ATM Mutation and Breast Cancer
ATM Mutation and Breast Cancer: A Complete Beginner’s Guide
- What Is the ATM Gene and Why It Matters in Breast Cancer
- How ATM Mutations Increase Breast Cancer Risk
- Symptoms of Breast Cancer in People With ATM Mutation
- How ATM Mutations Compare to BRCA1 and BRCA2
- How to Get Tested for ATM Mutations
- What a Positive ATM Mutation Test Means for You
- ATM Mutation and Other Associated Cancers
- Treatment Planning for Breast Cancer Patients With ATM Mutation
- Should Family Members Get Tested for ATM Mutations?
- Screening Guidelines for ATM Mutation Carriers
- Psychological and Ethical Considerations of ATM Genetic Testing
- Latest Research on ATM and Breast Cancer Therapies
- Lifestyle and Risk Reduction for ATM Carriers
- Insurance and Financial Considerations for Genetic Carriers
- Differences in Management by Age or Gender
- Advocacy and Support Resources for ATM Mutation Carriers
- FAQ – ATM Mutation & Breast Cancer
What Is the ATM Gene and Why It Matters in Breast Cancer
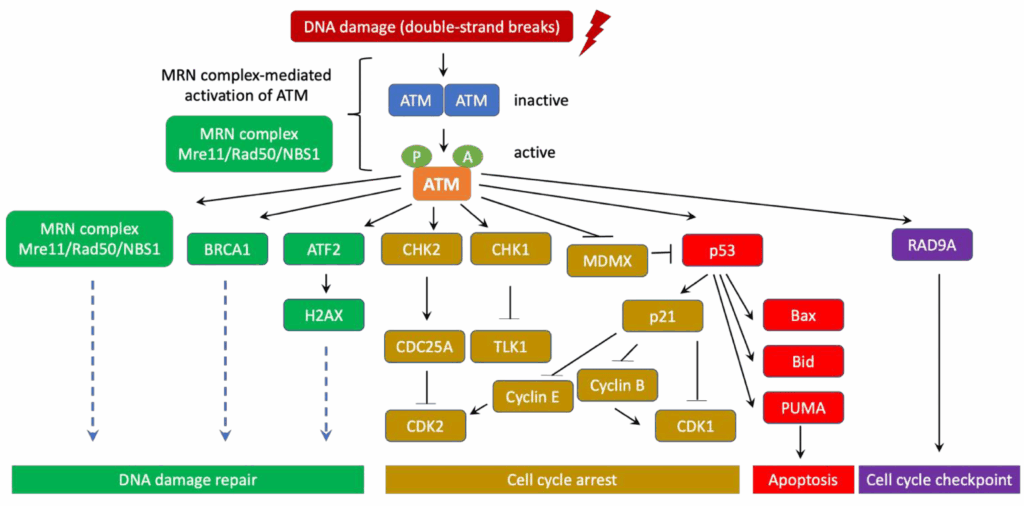
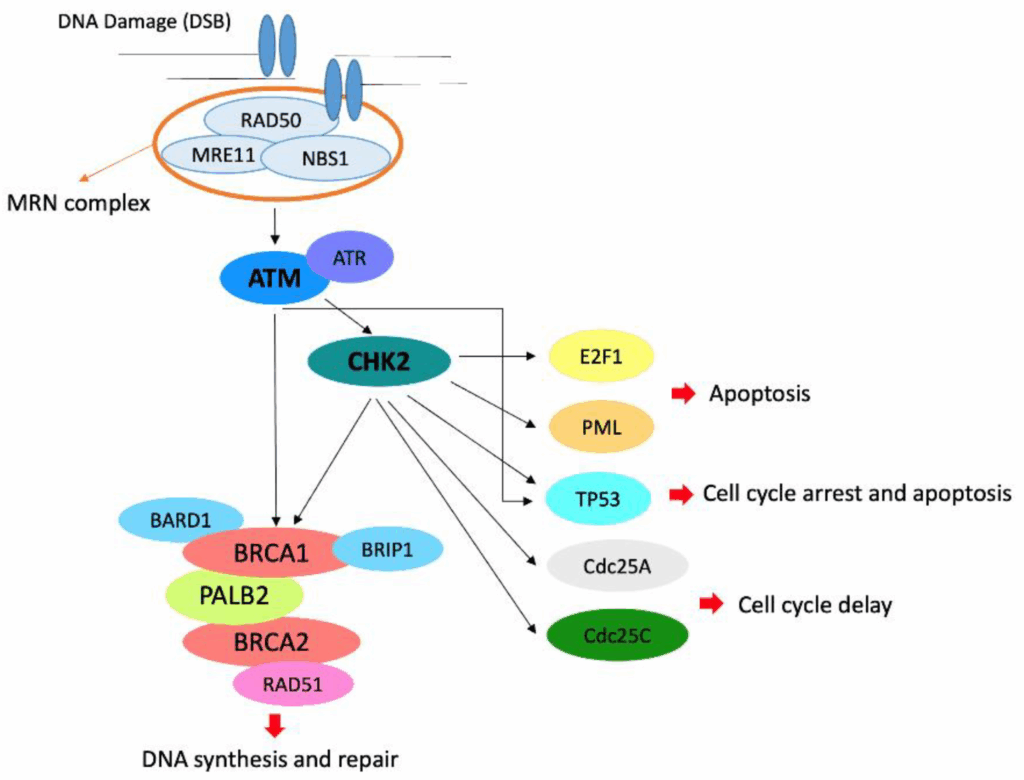
The ATM gene (ataxia-telangiectasia mutated) plays a critical role in the body’s response to DNA damage. It codes for a protein that helps detect DNA double-strand breaks and activates repair processes. When this gene is mutated, it compromises the cell’s ability to correct genetic errors—leading to increased risk for several types of cancer, especially breast cancer.
