Axillary Lump and Breast Cancer: What You Need to Know
- Understanding Axillary Lumps and Their Relationship to Breast Cancer
- Anatomy of the Axilla and Lymphatic Involvement
- Common Causes of Axillary Lumps: Beyond Breast Cancer
- How Breast Cancer Spreads to the Axillary Region
- Diagnostic Approach: From Physical Exam to Biopsy
- Role of Sentinel Lymph Node Biopsy and Axillary Dissection
- Treatment Options Based on Axillary Involvement
- Prognosis and Survival Rates in Cases with Axillary Node Involvement
- Imaging Techniques for Evaluating Axillary Lumps
- Hormone Receptor Status and Its Implications in Axillary Disease
- Managing Lymphedema After Axillary Surgery
- Psychosocial and Emotional Impact of Axillary Lumps and Breast Cancer
- Special Considerations in Male Breast Cancer with Axillary Involvement
- Axillary Lump Evaluation During Pregnancy and Lactation
- Clinical Pathways and Staging Guidelines
- Post-Treatment Surveillance and Long-Term Outlook
- Frequently Asked Questions (FAQ)

Understanding Axillary Lumps and Their Relationship to Breast Cancer
An axillary lump refers to a swelling, mass, or enlargement in the armpit area, medically known as the axilla. This region contains a dense network of lymph nodes, fatty tissue, nerves, and blood vessels. While many axillary lumps are benign—caused by infections, cysts, or reactive lymphadenopathy—some can be an early sign of breast cancer, particularly when cancer cells spread to the lymphatic system.
In breast cancer, malignant cells can migrate through the lymph channels to the axillary lymph nodes. The presence of such a lump may indicate local metastasis, which can impact staging, prognosis, and treatment decisions. Although not every axillary mass is cancerous, persistent, painless, or hard nodules—especially if fixed in place—warrant thorough medical investigation.
