Autism in 2025: Advances, Challenges, and Future Directions
Understanding Autism Spectrum Disorder (ASD): What Are We Talking About?
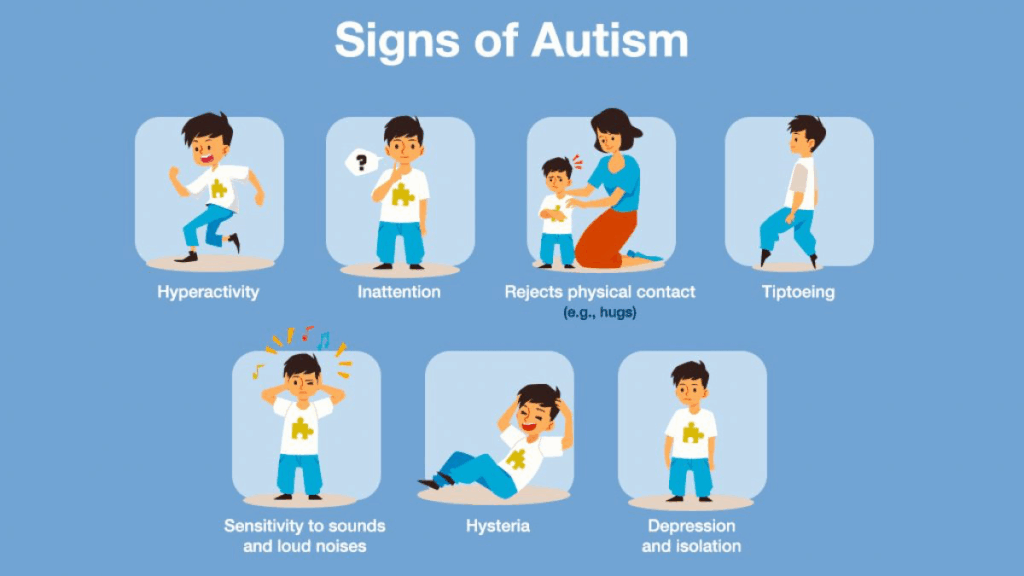
Have you ever wondered what exactly autism is? You might have heard the term thrown around, maybe even met someone diagnosed with it, but what does it really mean? Autism Spectrum Disorder (ASD) is not a single condition but a broad range of neurodevelopmental differences that affect how a person perceives the world, communicates, and interacts socially. The “spectrum” part means it’s incredibly diverse—two people with ASD might share some traits but be vastly different in others. Some individuals may have significant challenges with communication or behavior, while others might excel in areas like memory or pattern recognition.

Autism isn’t just a niche medical curiosity; it’s a global phenomenon. Estimates suggest that roughly 1 in 36 children worldwide is diagnosed with ASD, though this varies widely depending on location, diagnostic criteria, and awareness. That means autism impacts millions of people and their families, creating profound ripple effects in education, healthcare, employment, and society at large. In that way, autism shares something in common with larger-scale global health challenges—like those discussed in our analysis of Disease X—where understanding patterns and systems becomes key to shaping better futures.
Why Should We Care About Autism—Historically and Today?
Autism might seem like a “modern” diagnosis, but its recognition has a surprisingly recent history. It was first clinically described in the 1940s, which isn’t long ago in the grand scheme of medicine. For decades, understanding of autism was limited and often misunderstood. Early theories ranged from blaming parenting styles to seeing it as a rare psychiatric disorder. Thankfully, science and compassion have moved forward together since then.
Today, autism sits at the crossroads of multiple fields: neuroscience, psychology, genetics, education, and social policy. Why? Because autism challenges us to rethink what “normal” means in human development and communication. It asks society to build inclusion and support systems that recognize the value and dignity of all neurological profiles.
Thinking back to history helps us appreciate how far we’ve come—and also highlights the gaps we still face. For example, diagnostic tools have evolved from simple behavioral observations to sophisticated assessments incorporating genetics and even artificial intelligence. In fact, the broader field of diagnostics is undergoing a renaissance. Just as complete blood counts (CBCs) are being reimagined as tools for early cancer detection, our methods for identifying autism are growing more refined and predictive with each passing year.
