Basal Cell Carcinoma
Basal Cell Carcinoma: Understanding ICD-10 Coding and Clinical Relevance
- What Is Basal Cell Carcinoma and Why Coding Matters
- Introduction to ICD-10: Structure and Purpose
- Coding Basal Cell Carcinoma by Anatomic Site
- How ICD-10 Codes Influence Treatment and Insurance
- Differences Between Basal Cell and Other Skin Cancers in ICD-10
- Documenting Recurrence and Multiple Tumors
- ICD-10 Coding for Complications and Comorbidities
- How ICD-10 Enhances Epidemiology and Cancer Registries
- ICD-10 and Anatomic Localization of Basal Cell Carcinoma
- Coding Basal Cell Carcinoma in Immunocompromised Patients
- Common Errors in Basal Cell ICD-10 Coding and How to Avoid Them
- Clinical Workflow Integration: From Dermatologist to Coder
- ICD-10 and Histological Subtypes of Basal Cell Carcinoma
- ICD-10 for Recurrent or Multiple Basal Cell Carcinomas
- Insurance, Billing, and Prior Authorization Challenges
- Surveillance, Long-Term Tracking, and ICD-10 in Oncology Registries
- Legal Implications and Coding Accuracy in Basal Cell Cancer
- ICD-10 in Telemedicine and Dermatologic Triage
- Global ICD-10 Use for BCC Surveillance and Research
- Challenges in Documenting BCC with Coexisting Conditions
- Coding and Treatment Planning: Why ICD-10 Matters Clinically
- When to Use Neoplasm Codes vs. Benign/Dysplastic Codes
- Transition from BCC to Other Skin Cancer Categories
- ICD-10 Codes and Insurance Claims: Denials and Appeals
- FAQ: Basal Cell Cancer ICD-10
What Is Basal Cell Carcinoma and Why Coding Matters

Basal cell carcinoma (BCC) is the most common form of skin cancer, accounting for nearly 80% of all non-melanoma skin cancer cases. It originates in the basal cells—small, round cells found in the lower part of the epidermis. While BCC is rarely life-threatening, accurate documentation and diagnosis are crucial for insurance reimbursement, epidemiological research, and treatment planning.
The medical coding system known as ICD-10 (International Classification of Diseases, Tenth Revision) provides a structured way to categorize and report diseases across healthcare settings. In the context of BCC, correct ICD-10 coding allows providers to:
- Document the anatomical location of the lesion
- Track recurrence and progression
- Link diagnosis with specific treatment plans
- Ensure compliance with billing standards
Introduction to ICD-10: Structure and Purpose
The ICD-10 system, maintained by the World Health Organization (WHO), is used globally for medical classification. It is alphanumeric, where each diagnosis is represented by a specific code starting with a letter followed by numbers.
The full format includes:
- Category (e.g., C44 for skin cancers)
- Etiology or anatomic detail (e.g., site of lesion)
- Severity or other clinical aspects (e.g., recurrence)
For basal cell carcinoma, the codes fall within C44: “Other and unspecified malignant neoplasm of skin.”
Here’s a basic layout in tabular form:
| ICD-10 Code | Description |
| C44.01 | BCC of lip |
| C44.11 | BCC of eyelid |
| C44.21 | BCC of ear |
| C44.31 | BCC of face |
| C44.41 | BCC of scalp/neck |
| C44.51 | BCC of trunk |
| C44.61 | BCC of upper limb |
| C44.71 | BCC of lower limb |
| C44.91 | BCC of unspecified site |
Sub-classification improves accuracy in clinical documentation and highlights nuances like laterality, recurrence, or uncertain behavior.
Coding Basal Cell Carcinoma by Anatomic Site
Each case of basal cell carcinoma must be coded not only by cancer type but also by its anatomic site. The ICD-10 system helps capture specific locations, which can influence treatment strategy.
For instance:
- BCC on the face (C44.31) may require more precise surgical intervention due to cosmetic and functional concerns.
- BCC on the trunk (C44.51) might allow for less aggressive excision techniques.
Understanding location-specific codes also impacts the assessment of recurrence risks, especially in previously irradiated or sun-exposed areas.
Consider this scenario:
A patient presents with a recurring lesion on the right cheek. The correct ICD-10 code would be:
- C44.312: Basal cell carcinoma of the skin of the right cheek
Such specificity assists in tracking long-term outcomes and identifying high-risk populations, especially when cross-referenced with comorbid conditions like bartholin gland cancer in immunocompromised patients.