ATM mutations can be inherited (germline) or acquired (somatic). Individuals with an inherited mutation often don’t have symptoms of ataxia-telangiectasia (a rare childhood disorder), but still carry a higher lifetime risk of developing breast cancer.
Understanding the ATM gene’s function is essential for assessing familial cancer risk and determining appropriate screening or preventive measures. Recent advancements, including trials for The Breast Cancer Vaccine, increasingly consider genetic background like ATM status for eligibility.
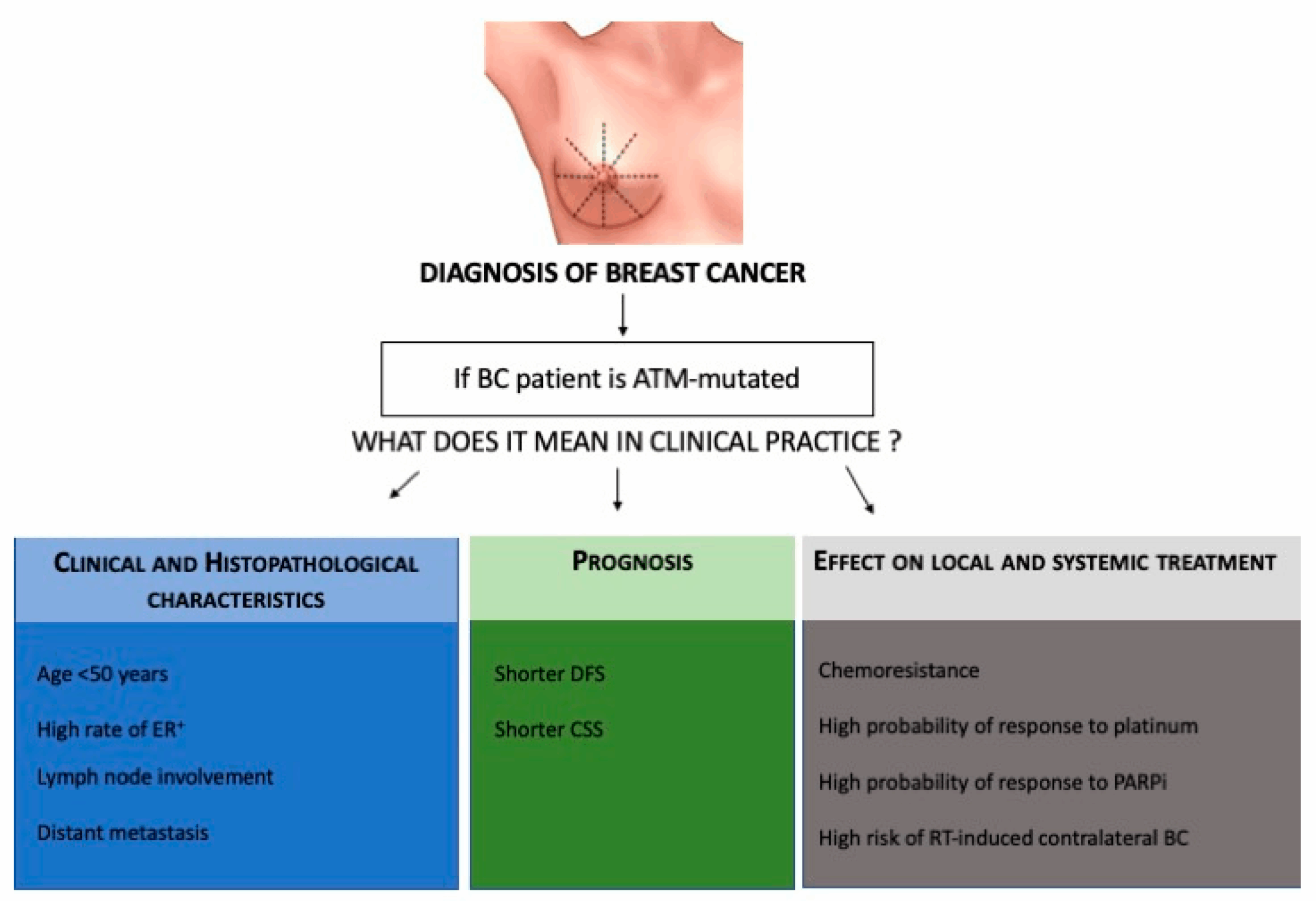
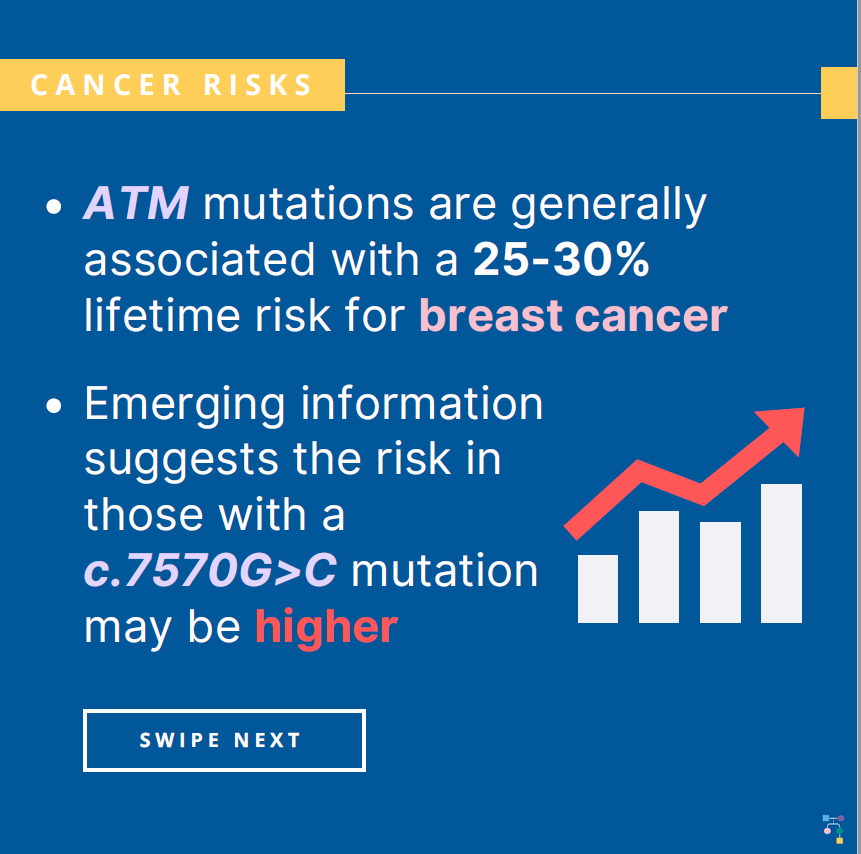
How ATM Mutations Increase Breast Cancer Risk
ATM mutations impair the body’s ability to repair DNA double-strand breaks, especially those caused by environmental or metabolic stress. This leads to genomic instability, allowing mutations to accumulate over time—a hallmark of cancer development.