What’s Coming Up in This Journey Through Autism in 2025?
In this series, we’ll explore the many layers of autism’s reality today and what the future might hold. We’ll look at who is diagnosed and why, what we know about the complex genetics and environment factors at play, and how cutting-edge technology is transforming diagnosis and treatment. We’ll also address the real-world systems that support individuals and families, recognizing that no medical advance alone can replace compassion and community.
We want to keep this conversation open and accessible. So whether you’re a parent, educator, healthcare worker, or just curious, feel free to ask questions and reflect on your own experiences with autism. What surprises you? What challenges do you see in your community? This isn’t just about science—it’s about humanity.
Epidemiology: Unraveling the Patterns of Autism Around the World
Understanding how common autism is and who it affects is fundamental to shaping the right supports and policies. Epidemiology—the study of disease patterns in populations—gives us this insight, but when it comes to autism, the picture is anything but straightforward.
Worldwide estimates suggest that approximately 1 in 36 children is diagnosed with autism in certain countries, such as the United States. Yet, these numbers vary significantly across regions, reflecting more than just biological realities. Diagnostic criteria, cultural attitudes, healthcare infrastructure, and awareness all shape who gets identified as autistic.
For example, in some countries, autism diagnoses remain rare, not necessarily because autism is less common, but because access to specialists or developmental screenings is limited. Social stigma and differing cultural interpretations of behavior can also delay or prevent diagnosis. This means that global autism prevalence data must be interpreted with care—underdiagnosis is a significant challenge, especially in low-resource settings.
The story gets more intricate when we consider demographics. Autism has historically been diagnosed more frequently in boys, with reported ratios of about four boys to every girl. However, this gap is narrowing as researchers uncover how autism manifests differently in females. Girls often exhibit more subtle social difficulties or better compensation skills, which have led to many being overlooked or misdiagnosed for years. This evolving understanding has profound implications, reminding us that our diagnostic tools and social expectations can unintentionally bias who gets recognized and supported.
Socioeconomic factors further complicate the landscape. Families with greater access to healthcare and education tend to have higher diagnosis rates, suggesting that autism exists across all social strata but is more readily identified where resources and knowledge are abundant. This disparity calls for ongoing efforts to improve equity in diagnosis and care.
Beyond diagnosis rates, epidemiology also fuels important debates about why autism prevalence appears to be rising. Some of this increase is undoubtedly due to broader diagnostic criteria, improved awareness, and more systematic screening programs. Yet, scientists continue to investigate environmental and biological contributors that might be influencing real changes in incidence. Factors such as parental age, prenatal exposures, and environmental pollutants are under intense scrutiny, though no single cause has been isolated.
Why do these numbers matter so much? They guide everything from education planning to healthcare resource allocation and social policy. When we know how many people are on the autism spectrum—and where they are—we can better tailor services and supports that meet their unique needs.
Epidemiology reminds us that autism is not a static statistic but a dynamic part of our societies. It pushes us to improve detection while addressing the inequalities that leave many individuals and families without the understanding and support they deserve. It also challenges us to remain curious and compassionate, recognizing the diversity and complexity behind the numbers.
Genetic and Environmental Factors: Piecing Together the Puzzle of Autism
When it comes to understanding why autism occurs, the story is intricate and multifaceted. It’s not a simple matter of “one cause,” but rather a complex interplay between genetics and environment, each contributing pieces to the overall puzzle.
Decades of research have established that genetics play a major role in autism. Studies of twins and families show that autism is highly heritable—meaning that genes contribute significantly to a person’s likelihood of being on the spectrum. However, unlike traits such as eye color or blood type, autism is not linked to a single gene. Instead, it involves many genes, often working together in complex ways. Hundreds of genetic variants have been identified that may increase susceptibility, some common and subtle, others rare but with strong effects.

