Best Birth Control Methods for Women Over 35

Choosing the best birth control method for women over 35 is not always straightforward. At this stage of life, fertility naturally begins to decline, but pregnancy is still possible — and sometimes riskier for both mother and baby. Many women also start noticing health changes such as high blood pressure, migraines, or changes in menstrual cycles, which can affect the safety of certain contraceptive options.
In my clinical experience, I often meet patients who ask whether the pill they have been taking for years is still the safest choice. Others are considering switching to long-term solutions like an IUD or even permanent contraception. The truth is that there is no single “best” option that fits everyone. The safest choice depends on your overall health, lifestyle, and future family planning goals.
This guide will review the most reliable contraceptive options for women over 35, including both hormonal and non-hormonal methods. We will also look at which options may carry higher risks, especially for women who smoke or have chronic conditions. By the end, you’ll understand how to work with your doctor to select a method that balances effectiveness, safety, and personal needs.
Why does age matter in family planning after 35?
Even though many women stay healthy and active well into their 30s and 40s, age still plays a major role in reproductive health. After 35, natural fertility begins to decline, hormone levels shift, and health risks such as high blood pressure or diabetes become more common. These changes influence not only the chances of pregnancy but also the safety and effectiveness of different contraceptive methods.
How fertility naturally changes in your late 30s
After 35, women often notice that getting pregnant is not as easy as it once was. This is because the number and quality of eggs naturally decline with age. By the late 30s, ovulation can become less predictable, and the chances of conception each month decrease.
In my practice, I sometimes meet women who are surprised to learn that even if they still have regular periods, their fertility may already be lower. For some, this means they may worry less about unintended pregnancy, while for others it creates anxiety about planning for children in the future.
It is important to remember that a decline in fertility does not equal zero fertility. Pregnancy is still possible — and for some women, it may come with higher health risks. That is why choosing the right contraceptive option for women over 35 is not just about preventing pregnancy, but also about protecting overall health and supporting long-term family planning goals.
Hormonal shifts and their impact on contraceptive choices
Around the age of 35, natural hormone patterns begin to change. Estrogen and progesterone levels may fluctuate more, leading to irregular periods, heavier bleeding, or new symptoms like hot flashes and mood swings. These hormonal shifts can make some methods of contraception less comfortable or increase their side effects.
For example, women who notice more intense migraines or premenstrual symptoms may find that certain birth control pills worsen their condition. On the other hand, hormonal IUDs can sometimes help reduce heavy bleeding and painful cramps, making them a better fit for this stage of life. Choosing the right contraceptive method after 35 often requires balancing symptom control with overall safety.
Why age raises certain health risks
By the mid-30s, many women also develop health conditions that affect contraceptive safety. High blood pressure, diabetes, or a history of blood clots can make hormonal options riskier. Smoking after 35 is another major concern, since it sharply increases the risk of cardiovascular events when combined with estrogen-containing birth control.
In my practice, I often remind patients that while contraception is mainly about preventing pregnancy, it must also protect long-term health. A method that worked well in the 20s may need to be reconsidered in the late 30s. This is why regular check-ups and open conversations with a healthcare provider are so important when choosing the safest contraceptive plan.
Non-hormonal contraceptive methods for women over 35
Not every woman wants or can safely use hormones. For those with certain medical conditions, or for women who simply prefer to avoid hormone-based contraception, non-hormonal options can be highly effective. These methods focus on long-term protection or barrier strategies, giving women more flexibility and control over family planning.