Understanding the nature of the lump involves clinical examination, imaging, and often biopsy. Because of its location and implications, an axillary lump must never be ignored, particularly in individuals with a personal or family history of breast cancer.
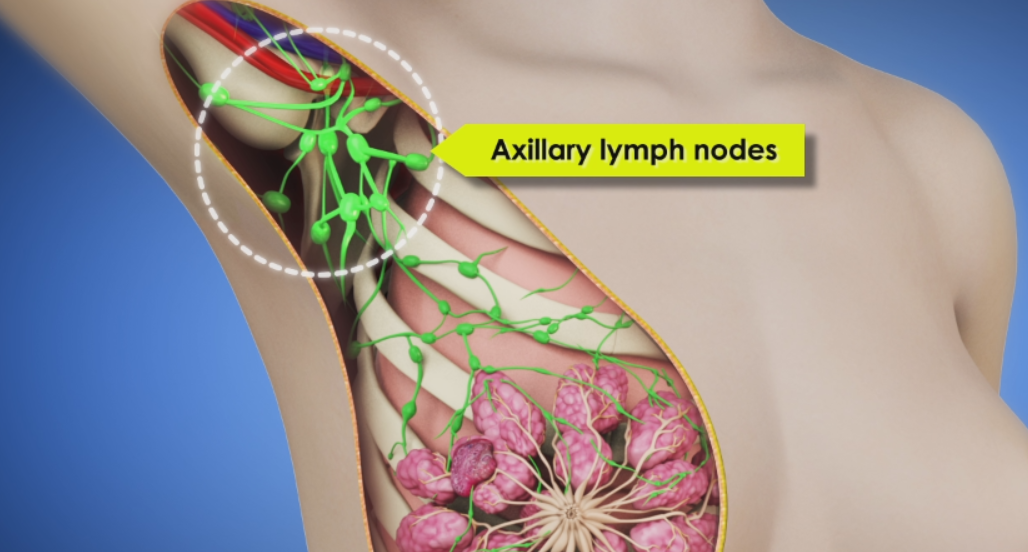
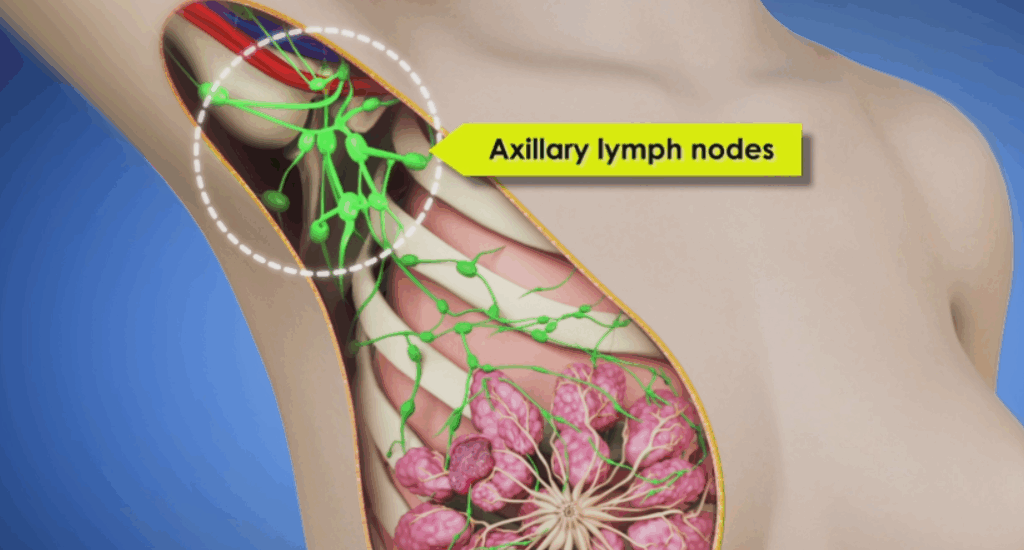
Anatomy of the Axilla and Lymphatic Involvement
To fully grasp the significance of axillary lumps in the context of breast cancer, it is important to understand the anatomy of the axilla. The axilla houses level I, II, and III lymph nodes, which act as filters for lymphatic fluid draining from the breast and upper limbs. When cancer cells invade the lymphatic system, they often reach these nodes first before spreading further.
Level I lymph nodes are located below the edge of the pectoralis minor muscle, Level II behind it, and Level III above it. Cancer that reaches Level II or III lymph nodes may be classified as more advanced, which can alter treatment strategy and prognosis. The axilla also contains adipose tissue, branches of the brachial plexus, and the axillary artery and vein—all of which may be affected by tumor growth or surgery.
Enlargement of lymph nodes in this area is not exclusive to cancer. It can occur with viral or bacterial infections, autoimmune diseases, or as a reaction to vaccines. However, in breast cancer, these nodes often become hard, non-tender, and immobile—features that distinguish them from inflammatory causes.
Common Causes of Axillary Lumps: Beyond Breast Cancer
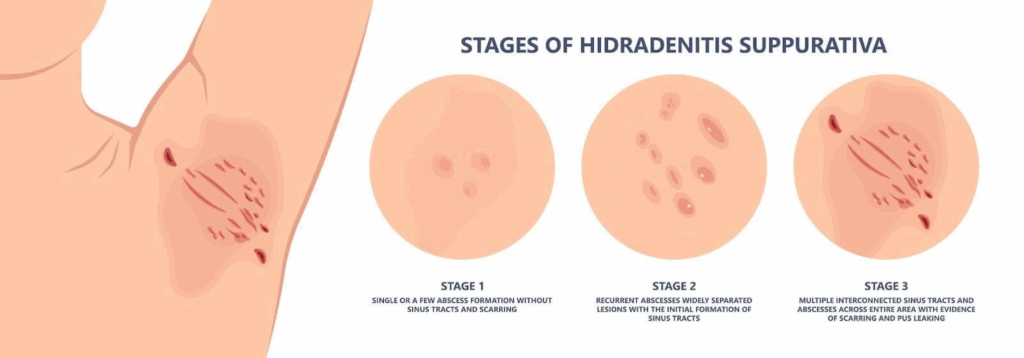
Although breast cancer is a major concern, not all axillary lumps signal malignancy. In fact, the most common causes include benign conditions such as reactive lymphadenopathy due to upper respiratory infections, localized skin infections (like folliculitis or hidradenitis suppurativa), or benign cysts. These lumps are often soft, tender, and fluctuate with inflammation.