This genetic diversity helps explain why autism manifests so differently from one person to another. It’s like an elaborate recipe with many ingredients, each adding a unique flavor. For some individuals, a particular genetic mutation may be a key driver, while for others, it’s a combination of multiple genetic factors acting in concert.
But genetics is only one side of the story. Environmental factors, particularly those influencing brain development before and shortly after birth, also play an essential role. These can include prenatal exposures like maternal infections, certain medications, environmental pollutants, or even parental age at conception. These factors don’t act in isolation; instead, they interact with a person’s genetic makeup, influencing how genes are expressed or how the brain develops.
This gene-environment interplay is vital to grasp because it shifts the narrative away from deterministic views of autism. It suggests that while genetic predispositions set the stage, the environment can shape the unfolding of traits in profound ways. This also means there is hope for interventions that optimize environments to support neurodevelopment.
Understanding these relationships is a challenge. Scientists continue to probe which environmental factors matter most, at what points during development they exert influence, and how exactly they interact with genetic risk. Some research focuses on identifying biomarkers—biological indicators—that could signal increased likelihood of autism before behaviors emerge, opening doors to earlier support.
Importantly, this nuanced view helps dispel myths that oversimplify autism’s origins or blame parents unfairly. Instead, it promotes a compassionate understanding grounded in science, recognizing the complexity of human development and the diversity of pathways leading to autism.
Looking ahead, this knowledge could pave the way for personalized approaches in healthcare and education, where supports and interventions are tailored to the unique genetic and environmental profiles of each individual. It also highlights the importance of public health measures that minimize harmful exposures during critical periods of brain development.
Diagnostic Criteria and Tools: Navigating the Complex Path to an Autism Diagnosis
Diagnosing autism today is both an art and a science. Unlike some medical conditions that can be confirmed with a blood test or an X-ray, autism diagnosis relies largely on careful observation of behavior and detailed developmental history. Professionals use standards like the DSM-5, which outlines criteria focusing on social communication challenges and repetitive behaviors, but the reality is far more nuanced.
Each individual with autism presents a unique profile. For some, the signs are evident early in childhood: difficulties with eye contact, trouble understanding social cues, or intense focus on specific interests. For others, especially older children or adults, these signs may be more subtle or masked by learned coping strategies, making diagnosis more complex.
In recent years, technology has started to complement traditional diagnostic approaches. Eye-tracking devices, brain imaging, and voice analysis are opening new doors, offering more objective data to support clinical judgment. Artificial intelligence (AI), in particular, shows promise for enhancing early detection by analyzing patterns in behavior or physiological data that humans might miss.
This technological leap is especially exciting because early diagnosis can lead to earlier intervention, which is often linked to better developmental outcomes. Yet, these advancements also come with challenges. AI tools must be carefully validated to ensure they work fairly across diverse populations and don’t inadvertently reinforce biases.
Access remains a critical issue. Many families still face long waits or travel significant distances to see specialists. This highlights the need for more accessible, affordable, and culturally sensitive diagnostic services—something that emerging digital tools and telehealth might help address in the near future.
Ultimately, autism diagnosis is more than just a clinical label. It’s a gateway to understanding, support, and resources tailored to each individual’s needs. The future holds promise for more precise, personalized diagnostics that respect the diversity of the autism spectrum while opening new paths for care and inclusion.
Intervention Strategies: Supporting Individuals with Autism Through Therapies and Treatments
Once a diagnosis is made, the focus naturally shifts toward intervention—how to support individuals with autism in thriving according to their unique needs and strengths. The approaches to intervention have evolved significantly over the years, moving beyond one-size-fits-all models toward more personalized, flexible strategies. By 2025, this evolution continues, blending established behavioral methods with emerging pharmacological treatments and an increasing emphasis on holistic well-being.
The backbone of autism intervention remains behavioral therapies, which aim to improve social communication skills, reduce challenging behaviors, and enhance adaptive functioning. Applied Behavior Analysis (ABA) has been a cornerstone of this field for decades. It uses principles of learning theory to reinforce desired behaviors and reduce those that interfere with learning or daily life. ABA programs are highly individualized, often intensive, and can be adapted to suit different ages and abilities.