How ICD-10 Codes Influence Treatment and Insurance
Treatment planning often relies on detailed diagnostic coding. For BCC, clinicians must identify not only the site but also:
- Whether the tumor is new or recurrent
- Whether it is in situ or invasive
- Whether it has unspecified behavior
This information drives:
- Preauthorization for surgical excision or Mohs micrographic surgery
- Insurance coverage for follow-up imaging or pathology
- Eligibility for certain high-cost medications or radiation therapy
In billing, vague or incorrect codes can lead to claim denials or delays in care. This is particularly problematic for older adults or patients managing multiple conditions.
Moreover, coding guides treatment pathways, such as whether Mohs surgery is indicated or whether radiation is justified in cases of recurrence.
This system is also useful when tracking broader trends across cancers. For instance, if BCC recurs near bile ducts or mucosal zones, cross-referencing with codes from bile duct cancer ICD-10 may reveal patterns worth investigating in multidisciplinary cancer boards.
Differences Between Basal Cell and Other Skin Cancers in ICD-10

Basal cell carcinoma (BCC) must be distinguished from other skin cancers in clinical documentation and coding. The ICD-10 system allows this through unique code categories:
- Basal cell carcinoma: C44.0–C44.9
- Squamous cell carcinoma: Often coded similarly but with separate morphology modifiers
- Melanoma: Covered under C43 category
Why this matters: each type behaves differently. BCC is slow-growing and rarely metastasizes, while squamous cell carcinoma and melanoma can be aggressive and life-threatening.
Accurate differentiation in the coding phase allows:
- Tailored clinical response
- Insurance policy alignment
- Better research insights
Comparative example:
| Cancer Type | ICD-10 Code | Behavior |
| Basal Cell | C44.31 | Locally invasive |
| Squamous Cell | C44.32 | Higher risk of metastasis |
| Melanoma | C43.31 | High metastatic potential |
By separating out BCC correctly in ICD-10 reports, registries can better track prevalence and guide funding toward non-melanoma skin cancer prevention. For more on squamous cell categorization, refer to our underlined and italicized guide on Basal Cell Skin Cancer ICD-10.
Documenting Recurrence and Multiple Tumors
BCC frequently recurs in the same or adjacent areas, especially after incomplete excision or radiation exposure. ICD-10 allows for this documentation through:
- D48.5 for tumors of uncertain behavior
- Use of Z85.828 for personal history of other skin neoplasms
- Modifier codes to indicate recurrence, laterality, or secondary malignancy
For example:
A patient with a second basal cell lesion on the same cheek, six months post excision, would require both:
- C44.312 (Right cheek BCC)
- Z85.828 (Personal history of skin cancer)
Properly coding recurrence helps in:
- Treatment reevaluation
- Insurance audit trails
- Research on resistance patterns
It also distinguishes between a metastatic lesion and a new primary site, which is critical in oncological care — especially for patients being monitored for other conditions like Bartholin Gland Cancer or internal malignancies.
ICD-10 Coding for Complications and Comorbidities
Some cases of basal cell carcinoma involve complications such as:
- Ulceration
- Bleeding
- Infection
- Involvement of bone or cartilage
To reflect the full clinical picture, providers should use ICD-10 combination codes or secondary codes. Examples include:
- L98.3: Necrobiosis and ulceration of skin
- C79.89: Secondary malignant neoplasm of other sites
- Z92.21: Personal history of antineoplastic chemotherapy
These codes help track how BCC interacts with other diseases and previous interventions. If a patient has previously undergone radiation or chemotherapy for another malignancy (e.g., bile duct cancer ICD-10), this could alter treatment thresholds or contraindications.
Clinical documentation should also include immunosuppression, especially in transplant patients or those with HIV/AIDS, where skin cancers can behave atypically.
How ICD-10 Enhances Epidemiology and Cancer Registries
Beyond billing and clinical application, ICD-10 codes are foundational for national cancer surveillance. Accurate and detailed coding of BCC helps government and academic researchers:
- Monitor incidence rates by age, race, and geography
- Identify occupational or environmental risks
- Track treatment outcomes and recurrence rates
For example, Medicare data coded with C44.31 (BCC of face) in Florida may show seasonal spikes, indicating sun exposure risk. These trends shape:
- Public health messaging (e.g., sunscreen campaigns)
- Funding allocations for research
- Targeted screening programs
More granular coding also supports clinical trials, especially when comparing treatments across demographics or comorbidity groups. This is increasingly important as newer therapies for BCC — like Hedgehog pathway inhibitors — enter clinical use.