Another frequent cause is lipomas, which are soft, movable, non-cancerous fatty tumors. While lipomas are harmless, they can mimic more serious masses and may require imaging to differentiate. Fibroadenomas, although more common in the breast tissue itself, can sometimes be palpated near the axillary tail of the breast.
In rare cases, axillary lumps may result from lymphoma, tuberculosis, or metastatic cancers from organs other than the breast. The key differentiating factor is whether the lump persists, grows, or changes in character. Persistent lumps should always prompt further evaluation, particularly in populations at risk for breast or lymphatic cancers.
How Breast Cancer Spreads to the Axillary Region
Breast cancer typically begins in the ductal or lobular cells of the breast and can spread in two primary ways: through the bloodstream or the lymphatic system. The latter is particularly relevant in the context of axillary involvement. Once malignant cells enter lymphatic vessels, they may travel to the axillary lymph nodes, which are the most common first site of regional spread.
In clinical practice, axillary lymph node involvement is considered a major staging and prognostic factor. A single cancerous node may shift a patient’s diagnosis from Stage I to Stage II or higher. This impacts treatment decisions, including the need for chemotherapy, radiation, or extended surgical intervention.
The spread to axillary nodes does not always produce palpable lumps in early stages. Sometimes, the involvement is microscopic and only discovered during sentinel lymph node biopsy. However, in more advanced or neglected cases, patients may present with visible swelling in the armpit, skin puckering, or associated breast changes. Androsteinedion aromatase inhibtor prostate cancer, особенно при обсуждении гормональной зависимости опухолей и ингибиторов ароматазы.
Diagnostic Approach: From Physical Exam to Biopsy
The diagnostic process for an axillary lump begins with a detailed clinical examination, during which a healthcare provider assesses the lump’s size, consistency, mobility, and tenderness. A firm, fixed, painless lump is more suspicious for malignancy than a soft, mobile, or tender one. The clinician will also examine the breast and other lymph node regions to evaluate for systemic signs of disease.
If cancer is suspected, imaging studies are the next step. Ultrasound is typically the first modality used due to its effectiveness in distinguishing solid from cystic masses. Mammography may be employed when a lump is related to breast pathology, especially in older patients. In ambiguous or high-risk cases, MRI provides greater detail of both breast and axillary tissue.
When imaging suggests malignancy or the lump does not resolve, a biopsy becomes essential. Fine needle aspiration (FNA), core needle biopsy, or excisional biopsy may be performed depending on the situation. The pathology report will reveal whether the cells are cancerous, and if so, what type of cancer is present. This histological confirmation guides the treatment plan.
Role of Sentinel Lymph Node Biopsy and Axillary Dissection
One of the most critical advances in breast cancer management is the development of sentinel lymph node biopsy (SLNB). The sentinel nodes are the first few lymph nodes into which a tumor drains. If these nodes are free of cancer, it’s likely that the rest of the nodes are also uninvolved. This procedure helps avoid the more invasive axillary lymph node dissection (ALND), which carries a higher risk of complications.
SLNB is usually performed during breast cancer surgery using a radioactive tracer and blue dye to identify the sentinel nodes. If cancer is found in these nodes, further axillary surgery may be needed. However, in some cases—particularly when only micrometastases are present—additional dissection may be avoided in favor of radiation or systemic therapy.
ALND involves removing many axillary nodes (typically Levels I and II) and is reserved for cases with confirmed node-positive disease. While effective, it can cause long-term side effects, including lymphedema, numbness, and limited shoulder mobility. Thus, modern practice aims to limit ALND when appropriate without compromising cancer control.