However, the field has grown more nuanced. There’s recognition that rigid, highly structured interventions may not fit everyone’s needs or values, leading to the development of more naturalistic and relationship-based approaches. Methods like the Early Start Denver Model or Developmental, Individual Difference, Relationship-Based (DIR) therapy focus on engaging children through play and interaction, respecting their interests and emotional states. This shift reflects a broader cultural understanding of autism, emphasizing acceptance and collaboration rather than correction.
Educational interventions are also vital. Many children on the spectrum benefit from specialized schooling environments or inclusive classrooms with tailored supports. These educational strategies focus not only on academic skills but also on social integration, communication, and self-advocacy. Supporting executive functioning—skills like planning, organization, and flexible thinking—is increasingly recognized as essential for lifelong success.
Pharmacological treatments are a different, sometimes controversial, aspect of autism intervention. No medication “cures” autism, but some can help manage co-occurring symptoms such as anxiety, attention difficulties, or irritability. Advances in neuroscience are gradually improving our understanding of how certain medications might target underlying neurochemical imbalances, offering more tailored and effective options. Yet, medication use must always be carefully weighed against potential side effects, and integrated into a broader therapeutic plan.
In 2025, there’s also growing interest in novel therapies, including nutritional interventions, sensory integration therapies, and even technology-assisted methods like virtual reality or robot-assisted social skills training. While some of these approaches show promise, rigorous scientific evaluation remains essential to separate effective treatments from those lacking evidence.
Crucially, intervention is not solely about the individual. Family involvement and support play an indispensable role. Caregivers often serve as primary coaches and advocates, making family-centered approaches a priority in contemporary practice. Supporting families with education, respite services, and counseling reduces stress and improves outcomes for everyone involved.
Ultimately, successful intervention respects the diversity of the autism spectrum. It focuses on enhancing quality of life—helping individuals build meaningful relationships, pursue their interests, and participate fully in their communities. It’s a long-term journey, requiring flexibility, patience, and above all, a commitment to seeing each person as whole and capable.
Support Systems and Services: Building a Network Around Individuals with Autism
Diagnosis and intervention are critical steps, but they’re only part of the broader picture. For individuals with autism to truly thrive, a robust network of support systems and services is essential. By 2025, the landscape of support has become more varied and sophisticated, yet challenges around accessibility and equity remain central concerns.
When we talk about support systems, we mean everything from early intervention programs and specialized education to vocational training, mental health services, and community-based resources. These supports are designed to help individuals navigate daily life, build independence, and engage meaningfully with their families, peers, and communities.
One of the most important pillars is early intervention services, which provide therapeutic and educational supports in the crucial developmental years. These programs often combine speech therapy, occupational therapy, and social skills training tailored to the child’s needs. Early, coordinated care can have a lasting impact, helping children build foundational skills that influence their trajectories throughout life.
As children grow, educational systems take center stage. Inclusive classrooms with individualized education plans (IEPs) aim to balance access to mainstream learning with necessary accommodations. Yet, the quality and availability of these services vary widely depending on geography, funding, and policy. For many families, navigating the education system can be a daunting challenge, requiring advocacy and persistence.
Support doesn’t end with childhood. Adult services—often overlooked—are gaining attention as more individuals on the spectrum reach adulthood. These programs focus on job training, independent living skills, social engagement, and mental health support. Employment support services are especially vital, helping bridge the gap between capability and opportunity, addressing the stark reality that many autistic adults face unemployment or underemployment despite their talents.
Government programs and community organizations play a crucial role in creating these supports, but their reach and effectiveness vary. In some countries, national policies provide comprehensive frameworks and funding for autism services, while in others, families must rely on patchy or informal networks. Advocacy groups continue to push for more inclusive, rights-based approaches that recognize autism as a natural variation rather than a deficit.
Technology has also begun to transform support services. Telehealth platforms make therapy more accessible, especially in rural or underserved areas. Apps and devices assist with communication, organization, and social skills development. Virtual support groups offer connection and peer mentoring that can reduce isolation.
