Benign Prostatic Hyperplasia (BPH): Symptoms, Diagnosis, and Treatment
“In my 12 years of medical practice, I have often met patients struggling with urinary symptoms caused by an enlarged prostate. Many feared it was cancer, but in most cases it was benign prostatic hyperplasia (BPH) — a common, non-cancerous condition. In this guide, I will explain what BPH is, how doctors diagnose it, and the treatment options that can improve quality of life.”
Benign prostatic hyperplasia (BPH), also known as an enlarged prostate, is a common condition that affects many men as they get older. The prostate gradually grows and presses against the urethra, leading to urinary difficulties such as weak stream, frequent urges, and nighttime interruptions. While these symptoms often cause anxiety, BPH is not cancer. It is a benign condition that can be effectively managed through proper diagnosis, medications, and treatment options tailored to each patient’s needs.
What is Benign Prostatic Hyperplasia (BPH)?
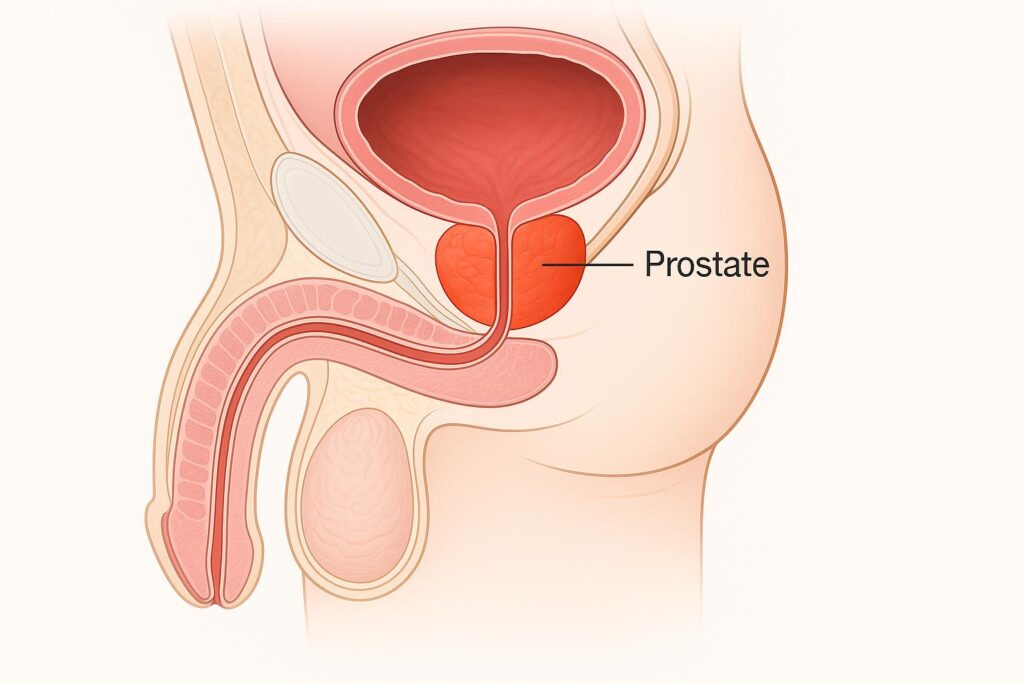
BPH means the prostate gland has increased in size without being cancerous. This condition develops gradually and often becomes noticeable after the age of 40–50. Understanding what BPH is helps men separate it from more serious diseases and recognize that effective treatments exist.
Definition and overview
Doctors define benign prostatic hyperplasia as a non-cancerous enlargement of the prostate gland. The growth happens in the central part of the prostate, where it surrounds the urethra. As the gland expands, it narrows the urinary passage and creates typical symptoms like weak flow and incomplete emptying.
In practice, BPH does not spread to other organs and does not threaten life. Its impact comes mainly from urinary obstruction and the stress these symptoms bring. Early recognition allows men to take steps that reduce discomfort and prevent long-term complications.
ICD-10 code for BPH
In medical records, doctors classify BPH using the ICD-10 system. The main code is N40, which covers benign prostatic hyperplasia without complications. Subcategories like N40.1 identify BPH with lower urinary tract symptoms, helping physicians document the severity more precisely.
This coding supports accurate diagnosis, treatment planning, and insurance coverage. When a doctor assigns an ICD-10 code for prostate enlargement, it ensures that the patient’s condition is recorded clearly and can be followed consistently across different stages of care.
Common Symptoms of an Enlarged Prostate
An enlarged prostate develops slowly, and many men first notice changes in how they urinate. These symptoms may appear mild at the beginning but often progress over time. Recognizing them early helps patients seek care before the condition disrupts daily life.

Urinary difficulties (weak stream, frequency, urgency)
The most common benign prostatic hyperplasia symptoms involve problems with urination. Men may experience a weak or interrupted stream, the need to strain, or the feeling that the bladder never empties fully. These issues occur because the enlarged gland squeezes the urethra and obstructs urine flow.