Treatment Options Based on Axillary Involvement
The presence or absence of axillary lymph node involvement significantly impacts the course of treatment. In early-stage breast cancer without nodal involvement, treatment may be limited to lumpectomy or mastectomy with or without radiation. However, when axillary nodes test positive for cancer, a more aggressive multimodal approach is usually required.
Radiation therapy is often used to treat the axillary region post-surgery, particularly when several nodes are involved or when ALND has been avoided. Systemic therapies—including chemotherapy, hormonal therapy, and targeted therapy—are also employed to address both local and distant disease. Hormone receptor-positive cancers respond to agents such as tamoxifen or aromatase inhibitors, while HER2-positive cancers may require trastuzumab.
The choice of treatment depends on tumor biology, stage, patient preferences, and overall health status. In all cases, a multidisciplinary team is essential to customize the approach and minimize overtreatment or long-term complications. Angiosarcoma breast cancer, discussing rare and aggressive types of breast tumors that may have an atypical course and require a different therapeutic strategy.
Prognosis and Survival Rates in Cases with Axillary Node Involvement
The prognosis for breast cancer varies widely depending on whether axillary lymph nodes are involved. When no nodes are affected, the 5-year survival rate exceeds 95% for most early-stage tumors. However, with increasing nodal involvement, the likelihood of recurrence rises, and long-term survival may decline.
Patients with 1–3 positive nodes typically fall into an intermediate-risk category, often treated with both local and systemic therapies. Those with 4 or more positive nodes are considered high-risk and require aggressive multimodal treatment. Still, even in these cases, outcomes have improved significantly due to advances in early detection and targeted therapies.
Survival also depends on tumor subtype. For instance, hormone receptor-positive cancers generally have a better outlook than triple-negative tumors, which are more likely to spread and recur. The response to treatment, overall health, and patient adherence to follow-up all influence the final prognosis.
While axillary involvement adds complexity, it does not equate to a poor outcome. With individualized care and close monitoring, many patients achieve long-term remission and excellent quality of life.
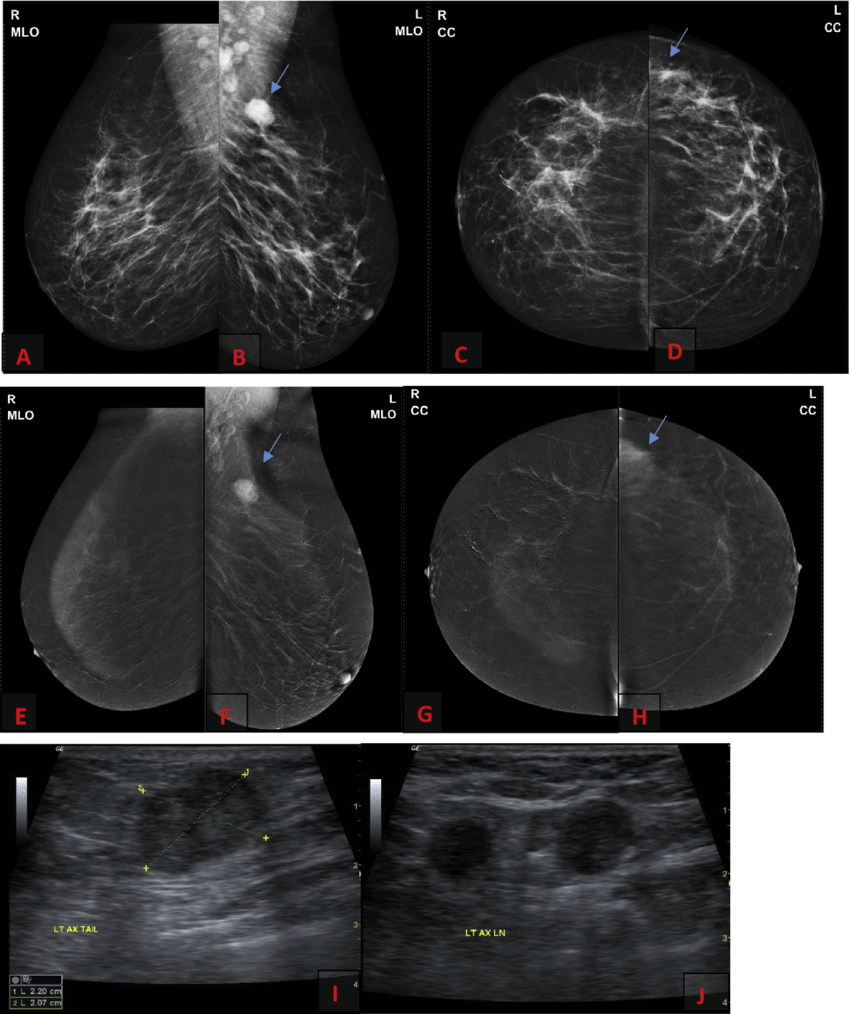
Imaging Techniques for Evaluating Axillary Lumps
Modern imaging plays a critical role in identifying and characterizing axillary lumps, especially when determining their relationship to breast pathology. Ultrasound is often the first-line modality due to its accessibility and sensitivity in distinguishing between cystic and solid masses. It allows visualization of the shape, margins, and vascular flow of the lump, which helps differentiate benign from malignant features.