In this way, ICD-10 supports not only the individual’s care path but also broad population health management, similarly to how Bartholin gland cancer and other rare conditions are tracked in global cancer databases.
ICD-10 and Anatomic Localization of Basal Cell Carcinoma
One of the most powerful features of the ICD-10 coding system is its ability to specify anatomic location of the tumor, which is critical in basal cell carcinoma (BCC) due to high recurrence risk in certain zones, especially the H-zone of the face (around the eyes, nose, and lips).
Key ICD-10 codes for location include:
- C44.31 – BCC of face
- C44.41 – BCC of scalp and neck
- C44.51 – BCC of trunk
- C44.61 – BCC of upper limbs, including shoulder
- C44.71 – BCC of lower limbs, including hip
Using the correct localization code supports:
- Accurate surgical planning
- Reimbursement for location-specific reconstruction
- Long-term tracking of tumor-prone zones
Clinical example:
A patient presenting with a pearly papule on the left temple is coded as C44.312 – Basal cell carcinoma of skin of left cheek, including temple.
This level of detail becomes essential when managing elderly patients or those with multiple comorbidities, where tumor location influences therapeutic risk. It also aligns with detailed protocols in dermato-oncology, just like those used in bile duct cancer ICD-10 classifications.
Coding Basal Cell Carcinoma in Immunocompromised Patients

Immunocompromised individuals, including organ transplant recipients and those undergoing chemotherapy, are at heightened risk of aggressive BCC variants. ICD-10 offers tools to reflect this:
- Z94.0–Z94.9: Transplanted organ status
- Z92.21: Personal history of antineoplastic chemotherapy
- D84.9: Immunodeficiency, unspecified
These modifiers guide treatment plans, for instance:
- More frequent follow-up schedules
- Increased use of Mohs surgery for margin control
- Expanded biopsy of suspicious adjacent areas
Such patients may also develop multiple skin cancers. If they have previously battled internal malignancies like Bartholin Gland Cancer, clinicians must balance systemic surveillance with aggressive local skin management.
Accurate ICD-10 documentation in these cases can also determine eligibility for specialty oncology programs, clinical trials, and pharmacy benefit approvals for advanced topical or systemic treatments.
Common Errors in Basal Cell ICD-10 Coding and How to Avoid Them
Missteps in coding basal cell carcinoma can lead to:
- Reimbursement denials
- Incomplete cancer registry data
- Misleading clinical documentation
Top errors include:
- Using a generic code like C44.9 (skin, unspecified) instead of specific site-based codes
- Omitting laterality (left/right) when required
- Failing to indicate recurrence or complications
Solutions:
- Always review documentation for laterality and recurrence
- Train billing teams in dermatologic ICD-10 usage
- Use templates in EHR systems to prompt correct code usage
Clinical Workflow Integration: From Dermatologist to Coder
Efficient ICD-10 documentation of BCC begins at the point of care. Dermatologists, Mohs surgeons, and oncologists must collaborate with coders and electronic health records (EHR) systems.
Recommended steps:
- Clinical note templates that capture:
- Lesion size and location
- Type of biopsy or excision
- Adjacent tissue involvement
- Automatic ICD-10 prompts within EHR for lesion laterality, depth, and behavior
- Post-surgical reports coded with:
- Initial diagnosis code (C44.x)
- Additional codes for reconstruction, complications, or grafting
- Follow-up scheduling paired with Z-codes like Z08 (follow-up for malignant neoplasm)
By aligning clinical documentation with ICD-10 precision, health systems can improve not only billing accuracy but also outcomes tracking, insurance negotiation, and multidisciplinary coordination.
This model also parallels best practices for complex cases in gynecologic oncology or hepatobiliary surgery — as seen in structured coding workflows for Bartholin Gland Cancer or bile duct cancer ICD-10 management.