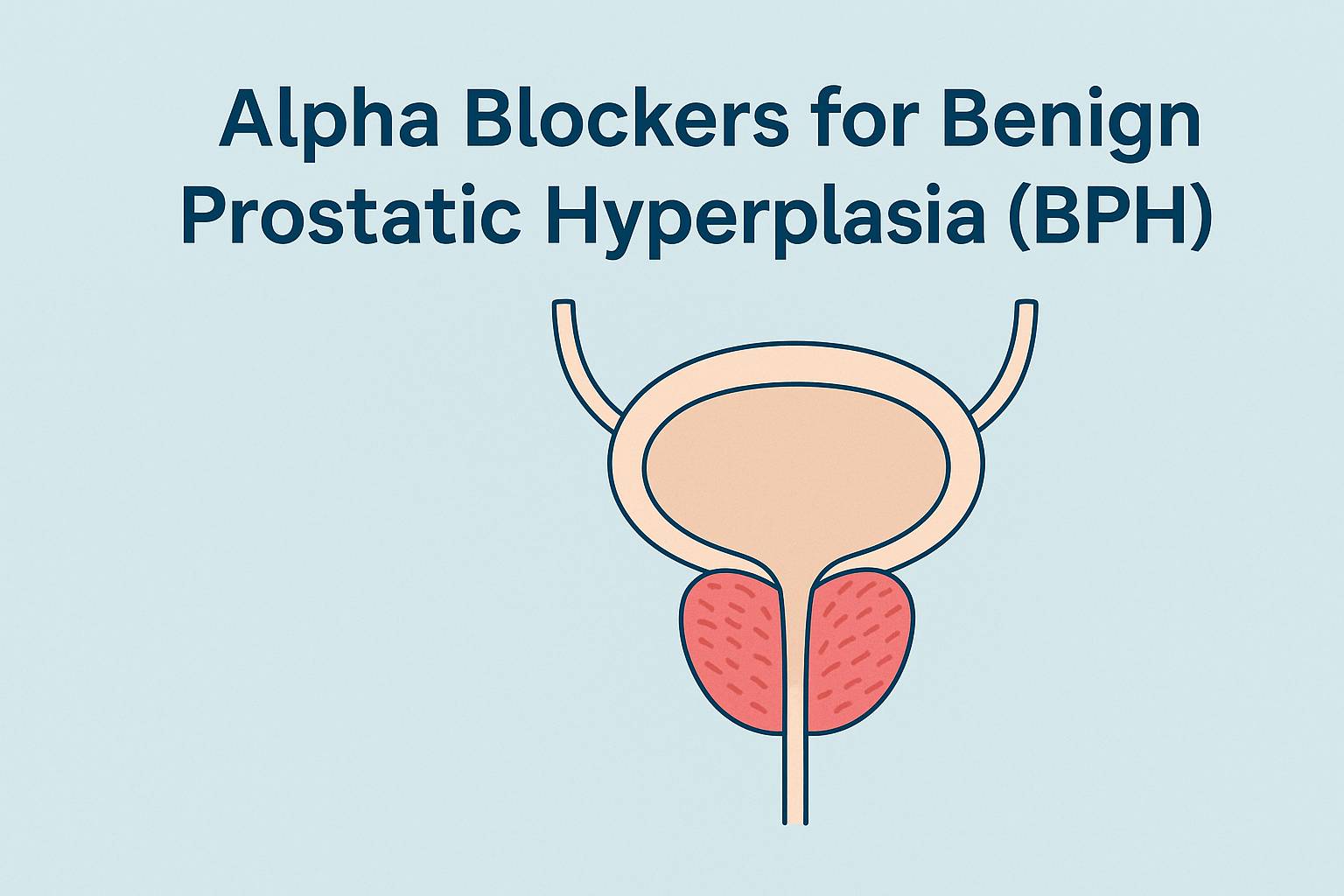
Copper IUD — long-term, hormone-free solution
The copper intrauterine device (IUD) is one of the most effective non-hormonal contraceptive options available. Once inserted by a healthcare professional, it can provide reliable protection for up to 10 years. Because it does not use hormones, it avoids side effects like mood swings, headaches, or weight gain that some women experience with hormonal methods.