Mammography is particularly useful in evaluating the breast when an axillary lump is discovered, especially in women over 40. It can detect microcalcifications or masses in the breast that correlate with lymph node involvement. When standard imaging is inconclusive, MRI provides detailed cross-sectional views of both the breast and axilla, and is especially beneficial in dense breast tissue or high-risk patients.
In cases of suspected metastasis or advanced disease, PET-CT or whole-body bone scans may be ordered to assess for distant spread. These functional imaging techniques help stage the disease and guide systemic treatment decisions. Proper imaging selection enhances diagnostic accuracy and reduces the need for unnecessary procedures.
Hormone Receptor Status and Its Implications in Axillary Disease
Understanding hormone receptor status is essential in all forms of breast cancer, particularly when axillary lymph node involvement is present. Tumors are tested for estrogen receptors (ER), progesterone receptors (PR), and HER2 (human epidermal growth factor receptor 2). These markers determine how the cancer may respond to specific treatments.
Hormone receptor-positive cancers often respond well to endocrine therapies, such as tamoxifen or aromatase inhibitors. These treatments help prevent recurrence by blocking the hormonal pathways that fuel tumor growth. Axillary node involvement in hormone-sensitive cancers typically prompts the addition of systemic hormonal therapy to address potential micrometastatic disease.
HER2-positive tumors, which are more aggressive, benefit from targeted therapies like trastuzumab or pertuzumab. For triple-negative breast cancer (lacking ER, PR, and HER2), treatment relies heavily on chemotherapy due to limited targeted options. Each of these profiles informs treatment plans, especially in patients with nodal disease, and is crucial for tailoring long-term management.
Managing Lymphedema After Axillary Surgery
Lymphedema is a common and often underrecognized complication following axillary lymph node removal or radiation. It occurs when lymphatic fluid accumulates in the arm, chest, or hand due to impaired drainage after surgery or radiation. The risk is higher in patients who undergo axillary lymph node dissection (ALND) or extensive nodal irradiation.
Symptoms of lymphedema include swelling, heaviness, tightness, and reduced range of motion in the affected limb. Without management, it can progress to chronic fibrosis, discomfort, and reduced quality of life. Prevention strategies include gentle range-of-motion exercises, avoiding trauma or infection to the arm, and early physical therapy intervention.
Once lymphedema develops, manual lymphatic drainage (MLD), compression garments, and specialized physiotherapy can help manage symptoms. Education on self-care and monitoring is vital, and in advanced cases, surgical lymphatic reconstruction may be considered. Managing lymphedema is an essential part of post-treatment survivorship care.