Despite these advances, significant barriers remain. Long waitlists, high costs, and uneven quality create gaps that leave many without needed services. Cultural and language differences, as well as stigma, can further limit access. Addressing these disparities is a major focus for policymakers and service providers moving forward.
At its heart, a strong support system recognizes that autism affects the whole person and their community. It values collaboration among families, professionals, educators, and individuals themselves. It prioritizes empowerment, respect, and the dignity of choice.
Recent Developments (2025–2026): Breaking New Ground in Autism Research and Care
As we find ourselves in 2025, the landscape of autism research and care is buzzing with fresh discoveries, innovative technologies, and shifting policies that together are reshaping what’s possible for individuals on the spectrum.
One of the most exciting frontiers is in early detection. Advances in neuroimaging and machine learning have brought us closer to identifying subtle markers of autism in infants as young as six months. This early window is critical because it opens the door to interventions at a stage when the brain is most adaptable. Several new studies have demonstrated promising results in refining these predictive models, combining behavioral data with genetic and physiological indicators. These tools could revolutionize how pediatricians screen for autism, making early diagnosis more accurate and widely available.
On the therapeutic front, there’s growing momentum toward personalized interventions. Thanks to deeper genetic insights and the integration of big data analytics, clinicians are beginning to tailor therapies not only to observable behaviors but also to the underlying biology of each individual. This shift moves us beyond the “one-size-fits-all” model, aiming to maximize the effectiveness of treatments by aligning them with unique profiles.
Technology continues to expand its role in supporting individuals with autism. Virtual reality (VR) programs are being piloted to help build social skills and emotional regulation in safe, controlled environments. Robotics and AI-driven coaching tools offer interactive learning experiences, providing consistent practice with social scenarios or daily living skills. These innovations are especially promising for those who face barriers to traditional therapy due to geographic isolation or resource limitations.
Policy-wise, several countries have introduced or refined legislation to improve access to autism services and protect the rights of autistic individuals. The emphasis on neurodiversity and inclusion is stronger than ever, influencing education, employment, and healthcare practices. Public awareness campaigns have shifted focus from just understanding autism to celebrating strengths and promoting societal acceptance.
Yet, as the pace of progress accelerates, new challenges arise. Ethical questions around genetic testing, data privacy, and equitable access to advanced diagnostics and therapies demand careful navigation. The autism community—individuals, families, advocates, and professionals—continues to engage in important conversations about how to balance innovation with respect for autonomy and diversity.
In sum, recent developments paint a picture of hopeful possibility. The combination of scientific breakthroughs, technological tools, and evolving social attitudes is steadily expanding opportunities for earlier diagnosis, more personalized support, and fuller inclusion. The journey is far from over, but 2025 marks a dynamic moment of transformation in autism research and care.
Future Directions: Charting the Path Forward for Autism in 2025 and Beyond
Looking ahead, the future of autism research and support is both inspiring and complex. As we stand at this crossroads, several promising directions and important challenges come into focus—each shaping how individuals on the spectrum and their communities will experience life in the years to come.
One major area ripe for advancement is personalized medicine. The growing understanding of autism’s genetic and biological diversity suggests that tailoring interventions to individual profiles will become the norm rather than the exception. Imagine a future where therapies are not just based on observed behaviors but guided by precise genetic, neurological, and environmental data. This could dramatically improve outcomes and reduce trial-and-error in finding effective supports.
Technology will continue to be a powerful catalyst. Artificial intelligence, wearable devices, and virtual reality are poised to provide real-time support and monitoring, helping individuals manage sensory sensitivities, communicate more effectively, or navigate social environments with greater confidence. Such tools might also facilitate more seamless collaboration between clinicians, educators, and families, creating holistic support networks.
However, these technological advancements must be balanced with ethical considerations. Issues of privacy, data security, and informed consent are paramount, especially when dealing with vulnerable populations. Ensuring equitable access is also critical; the benefits of new tools should not be limited to those with financial means or living in well-resourced areas.