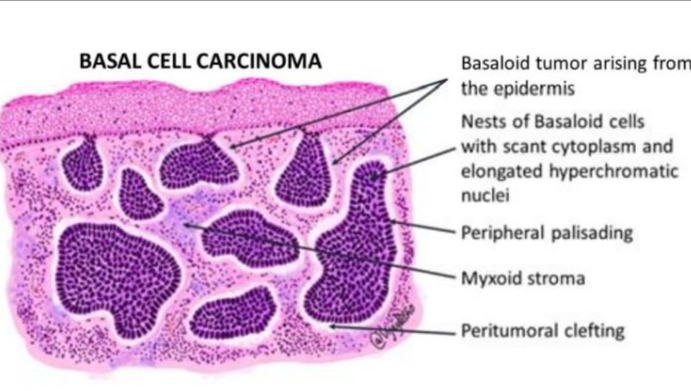
ICD-10 and Histological Subtypes of Basal Cell Carcinoma
Not all basal cell carcinomas behave the same. Histologic variants—such as morpheaform, infiltrative, micronodular, or superficial BCC—differ in aggressiveness, recurrence, and treatment difficulty. Unfortunately, ICD-10-CM does not always provide a separate code for these subtypes, but proper clinical documentation is still critical.
While C44.x codes cover anatomic and behavioral classification, pathology reports should specify:
- Subtype (e.g., morpheaform BCC)
- Margins (positive/negative)
- Depth of invasion
- Perineural involvement
This information, though not coded directly, significantly affects:
- Surgical planning (e.g., wider margins)
- Need for Mohs surgery vs standard excision
- Radiation or systemic therapy indications
In rare cases, advanced variants can show deeper invasion, similar to the infiltrative behavior of Bartholin Gland Cancer, reinforcing the need for coordinated pathology and clinical coding documentation.
ICD-10 for Recurrent or Multiple Basal Cell Carcinomas
Recurrent BCCs require a different approach in coding and documentation. Recurrent disease means the lesion has returned after previous treatment in the same or nearby area. While the ICD-10 system does not have a specific “recurrent” modifier for basal cell carcinoma, it’s essential to:
- Indicate recurrence clearly in clinical notes
- Use Z85.828 (Personal history of skin cancer) for past lesions
- Combine with new C44.x code for current active disease
For patients with multiple concurrent lesions, assign a separate code for each anatomic location. For example:
- C44.312 – BCC of left cheek
- C44.721 – BCC of right lower limb
Billing Tip: Ensure modifiers (e.g., 59 or XS in CPT) differentiate procedures on multiple sites to avoid denials.
Insurance, Billing, and Prior Authorization Challenges
Basal cell carcinoma may seem “routine” to insurers, but certain therapies (like hedgehog pathway inhibitors or advanced reconstructive surgery) often require prior authorization. ICD-10 codes play a decisive role in approval.
Insurers typically request:
- Precise site code (C44.x)
- Laterality (when applicable)
- Size or aggressive behavior documented in notes
- Failed prior treatments or contraindications to standard care
Coding combinations that aid insurance navigation:
| Clinical Situation | Code Combination Example |
| Recurrent facial BCC after surgery | C44.311 + Z85.828 |
| BCC in organ transplant patient | C44.312 + Z94.0 |
| Large aggressive scalp lesion needing Mohs | C44.411 + CPT for Mohs stages |
Pro tip: Denials for newer treatments can often be overturned with detailed ICD-10 codes linked to pathology-confirmed aggressive behavior.
Surveillance, Long-Term Tracking, and ICD-10 in Oncology Registries
While basal cell carcinoma is generally excluded from mandatory cancer registries due to its low metastatic risk, some subtypes or complex cases are increasingly included in research cohorts. ICD-10 enables tracking of patterns such as:
- Increasing BCC rates in younger adults
- High-risk zones (face, ears, scalp)
- Post-transplant skin cancers
Use of Z-codes like Z08 (Follow-up of malignant neoplasm) or Z85.828 ensures continuity of care. Documentation should emphasize:
- Site-specific recurrence (e.g., recurrent left nasal ala lesion)
- Changes in lesion size or growth rate
- Need for repeated biopsies or escalated treatments
These coding patterns mirror long-term monitoring approaches for serious conditions like basal cell skin cancer ICD-10 in transplant patients or patients with genetic syndromes (e.g., Gorlin syndrome).
Legal Implications and Coding Accuracy in Basal Cell Cancer
Accurate ICD-10 coding for basal cell carcinoma (BCC) is more than administrative—it’s a legal safeguard. Misclassification can lead to:
- Billing errors
- Insurance denials
- Medical liability in under-documented recurrences or aggressive subtypes
Common legal issues include:
- Assigning a generic code like C44.90 (unspecified skin site) instead of precise locations like C44.311 (left cheek)
- Failing to document multiple lesions with unique codes
- Misrepresenting excisional margins or pathology severity
In medico-legal investigations, coding data often serves as evidence of due diligence or, conversely, as proof of oversight. This is especially relevant in patients who later develop metastatic behavior, though rare in BCC, or when misdiagnosed lesions evolve into more dangerous cancers like Bartholin Gland Cancer.