Psychosocial and Emotional Impact of Axillary Lumps and Breast Cancer
The discovery of an axillary lump and the subsequent diagnosis of breast cancer can be emotionally overwhelming. Anxiety often stems from uncertainty about the cause of the lump, potential cancer diagnosis, and fear of invasive tests or treatment. For many patients, the idea of cancer spreading to lymph nodes signals a loss of control or hope, even though treatment outcomes are often favorable.
Breast cancer affects not only physical health but also body image, sexuality, and identity, particularly when surgery or radiation involves the underarm or breast. Survivors may struggle with post-treatment fatigue, altered appearance, and emotional distress, all of which require compassionate and comprehensive support.
Psychological counseling, peer support groups, and open dialogue with the healthcare team can significantly ease the mental burden. Addressing emotional wellness is just as important as managing the physical aspects of the disease. Patients who feel heard and supported are more likely to engage in their care and maintain better long-term outcomes.
Special Considerations in Male Breast Cancer with Axillary Involvement
Although breast cancer is predominantly a disease of women, it can also affect men. Male breast cancer accounts for less than 1% of all breast cancer cases, but axillary lumps in men should never be dismissed. In many cases, a lump in the underarm is the first and only visible sign of malignancy, prompting further investigation into the breast tissue.
Men typically present at a later stage due to lack of awareness or delay in seeking medical attention. By the time cancer is detected, axillary lymph node involvement is often present. Most male breast cancers are hormone receptor-positive, making endocrine therapy an important part of treatment. However, because of anatomical differences, the disease may behave differently, and surgical management often includes mastectomy with axillary node evaluation.
Awareness campaigns and better education are helping improve early detection in men. When a male patient presents with a hard, painless axillary lump, especially with changes in the chest area, breast cancer should always be included in the differential diagnosis.
Axillary Lump Evaluation During Pregnancy and Lactation
Pregnancy and lactation create unique physiological changes in breast and axillary tissue. Hormonal shifts lead to increased glandular activity, which can cause reactive lymphadenopathy or benign lumps in the axilla. Despite this, any persistent or unusual lump must be evaluated carefully, as breast cancer can still occur during or shortly after pregnancy.
Imaging choices must consider fetal safety. Ultrasound is the preferred modality due to its safety and ability to differentiate cystic from solid lesions. Mammography may be used with abdominal shielding if necessary. If a suspicious mass is found, a core needle biopsy can be safely performed under local anesthesia, even during pregnancy.
Pregnancy-associated breast cancer tends to be more aggressive, partly due to delayed diagnosis. Early identification of axillary node involvement plays a critical role in staging and planning treatment, which often includes surgery and postpartum chemotherapy. A multidisciplinary team, including obstetricians and oncologists, is essential for optimal outcomes for both mother and child.
Clinical Pathways and Staging Guidelines
| Clinical Factor | Impact on Staging & Treatment |
| Presence of Axillary Lump | May suggest nodal involvement, raising the clinical stage |
| Confirmed Node Metastasis | Converts early-stage breast cancer to Stage II or III |
| Number of Positive Nodes | Determines need for chemotherapy, radiation, or further surgery |
| Hormone Receptor Status | Influences systemic therapy plan (e.g., endocrine therapy) |
| HER2 Status | Indicates suitability for targeted agents like trastuzumab |
| Tumor Size in Breast | Assessed alongside nodal spread to determine overall stage |
| Surgical Margins | May necessitate re-excision or mastectomy if unclear |
| Lymphovascular Invasion | Associated with higher risk of recurrence |
This table illustrates how multiple clinical variables interact in determining the appropriate treatment pathway and staging classification for breast cancer involving axillary nodes.
Post-Treatment Surveillance and Long-Term Outlook
After completing treatment, patients with axillary node involvement require ongoing surveillance to monitor for recurrence and manage side effects. Follow-up typically includes clinical breast exams every 3 to 6 months for the first 3 years, then annually. Imaging, such as mammograms and sometimes MRI, is conducted based on risk and prior treatment history.