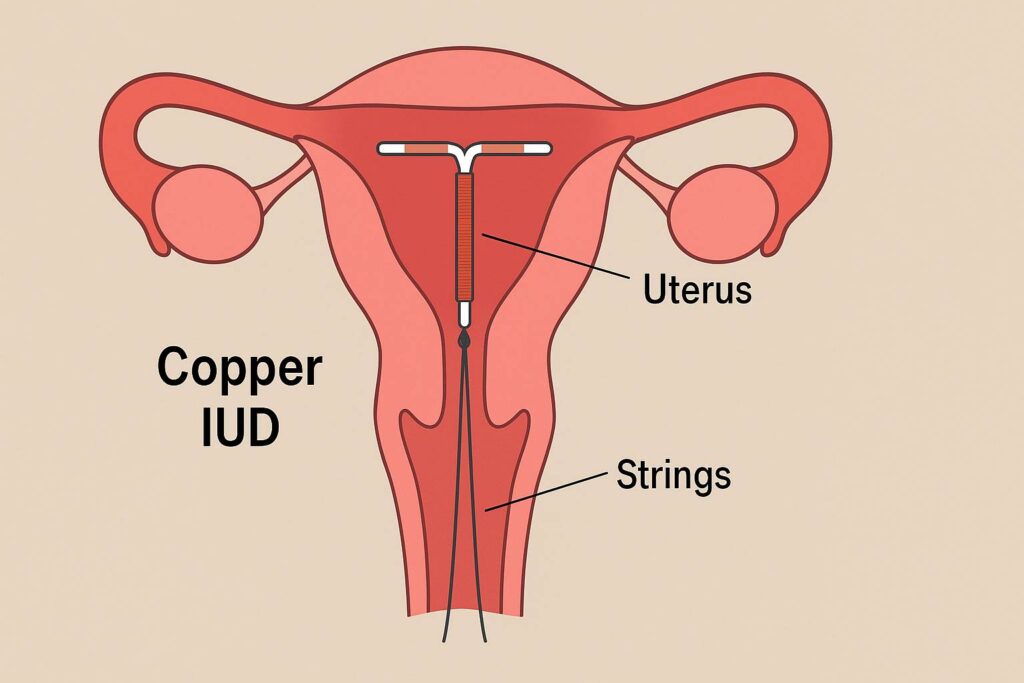
In my clinical practice, many women over 35 appreciate the copper IUD for its convenience. They like the idea of not having to remember a daily pill. However, it’s important to know that copper IUDs can sometimes make periods heavier or more painful, especially in the first months after insertion. This is why I usually recommend it for women who already have normal or light menstrual cycles.
Barrier methods (condoms, diaphragm, cervical cap)
Barrier methods physically prevent sperm from reaching the egg. Condoms, diaphragms, and cervical caps are widely accessible, hormone-free, and have the added benefit of protecting against sexually transmitted infections (STIs). This makes them an important option for women who may be entering new relationships after 35.
That said, barrier methods are less effective than long-term options like IUDs. Their success depends heavily on correct and consistent use. In practice, I often advise patients who want maximum reliability to combine barrier methods with another contraceptive strategy — for example, using condoms together with a copper IUD. This way, they gain both pregnancy prevention and protection against infections.
Permanent solutions (tubal ligation, vasectomy for partner)
For women who are certain they do not want more children, permanent contraception may be the most practical option. Tubal ligation, sometimes called “getting your tubes tied,” is a surgical procedure that blocks or seals the fallopian tubes so that eggs cannot meet sperm. It is highly effective and considered a safe option for women who are finished with family building.
Another permanent solution is vasectomy for a male partner. This procedure is simpler, less invasive, and usually has a faster recovery time compared to tubal ligation. In my practice, I often see couples discussing both procedures together. The decision often depends on who feels more comfortable undergoing the surgery and the couple’s long-term goals.
It is important to note that while these procedures are considered permanent, they are not easily reversible. That is why doctors usually recommend them only when a woman or couple is absolutely certain about not wanting future pregnancies. For women over 35 who are confident in this decision, permanent contraception can provide peace of mind without the need for ongoing management.
Hormonal contraceptive methods for women over 35
Hormonal methods remain popular among women in their late 30s and 40s. They can regulate cycles, reduce pain, and in some cases even improve symptoms like heavy bleeding or anemia. However, because hormones affect the cardiovascular system and overall health, not every option is safe for every woman after 35. Let’s look at the most common hormonal methods in more detail.
Hormonal IUD — lighter periods and reliable protection
The hormonal intrauterine device (IUD) is a small device placed inside the uterus that slowly releases progestin. It is more than 99% effective and lasts between 3 and 7 years, depending on the type. For many women, the biggest benefit is lighter or even absent periods, which can be a welcome change after years of heavy or painful menstruation.