ICD-10 in Telemedicine and Dermatologic Triage
With the rise of teledermatology, ICD-10 codes are integral to virtual triage and continuity of care. Providers now use high-definition images, patient history, and lesion monitoring tools to assign preliminary diagnoses and billing codes remotely.
Benefits of ICD-10 coding in teledermatology for BCC include:
- Remote assignment of location-specific codes (C44.x) for follow-up in-person biopsy
- Use of Z-codes like Z12.83 (Encounter for screening for skin cancer) during surveillance
- Integration with AI-based diagnostic tools that suggest code ranges based on photo analysis
Still, caution is necessary—overreliance on visuals without biopsy confirmation may lead to inaccurate use of malignant neoplasm codes. Providers should document disclaimers when using provisional coding via telemedicine.
Global ICD-10 Use for BCC Surveillance and Research
Though BCC rarely metastasizes, its overwhelming prevalence makes it a major public health concern. Global databases use ICD-10 to map:
- Incidence by country and climate
- Age trends in onset
- Correlation with UV exposure and tanning beds
WHO ICD-10 frameworks (and the newer ICD-11 transition) are being refined to capture:
| Aspect | ICD-10 (Current) | ICD-11 (Planned) |
| Lesion behavior | Limited (malignant only) | Includes premalignant codes |
| Histological subtype | Not captured | Proposed granularity |
| Recurrence history | Separate Z-codes | Integrated metadata |
This effort aligns with the kind of granularity now seen in tracking rarer diseases like bile duct cancer ICD-10, where nuanced behavior matters despite the low incidence rate.
Challenges in Documenting BCC with Coexisting Conditions
Many BCC patients—especially elderly individuals—have comorbidities like diabetes, immunosuppression, or anticoagulant use. ICD-10 coding must reflect this complexity:
- Use of combination codes, such as:
- C44.312 (BCC, left cheek) + Z94.0 (Organ transplant)
- C44.520 (BCC of trunk) + Z79.01 (Long-term anticoagulant use)
- Modifiers and secondary diagnosis fields ensure accurate risk stratification
- Documenting immunosuppression or transplant history is critical, as these patients may exhibit more aggressive skin cancers
Failing to capture comorbidity complexity may result in underestimation of risk, delayed intervention, or missed eligibility for advanced therapies.
Coding and Treatment Planning: Why ICD-10 Matters Clinically
ICD-10 codes for basal cell carcinoma are not just administrative—they directly influence treatment paths. For example:
- Precise lesion location codes (like C44.311 for left cheek) help surgeons plan excisions and determine cosmetic impact zones.
- Laterality inclusion ensures correct operative side in outpatient surgery reports.
- Multiple lesion coding allows billing and tracking of concurrent excisions (e.g., C44.310 + C44.521).
Accurate ICD-10 documentation also impacts:
- Radiation referrals (when surgery is contraindicated)
- Eligibility for topical therapies or Mohs micrographic surgery
- Inclusion in tumor registries or clinical audits
In many U.S. hospital systems, treatment approval algorithms are partially automated based on ICD-10 codes. Mislabeling a BCC can delay care or misguide therapy intensity.
When to Use Neoplasm Codes vs. Benign/Dysplastic Codes
BCC often starts as a suspicious lesion without definitive pathology. This raises the challenge: when to code as neoplasm of uncertain behavior (D48.5) versus confirmed malignant neoplasm (C44.x)?
| Scenario | Recommended Code | Reason |
| Lesion biopsied and confirmed BCC | C44.x series | Accurate malignancy |
| Lesion suspicious but not biopsied | D48.5 or R85.614 | Awaiting confirmation |
| Cosmetic removal, not suspicious | L57.0 or D23.x | Benign sun damage, not neoplastic |
This distinction matters for Medicare/Medicaid billing, audit risk, and long-term tracking. For instance, a misclassified lesion may later appear in basal cell skin cancer ICD-10 registries without true histological confirmation.