| ATM Mutation Status | Relative Breast Cancer Risk | Notes on Risk Increase |
| One copy mutated (heterozygous) | 2–4x higher than general population | Especially relevant in women under 50 |
| Two copies mutated (homozygous) | Often associated with A-T syndrome | Not typically seen in adult-onset cancer carriers |
| Co-occurrence with BRCA1/2 | Compound risk effects | May shift treatment plans toward aggressive prevention |
The mutation is most often associated with estrogen receptor-positive (ER+) breast cancer, but has also been found in triple-negative and rare subtypes. Ongoing research continues to clarify the precise cancer mechanisms behind ATM deficiency.
Symptoms of Breast Cancer in People With ATM Mutation
The symptoms of breast cancer in individuals with ATM mutations are generally the same as those in the broader population. However, due to their genetic predisposition, these individuals may develop cancer at a younger age, or experience bilateral or multiple tumors.
Infographic: Symptoms to Watch in ATM Carriers
- A newly formed lump or mass in the breast or underarm
- Skin dimpling or puckering
- Nipple discharge, particularly if bloody
- Persistent pain in one area of the breast
- Changes in breast size or shape
- Redness or scaling of the nipple or breast skin
Because early signs can be subtle, vigilant monitoring is critical, especially for carriers of known pathogenic ATM mutations. Learn more about subtle and often overlooked Breast Cancer Early Symptoms.
How ATM Mutations Compare to BRCA1 and BRCA2
ATM mutations are considered moderate-risk, whereas BRCA1 and BRCA2 are high-risk genes for breast and ovarian cancers. However, their roles in DNA repair are part of the same cellular pathway, which makes ATM functionally relevant in the broader DNA damage response system.
| Feature | ATM Mutation | BRCA1 / BRCA2 Mutations |
| Inheritance pattern | Autosomal dominant | Autosomal dominant |
| Cancer types linked | Breast, pancreatic, prostate | Breast, ovarian, prostate, pancreatic |
| Relative risk of breast cancer | 2–4x baseline | Up to 12x (especially BRCA1 carriers) |
| Screening recommendations | Annual MRI, mammogram, early detection | More aggressive, sometimes prophylactic surgery |
| Risk-reducing medication | May include hormone therapy | Often includes hormonal + surgical options |
ATM mutations generally do not call for prophylactic mastectomy unless family history is extremely strong, but enhanced screening is almost always advised.
How to Get Tested for ATM Mutations
ATM mutation testing is typically done through a genetic test that analyzes DNA from a blood or saliva sample. This is often ordered by a genetic counselor or oncologist for individuals with a personal or family history of cancer.
| Testing Type | Description | Use Case |
| Germline testing (blood/saliva) | Identifies inherited mutations | Used for risk assessment and prevention |
| Tumor testing (somatic) | Looks for ATM mutations in cancer tissue only | Helps guide treatment in diagnosed cases |
| Multigene panel | Screens for ATM and other cancer genes (e.g., BRCA, CHEK2) | Comprehensive testing for high-risk patients |
Testing usually takes 2 to 4 weeks for results. Before testing, a patient may consult with a genetic counselor to discuss implications, privacy, and next steps depending on the results.