Beyond the clinic and lab, future directions emphasize societal change. Efforts to build inclusive communities where neurodiversity is celebrated will continue to gain momentum. This means transforming education systems, workplaces, and public spaces to accommodate different ways of thinking and interacting. Policies must evolve to protect rights while promoting opportunity, recognizing that true inclusion benefits everyone.
Research will also delve deeper into understanding autism across the lifespan. While much focus has traditionally been on early childhood, the needs of autistic adults are becoming a central concern. Aging, mental health, and quality of life in later years are areas demanding more attention and tailored supports.
Ultimately, the future calls for a holistic vision—one that integrates cutting-edge science, compassionate care, and social justice. It’s about creating environments where autistic individuals can flourish on their own terms, with dignity and full participation in society.
The path forward won’t be without obstacles, but with collaboration across disciplines and communities, the potential to improve lives and deepen understanding is immense.
Frequently Asked Questions About Autism in 2025
1. What exactly is Autism Spectrum Disorder (ASD)?
ASD is a neurodevelopmental condition characterized by differences in social communication and repetitive behaviors. It’s called a “spectrum” because it includes a wide range of experiences and abilities, from people who require significant support to those who live independently and excel in many areas.
2. Why are autism diagnosis rates increasing?
The rise in diagnosis is largely due to improved awareness, broader diagnostic criteria, and better access to screening. While research continues into possible environmental or biological factors, much of the increase reflects a greater ability to recognize and understand autism.
3. How much do genetics influence autism?
Genetics play a major role, with heritability estimates ranging from 50 to 90 percent. However, autism is influenced by many genes interacting with environmental factors, so it’s a complex genetic landscape rather than a single gene cause.
4. Can autism be diagnosed early?
Yes, advances in behavioral assessments and technology—including AI and neuroimaging—are enabling diagnosis in infancy or toddlerhood. Early diagnosis is crucial for starting interventions during key developmental windows.
5. What are the main types of intervention for autism?
Interventions include behavioral therapies like ABA, educational supports, speech and occupational therapy, and sometimes medication to manage co-occurring symptoms. Approaches are increasingly personalized and may incorporate new technologies.
6. How do support systems help individuals with autism?
Support systems provide therapy, education, social skills training, employment assistance, and family support. These services help individuals navigate life’s challenges, build independence, and engage with their communities.
7. What role does technology play in autism care?
Technology—from AI-assisted diagnosis to virtual reality and communication apps—is transforming how autism is identified and supported. It offers new possibilities for accessibility, personalization, and engagement.
8. What challenges remain in autism diagnosis and care?
Barriers include disparities in access, cultural and language differences, potential biases in diagnostic tools, and the need for services across the lifespan, especially for adults.
9. How is society changing in its approach to autism?
There’s a growing emphasis on neurodiversity, inclusion, and rights-based approaches. Policies and attitudes are shifting to celebrate differences rather than focusing solely on deficits.
10. What does the future hold for autism research and support?
The future points toward more personalized medicine, technology integration, inclusive communities, and greater attention to autistic adults’ needs, all balanced with ethical considerations and equitable access.
Conclusion: Embracing Complexity and Possibility in Autism’s Evolving Story
Autism in 2025 is a story of progress, challenges, and hope. Our understanding of autism’s roots in genetics and environment continues to deepen, revealing a tapestry of influences that shape each individual uniquely. Diagnostic tools are becoming more sophisticated, blending clinical expertise with innovative technology to identify autism earlier and more accurately than ever before.
Intervention strategies have grown more personalized and diverse, reflecting a broader cultural shift toward acceptance and empowerment. Support systems strive to meet individuals where they are, yet gaps and inequalities remind us that much work remains. Recent scientific advances and policy changes provide reason for optimism, while ongoing conversations around ethics, inclusion, and diversity ensure that progress is thoughtful and humane.
Looking forward, the promise lies in integrating science, technology, and social change to build environments where autistic people can flourish—not in spite of their differences, but because of them. As we continue this journey, empathy, curiosity, and collaboration will be our greatest guides, shaping a future where every person on the spectrum is seen, supported, and celebrated.