Transition from BCC to Other Skin Cancer Categories
Basal cell carcinoma is typically non-metastatic, but rare high-risk cases may show aggressive infiltration, especially in immunocompromised patients. Sometimes, a biopsy reveals:
- Mixed basal-squamous carcinoma
- Superficial BCC with perineural invasion
- Evolution into squamous cell carcinoma (SCC)
When this occurs, coders and clinicians must update from C44.3x (BCC codes) to appropriate SCC codes (C44.2x). Failing to reflect this change can:
- Misguide treatment escalation
- Confuse cancer registry data
- Lead to underreporting of high-risk cases
This coding migration is increasingly common in patients with multiple sun-related lesions. If you’re documenting this progression, also consider reviewing relevant codes used for Bartholin gland cancer, which requires equally specific anatomic and histologic mapping.
ICD-10 Codes and Insurance Claims: Denials and Appeals
Insurance companies use ICD-10 codes as justification for reimbursement. Even minor discrepancies in code precision can lead to:
- Claim denial for Mohs surgery
- Uncovered pathology charges
- Rejection of anesthesia billing
For example, billing Mohs surgery (CPT 17311) must be accompanied by a malignant skin cancer ICD-10 code (C44.x). Using a benign code like D23.9 (benign neoplasm) leads to automatic rejection.
What can help?
- Attaching pre-operative biopsy confirmation
- Including Z-codes like Z85.828 (personal history of skin cancer) if lesion is recurrent
- Submitting appeal letters that quote ICD-10 definitions and pathology data
Proper ICD-10 usage can prevent months of administrative delays and ensure patients receive care without financial hardship.
FAQ: Basal Cell Cancer ICD-10
1. What is the ICD-10 code for basal cell carcinoma of the nose?
The correct code is C44.311, indicating malignant neoplasm of the skin of the nose. Laterality and subsite-specificity are crucial for precise documentation.
2. Can one patient have multiple ICD-10 codes for basal cell cancer?
Yes. If the patient has BCC lesions on different anatomical sites, each site should be coded separately using the relevant C44.x code.
3. Is there a difference in coding for a suspected vs. confirmed basal cell carcinoma?
Yes. A confirmed diagnosis uses C44.x codes. If the lesion is suspected but not confirmed, D48.5 or R85.614 (for abnormal cytologic findings) may be appropriate.
4. What code should I use if the pathology report says “BCC in situ”?
You would use D04.x, which is the code series for carcinoma in situ of the skin, depending on location. It’s important to differentiate this from invasive BCC.
5. Are there ICD-10 codes for complications caused by basal cell cancer?
There are no specific complication codes tied to BCC, but related symptoms like ulceration or hemorrhage can be coded separately using symptom codes.
6. What is the ICD-10 code for recurrent basal cell carcinoma?
You still use the appropriate C44.x code, but can add Z85.828 (personal history of other malignant neoplasm of skin) to indicate recurrence.
7. Does the ICD-10 code change if the BCC is treated with Mohs surgery?
No, the ICD-10 diagnosis code remains the same. However, the CPT procedural code changes, which is what reflects Mohs treatment specifically.
8. Should I code actinic keratosis with BCC in the same visit?
Yes, if both are diagnosed, you may list L57.0 for actinic keratosis along with the C44.x code for BCC, as long as documentation supports it.
9. How do I code a BCC that was completely excised with clear margins?
Use the same C44.x code, and optionally include Z90.1x (acquired absence of other organs/tissue) if relevant. Coding should reflect diagnosis, not outcome.
10. Is there an ICD-10 code that indicates patient refusal of BCC treatment?
Yes. Use Z53.2 (procedure not carried out because of patient decision for other reasons) alongside the diagnosis code if the patient declines surgery or radiation.
11. Can I use ICD-10 codes for telemedicine skin cancer evaluations?
Yes, the diagnosis codes remain the same. Use modifier 95 for telehealth CPT codes, not the ICD-10.
12. Does skin grafting after BCC removal need a separate ICD-10 code?
Yes. Document the primary diagnosis (C44.x) and code the procedure (CPT or ICD-10-PCS for inpatient). The graft is not part of the cancer diagnosis code itself.
13. What if a biopsy reveals a different type of cancer than suspected BCC?
Update the ICD-10 code to reflect the new diagnosis, such as C44.22x for squamous cell carcinoma. This ensures proper tracking and treatment coverage.
14. Are ICD-10 codes used in cancer registries?
Yes. Basal cell carcinoma data is collected through ICD-10 codes but may be underreported in some registries due to its low mortality and high frequency.
15. What’s the ICD-10 code for basal cell carcinoma in bile duct or Bartholin gland?
Basal cell carcinoma rarely affects these areas. However, for related malignancies, see bile duct cancer ICD-10 or Bartholin gland cancer codes, which follow different anatomical coding conventions.