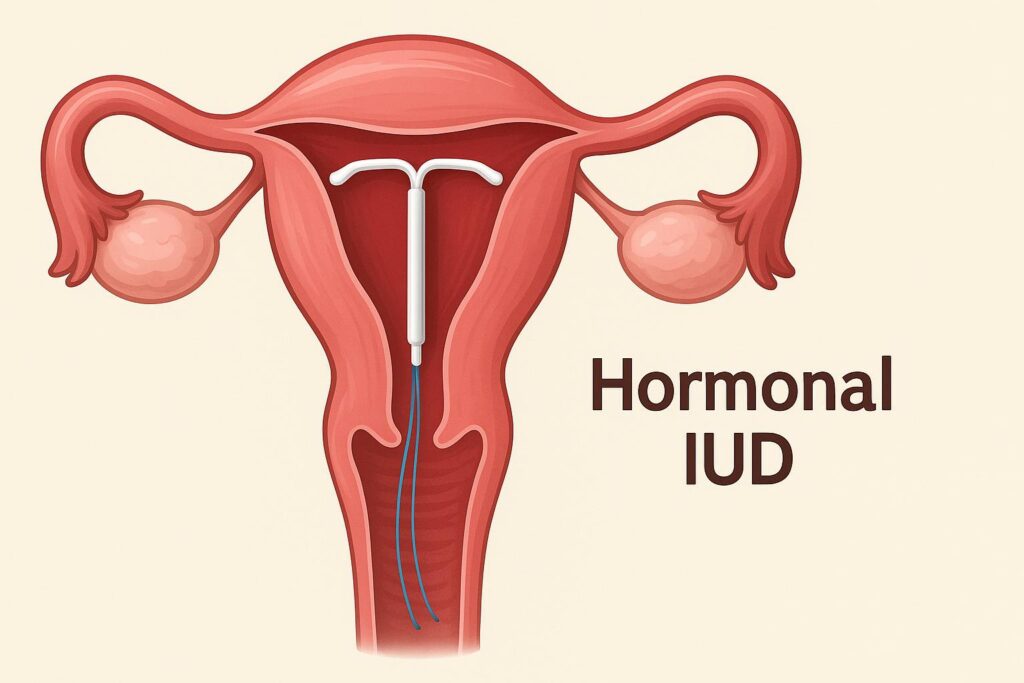
In my practice, women over 35 often choose the hormonal IUD because it combines long-term protection with a relatively low hormone dose. Unlike daily pills, it works in the background without requiring constant attention. The main downsides are irregular spotting in the first months and, in rare cases, device displacement. Still, for most healthy women, it is one of the safest and most convenient hormonal options.
Oral contraceptives (the pill) — benefits and cautions
Oral contraceptives remain a common choice, even after 35. They regulate menstrual cycles, improve acne, and can reduce the risk of ovarian and endometrial cancer. For women without major health concerns, the pill can still be a safe and effective option.
However, risks increase with age, especially for women who smoke, have high blood pressure, or suffer from migraines with aura. In these cases, estrogen-containing pills are usually not recommended because they raise the chance of blood clots and cardiovascular events. In my clinical experience, I often review each woman’s medical history carefully before continuing or starting the pill after 35. Safer alternatives, such as progestin-only pills or IUDs, may be better for some patients.
Contraceptive implant — low maintenance, high effectiveness
The contraceptive implant is a tiny rod placed under the skin of the upper arm. It releases a steady dose of progestin, providing protection for up to three years. With an effectiveness of over 99%, it is one of the most reliable birth control options available.
In my practice, many women over 35 choose the implant because it is “set and forget.” Once inserted, there is no daily or weekly routine — it simply works in the background. The most common side effects are irregular bleeding or, in some cases, lighter or absent periods. A few women also report headaches or mood changes. Still, for those who want a low-maintenance option without estrogen, the implant is often an excellent choice.