Another frequent complaint is increased urgency and frequency, especially during the day. Some patients report sudden strong urges to urinate that are hard to control. These changes often create anxiety and frustration, pushing men to seek medical advice.
Impact on daily life and sleep (nocturia, discomfort)
BPH symptoms extend beyond the bathroom. Nighttime urination, known as nocturia, interrupts sleep and leaves men tired during the day. This constant disruption can lower productivity, affect mood, and reduce overall quality of life.
The discomfort of always planning around bathroom access also takes a toll. Many men avoid long trips, social events, or situations without easy toilet access. Over time, this lifestyle limitation adds stress and highlights the importance of diagnosis and treatment.
Diagnosis and Medical Classification
Doctors use a structured approach to confirm BPH and rule out other causes of urinary problems. A proper diagnosis not only identifies the condition but also guides treatment options and prevents unnecessary worry about cancer.
Clinical examination and tests
The first step is a detailed medical history and a physical exam. Doctors ask about urinary symptoms, their duration, and how much they affect daily life. A digital rectal examination helps assess the size and consistency of the prostate.

Additional tests provide more accuracy. Urine flow studies, PSA blood tests, and ultrasound imaging help confirm the presence of prostate enlargement and evaluate potential complications. Together, these tools create a clear picture of the patient’s condition.
ICD-10 coding for prostate enlargement
To classify the condition, physicians rely on the ICD-10 system. The primary category is N40, which covers benign enlargement of the prostate. Subcodes allow doctors to specify whether lower urinary tract symptoms are present, ensuring a precise medical record.
Using ICD-10 for benign prostatic hyperplasia supports clear communication across clinics, accurate insurance documentation, and consistent follow-up. This coding helps align diagnosis with treatment plans and improves continuity of care.
Medications and Drug Therapies for BPH
Medication often serves as the first line of treatment for men with bothersome urinary symptoms. Drug therapy reduces discomfort, improves quality of life, and may delay the need for surgery. Doctors choose the medication based on prostate size, severity of symptoms, and patient health profile.
Alpha blockers
Doctors frequently prescribe alpha blockers for benign prostatic hyperplasia because these drugs relax the muscles in the prostate and bladder neck. This relaxation improves urine flow and makes it easier for the bladder to empty. Patients usually notice relief within days or weeks of starting therapy.

Alpha blockers do not shrink the prostate but provide quick symptom control. They may cause side effects such as dizziness or low blood pressure, so physicians adjust the dose carefully. For many men, these medications offer a safe and effective way to manage urinary difficulties linked to BPH.
5-alpha-reductase inhibitors
Doctors prescribe 5-alpha-reductase inhibitors to shrink the prostate by blocking the hormone that fuels its growth. These medications work more slowly than alpha blockers, often requiring several months before noticeable improvement occurs. The main benefit is long-term reduction in prostate size, which lowers the risk of urinary retention and the need for surgery.
Patients taking these drugs should know that they can reduce PSA levels, which affects prostate cancer screening. Side effects may include reduced sexual drive or erectile changes. Despite this, for men with significantly enlarged prostates, these inhibitors provide durable relief and disease control.
Combination therapies and other medications
In some cases, doctors combine alpha blockers with 5-alpha-reductase inhibitors. This dual approach offers both immediate symptom relief and long-term prostate shrinkage. Clinical studies confirm that combination therapy reduces progression risk more effectively than either medication alone.
Other benign prostatic hyperplasia medications include anticholinergics for bladder overactivity or phosphodiesterase-5 inhibitors, which can also improve erectile function. Physicians tailor these treatments to individual needs, balancing effectiveness with side effect profiles to achieve the best outcome.
Treatment Options for Prostate Enlargement
When medications no longer provide enough relief, doctors consider procedural options. Advances in technology now allow less invasive techniques before moving to traditional surgery. Choosing the right method depends on prostate size, overall health, and how much symptoms affect daily life.
