretching—keep it slow and focused on relaxation. Evening mobility work can also improve sleep quality by calming the nervous system.
Do magnesium supplements help with nighttime back pain?
In some cases, yes. Magnesium supports muscle relaxation and nerve regulation, and low levels have been associated with cramping and chronic pain. If you suspect a deficiency—especially if you also have symptoms like muscle twitching or insomnia—it may be worth exploring magnesium deficiency symptoms and adjusting your intake accordingly.