Injections — practical but may affect bone health
Contraceptive injections, usually given every three months, are another progestin-only option. They are highly effective and convenient for women who prefer not to take a daily pill or use a device.
However, long-term use of injections has been linked to a decrease in bone mineral density. This is especially important for women over 35, since bone health naturally begins to decline with age. In my clinical experience, I usually recommend injections as a short- to medium-term solution rather than a lifelong method. With proper monitoring, they can be safe and effective, but women at risk of osteoporosis may want to consider other options.
Which contraception methods may carry higher risks after 35?
While many contraceptive methods remain safe and effective for women in their late 30s and beyond, some options become riskier with age. Health conditions such as high blood pressure, diabetes, or a history of migraines can influence safety, and lifestyle factors like smoking can significantly increase complications. Understanding these risks is essential for choosing a method that protects both reproductive and overall health.
The pill and smoking — a dangerous mix

One of the clearest warnings in women’s health is the combination of smoking and estrogen-containing birth control pills. After 35, this mix can sharply raise the risk of blood clots, heart attack, and stroke. The reason is that both smoking and estrogen affect the blood vessels and clotting system, and together they multiply the danger.
In my clinical experience, I have seen women who felt well on the pill for many years but developed complications once they continued smoking past 35. This is why most doctors strongly advise against taking combined oral contraceptives if you smoke.
For women in this situation, safer alternatives exist. Progestin-only pills, hormonal IUDs, implants, or copper IUDs provide effective contraception without the added cardiovascular risks. The key is to be honest with your healthcare provider about smoking habits. Even light or occasional smoking can increase risk, and it should never be overlooked when making contraceptive decisions.
High blood pressure, migraines, and hormonal contraception
As women age, health conditions like high blood pressure, diabetes, or migraines often become more common. These conditions can affect how safe hormonal contraception is after 35. For example, women with uncontrolled hypertension may face a higher risk of stroke or heart disease if they use estrogen-based methods.
Migraines with aura deserve special attention. Research shows that combining this condition with estrogen-containing birth control significantly increases the chance of blood clots or stroke. In my practice, I always ask patients detailed questions about headaches before prescribing any hormonal method.
Safer alternatives include progestin-only options, such as the hormonal IUD, implant, or mini-pill. These provide effective contraception without the same level of cardiovascular risk. The key is careful evaluation: a woman’s medical history should always guide the choice of method.
When to avoid the patch or vaginal ring
The contraceptive patch and vaginal ring deliver hormones directly into the bloodstream, bypassing the digestive system. While convenient, they still contain estrogen and carry similar risks to birth control pills. For women over 35, especially those who smoke or have other health issues, these methods may not be the safest choice.
In clinical practice, I have seen women develop skin irritation from the patch or struggle with correct placement of the ring. But the greater concern is cardiovascular safety. Doctors generally advise caution for women with risk factors such as smoking, obesity, hypertension, or a history of blood clots.
For women seeking convenience without estrogen, alternatives like the implant, copper IUD, or progestin-only injection are often better suited. These options reduce risk while still providing reliable protection.
How to choose the right contraceptive method with your doctor
Selecting the safest and most effective birth control after 35 is rarely a one-size-fits-all decision. Each woman brings her own health history, lifestyle, and family planning goals. That’s why working closely with a healthcare provider is the best way to balance effectiveness, safety, and personal comfort.
Considering personal medical history (diabetes, hypertension, migraines)
A woman’s medical background plays a major role in choosing the right contraceptive method. Conditions such as diabetes, high blood pressure, or migraines can change which options are safe and which should be avoided. For example, women with uncontrolled hypertension may face higher risks if they use estrogen-containing pills, patches, or rings.
Migraines, particularly those with aura, are another red flag. In my clinical experience, I’ve seen patients who only realized the connection between their headaches and contraception after discussing their full health history. This is why doctors usually recommend progestin-only methods — such as the hormonal IUD, implant, or mini-pill — for women with certain medical concerns.
Diabetes adds another layer of complexity. Some women with diabetes can safely use hormonal contraception, but those with vascular complications may need non-hormonal options like the copper IUD. A personalized approach is key: the safest method is the one that fits not just reproductive goals but also long-term health.