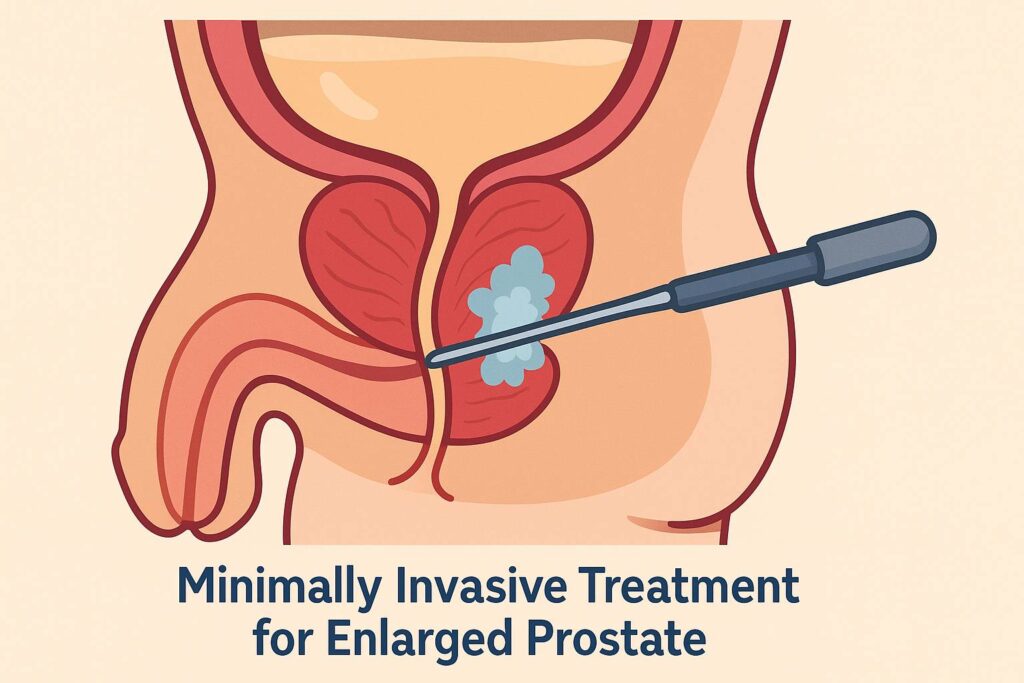
Minimally invasive therapies
Minimally invasive procedures represent an important category of benign prostatic hyperplasia treatment. Options such as transurethral microwave therapy, water vapor therapy, or prostatic urethral lift reduce tissue obstruction without major surgery. These treatments often take place in an outpatient setting and allow for faster recovery.
Patients benefit from symptom relief while avoiding the longer hospital stays linked to surgery. Some men may still need further treatment later, but these therapies provide a good balance between effectiveness and safety for those who want quicker recovery and minimal downtime.
Surgical approaches (TURP, laser therapy, prostatectomy)
When symptoms remain severe despite medication or minimally invasive procedures, doctors recommend surgery. The gold standard is transurethral resection of the prostate (TURP), which removes excess tissue and restores urine flow. Laser therapies, such as holmium laser enucleation, offer similar results with less bleeding and shorter hospital stays.
In rare cases of very large prostates, open or robotic-assisted prostatectomy may be necessary. These surgeries provide strong long-term relief but carry higher risks and longer recovery. Doctors weigh these factors carefully and select the procedure that best matches the patient’s condition and health status.
Lifestyle changes and natural remedies
Lifestyle adjustments support medical and surgical treatments. Reducing evening fluid intake, limiting caffeine and alcohol, and practicing timed voiding help control urinary urgency. Regular physical activity and maintaining a healthy weight also reduce symptom burden.
Some men explore natural remedies such as saw palmetto or beta-sitosterol supplements. Evidence remains mixed, but mild improvements are possible in selected patients. Doctors encourage open discussion about these options to ensure they do not interfere with prescribed therapies.
Living with BPH
Managing BPH does not end with a single treatment. It often requires ongoing strategies that adapt to changes in symptoms and overall health. With the right plan, most men keep their condition under control and maintain a good quality of life.
Managing symptoms long-term
Long-term management begins with regular check-ups. Doctors monitor prostate size, urinary flow, and PSA levels to adjust treatment when needed. Medications may continue for years, and in some cases, additional procedures ensure lasting relief.
Patients also play an active role in control. Staying hydrated but avoiding excess fluids in the evening, keeping a balanced diet, and exercising regularly all reduce symptom intensity. By combining medical guidance with healthy habits, men live more comfortably despite the presence of BPH.
Emotional and psychological aspects
Living with BPH affects more than the urinary system. Constant bathroom trips, poor sleep, and daily discomfort often create frustration and anxiety. Men may feel embarrassed to talk about these issues, which increases emotional stress and reduces quality of life.
Open communication with healthcare providers helps reduce this burden. Support from family and patient groups also provides reassurance. Addressing the psychological impact alongside physical treatment ensures a more complete approach to care.
When to see a doctor
Men should seek medical attention if urinary symptoms persist, worsen, or interfere with daily life. Warning signs include blood in the urine, painful urination, or sudden inability to pass urine, which require immediate evaluation.
Even mild symptoms deserve attention when they disrupt sleep or cause worry. Early consultation allows doctors to confirm the diagnosis, rule out cancer, and offer safe treatment options before complications arise.
FAQ About Benign Prostatic Hyperplasia
“As a physician, I know how stressful it can be to live with urinary problems linked to an enlarged prostate. Most cases involve benign prostatic hyperplasia (BPH), which is not cancer, but the symptoms still affect daily life. My advice is simple: do not ignore persistent changes in urination. If you notice worsening flow, frequent urges, or disrupted sleep, see a doctor promptly. Early evaluation brings peace of mind and ensures the best treatment outcome.”
Board-Certified Physician in Internal Medicine