Long-term outlook for these patients depends on multiple factors—extent of nodal involvement, tumor biology, response to treatment, and adherence to follow-up care. Recurrence risk is highest within the first five years, but with proper surveillance and healthy lifestyle choices, many patients remain disease-free long-term.
Survivorship care should also address lymphedema prevention, psychosocial recovery, hormonal therapy compliance, and management of menopausal symptoms or bone health, especially in those receiving endocrine treatment. The goal is to support not only survival but also a high quality of life.
Frequently Asked Questions (FAQ)
What does an axillary lump feel like in breast cancer?
In the context of breast cancer, an axillary lump is typically firm, painless, and immobile. It may feel like a small, hard node beneath the skin and can range in size. Unlike reactive lymph nodes, cancerous ones don’t usually cause tenderness or shrink over time.
Is every armpit lump a sign of breast cancer?
No, many axillary lumps are benign. They can result from infections, cysts, lipomas, or even skin irritation. However, any lump that persists for more than two weeks, grows, or feels hard should be evaluated by a healthcare provider.
Can an axillary lump be the first sign of breast cancer?
Yes, in some cases, an axillary lump may be the first noticeable sign of breast cancer—particularly when it represents a metastasis to the lymph nodes. This is why prompt evaluation is essential, even in the absence of a palpable breast mass.
What imaging tests are best for evaluating an axillary lump?
Ultrasound is often the first choice due to its effectiveness and safety. Mammography may follow if breast involvement is suspected. In complex or high-risk cases, MRI or PET-CT may be used for deeper visualization and staging.
Can men develop axillary lumps due to breast cancer?
Yes. Although rare, male breast cancer can present as an axillary lump. Because breast tissue in men is minimal, tumors often spread quickly to nearby lymph nodes, making awareness and timely evaluation important.
How is axillary lymph node involvement diagnosed?
Through a combination of clinical examination, imaging, and biopsy. Ultrasound-guided needle biopsy or core biopsy is the gold standard for confirming whether an axillary lymph node contains cancer cells.
What is the difference between sentinel node biopsy and axillary dissection?
Sentinel node biopsy is a targeted, minimally invasive procedure to sample the first draining lymph nodes. Axillary dissection is more extensive, involving removal of multiple nodes. The latter carries greater risk of complications like lymphedema.
How does hormone receptor status influence treatment of axillary node-positive cancer?
Hormone receptor status helps determine which systemic therapies will be effective. Hormone-positive cancers often respond to tamoxifen or aromatase inhibitors, which are essential for reducing recurrence in node-positive cases.
Is lymphedema permanent?
Lymphedema can become chronic if untreated, but with early detection and proper management—such as physical therapy and compression—it can often be controlled and minimized over time.
Can you have breast cancer without a breast lump?
Yes. Some patients present with only axillary swelling or subtle breast changes such as nipple inversion, skin dimpling, or pain. That’s why full diagnostic workup is essential when any suspicious symptom appears.
What happens after a positive axillary biopsy?
A positive biopsy typically leads to breast imaging (if not already done), full cancer staging, and multidisciplinary treatment planning. This may involve surgery, radiation, and systemic therapy depending on the extent of disease.
Do axillary lumps always require biopsy?
Not always. If the lump is clearly benign on imaging and resolves on follow-up, biopsy may not be needed. But in persistent, suspicious, or unexplained cases, tissue sampling is crucial for diagnosis.
axillary
Yes. Breastfeeding can cause reactive lymph nodes or benign breast tissue changes in the axilla due to increased milk production. However, persistent or unusual lumps during lactation still require medical evaluation.
What’s the prognosis for breast cancer with node involvement?
Prognosis varies. One to three positive nodes suggest intermediate risk, while four or more indicate higher risk. Modern treatments have greatly improved survival even in node-positive cases, especially with early intervention.
Are there any parallels between axillary lumps and other cancers?
Yes. Lymphatic involvement is a hallmark of many cancers. For example, prostate cancer and certain rare breast cancers like angiosarcoma can also present with nodal spread. Prostate cancer screening and Angiosarcoma breast cancer as examples of different metastasis scenarios.