Lifestyle and family planning goals
Beyond medical history, lifestyle and personal goals strongly shape which contraceptive method makes sense after 35. A woman who wants another pregnancy in the future may prefer a reversible method such as an IUD or implant. By contrast, someone who is certain her family is complete may consider permanent options like tubal ligation or her partner’s vasectomy.
Lifestyle also matters. For women who travel frequently, have busy work schedules, or struggle to take a pill at the same time each day, “set and forget” methods — like the implant or IUD — may be more practical. In my practice, I often hear patients say they want something they don’t have to think about daily. Aligning contraception with real-life habits ensures better consistency and fewer failures.
The importance of shared decision-making
Choosing a contraceptive method should never feel like a one-sided decision. Shared decision-making means that the patient and doctor discuss options openly, weighing effectiveness, side effects, and individual priorities. This approach empowers women to make informed choices instead of simply following a standard prescription.
In my clinical experience, women often feel more confident and satisfied with their contraception when they are part of the decision-making process. For example, a patient may initially think she wants oral contraceptives, but after reviewing her risk factors and lifestyle, she may realize that an IUD is a safer and more convenient fit. Shared decision-making ensures that the chosen method matches both medical needs and personal values.
Lifestyle factors that influence contraception safety
Even with the right medical history, lifestyle choices can influence how safe different contraceptive methods are after 35. Habits such as smoking, diet, exercise, and weight management all play a role in overall health and can change the balance of benefits and risks.
Smoking and cardiovascular risks
Smoking is one of the most significant lifestyle factors that affects contraception safety in women over 35. Nicotine and other chemicals in cigarettes damage blood vessels and increase the risk of blood clots, heart attack, and stroke. When combined with estrogen-containing birth control methods — such as the pill, patch, or vaginal ring — the risk becomes dangerously high.
In my clinical practice, I strongly advise women who smoke to avoid estrogen-based contraception altogether. Safer alternatives include progestin-only pills, hormonal IUDs, implants, or non-hormonal options like the copper IUD. These methods provide effective protection without adding to cardiovascular risk.
It is also important to note that even light or occasional smoking is not harmless. Many patients assume that smoking “only on weekends” is less risky, but research shows that any exposure increases the chance of complications when paired with hormonal contraception. For women over 35, quitting smoking is one of the most powerful steps to improve both contraceptive safety and overall health.
Weight, metabolic health, and contraceptive effectiveness
Body weight and metabolic health can also influence how well certain contraceptive methods work. Research shows that obesity may slightly reduce the effectiveness of some methods, particularly the contraceptive patch. Extra body fat can alter hormone absorption, meaning estrogen levels may not stay high enough for full protection.
In my practice, I always review metabolic health with patients — including blood sugar levels, cholesterol, and weight management — before recommending a method. For many women with obesity or metabolic syndrome, long-acting reversible contraception (LARC) such as the implant or IUD remains highly effective and safe. These options bypass the digestive system and are less affected by body weight.
It’s important to highlight that weight alone should not discourage women from using contraception. The goal is to select a method that fits both medical needs and lifestyle while ensuring strong, consistent protection.
Exercise, diet, and hormone balance
Healthy habits such as regular exercise and a balanced diet can support both hormonal stability and overall well-being. For women over 35, lifestyle choices often make the difference between tolerating contraception well or struggling with side effects. For example, regular physical activity improves cardiovascular health and lowers the risk of blood clots, which is especially important for women on hormonal methods.
Diet also plays a role. A nutrient-rich diet with adequate calcium and vitamin D supports bone health, which can be impacted by contraceptive injections. Anti-inflammatory foods may reduce menstrual cramps and bloating, helping women tolerate certain methods better.
In my clinical experience, patients who combine healthy habits with the right contraceptive method often report fewer side effects and better overall satisfaction. While no diet or workout plan can replace medical treatment, they provide a strong foundation for safe and effective contraception.
H2: When to seek medical attention immediately
Most contraceptive methods are safe when used correctly, but sometimes serious side effects can appear. Women over 35 should know the warning signs that require urgent medical evaluation. Acting quickly can prevent life-threatening complications and ensure safer long-term use of contraception.
Warning signs of blood clots
Blood clots are a rare but serious complication of hormonal contraception, especially estrogen-containing methods. Symptoms may include swelling, warmth, or pain in one leg, often in the calf, or sudden shortness of breath if a clot travels to the lungs.
In my clinical experience, I tell patients to treat these signs as emergencies. A blood clot can progress rapidly and requires immediate medical care. Women who smoke, have a family history of clotting disorders, or live a sedentary lifestyle face higher risks. Safer alternatives such as progestin-only or non-hormonal methods may be more appropriate for these patients.
Chest pain, severe headaches, or vision changes
Sudden chest pain, shortness of breath, or pain radiating to the arm may indicate a heart attack. Severe migraines with visual changes — flashing lights, blurred vision, or temporary vision loss — may be linked to increased stroke risk, particularly in women on estrogen-based contraception.
I advise patients never to ignore these symptoms. Even if they seem minor or pass quickly, they may signal serious complications. Prompt evaluation by a healthcare provider is the safest course of action. Switching to safer methods, such as hormonal IUDs or copper IUDs, is often recommended in these cases.
Unexpected bleeding or pelvic pain
Changes in menstrual bleeding are common with contraception, but sudden heavy bleeding, bleeding after sex, or persistent pelvic pain should not be dismissed. These symptoms may point to uterine fibroids, ovarian cysts, or, rarely, gynecologic cancers.
In my practice, I emphasize the importance of monitoring any new or unusual bleeding patterns, especially for women over 35. A thorough gynecologic exam, ultrasound, or blood test can help determine the cause. Early evaluation ensures that more serious conditions are not missed and that contraception remains both safe and effective.
Pros and cons summary — comparison table
When comparing contraceptive methods for women over 35, it helps to see the main differences side by side. The table below summarizes how effective each method is, how long it lasts, who it may be best suited for, and which risks should be considered after 35.
| Method | Effectiveness | Duration | Best suited for | Risks after 35 |
|---|---|---|---|---|
| Copper IUD | ~99% | Up to 10 years | Women wanting long-term, hormone-free option | May cause heavier or more painful periods |
| Hormonal IUD | ~99% | 3–7 years | Women with heavy bleeding or painful cycles | Irregular spotting in first months |
| Oral contraceptives (the pill) | ~91% (typical use) | Daily use | Women with regular cycles, no major health risks | ↑ risk of clots if smoking, hypertension, migraines |
| Contraceptive implant | ~99% | Up to 3 years | Women wanting “set and forget” option | Irregular bleeding, mood changes |
| Injections | ~94% | Every 3 months | Women preferring short- to medium-term option | May reduce bone density over time |
| Barrier methods (condoms, diaphragm, cervical cap) | ~79–85% typical use | Each act of sex | Women wanting STI protection, hormone-free option | Lower effectiveness if not used correctly |
| Tubal ligation | >99% | Permanent | Women certain about no future pregnancies | Surgical risks, irreversible |
| Vasectomy (partner) | >99% | Permanent | Couples certain about no future pregnancies | Requires partner’s consent, irreversible |
FAQs
1. Is contraception safe for women over 35?
2. Can I take the pill after 35 if I smoke?
3. What is the most effective contraceptive method in your late 30s?
4. Does hormonal contraception increase the risk of cancer?
5. Can birth control pills affect fertility after 35?
6. Which contraceptive options protect against STIs?
7. Do these methods delay menopause?
8. Is it harder to get pregnant after stopping contraception at 35+?
9. What’s the safest contraceptive for women with high blood pressure?
10. Are natural methods (cycle tracking, withdrawal) reliable after 35?
11. Is permanent contraception a good choice at this age?
12. How much do contraceptive methods cost in the US?
Expert’s Closing Note
“As a physician, I know how confusing it can feel to choose birth control after 35. Some methods remain very safe, while others may carry higher risks depending on your health and lifestyle. My advice is simple: never make this decision alone. Discuss your medical history, habits, and family planning goals with your doctor. The right choice will not only protect against pregnancy but also support your long-term health and peace of mind.”