What a Positive ATM Mutation Test Means for You
A positive ATM mutation test doesn’t mean a person currently has breast cancer—it means they carry a genetic change associated with increased lifetime risk. The clinical action depends on the mutation’s classification (pathogenic vs. variant of uncertain significance).
| Mutation Type | Clinical Action |
| Pathogenic/likely pathogenic | Enhanced screening, lifestyle counseling, family testing |
| Variant of uncertain significance | Watchful waiting; no change in care until more data is available |
| Negative result | May still recommend screening if family history is strong |
Patients with confirmed pathogenic mutations are generally advised to begin MRI and mammogram screenings earlier than the general population—often around age 30–35. In some cases, risk-reducing medication may also be considered.
ATM Mutation and Other Associated Cancers
ATM mutations are not limited to breast cancer. Carriers also show elevated risks for pancreatic cancer, prostate cancer, and potentially colorectal cancer. These links reflect ATM’s broad role in DNA damage repair throughout the body.
| Cancer Type | Increased Risk with ATM Mutation | Recommended Monitoring |
| Pancreatic cancer | 2–3x higher than average | Consider MRI or endoscopic screening in family clusters |
| Prostate cancer | Higher risk, especially aggressive forms | Early PSA screening, urologic monitoring |
| Colorectal cancer | Research suggests modest increase | Colonoscopy starting earlier if family history present |
Because ATM carriers may face multiple cancer risks, genetic counselors often recommend screening strategies that go beyond breast tissue alone.
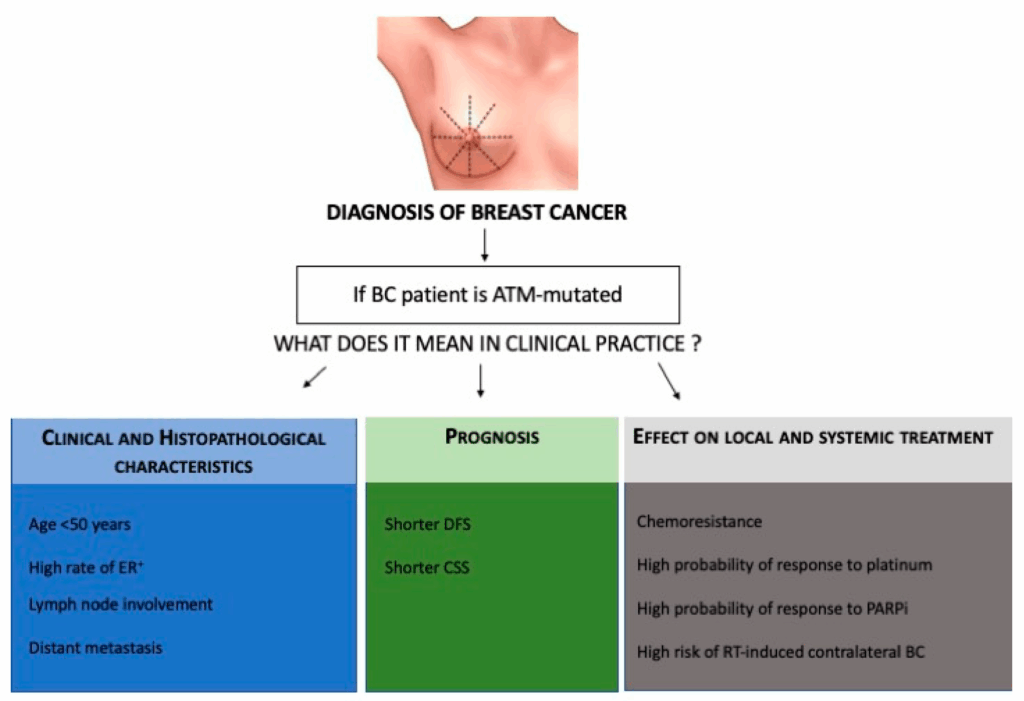
Treatment Planning for Breast Cancer Patients With ATM Mutation
An ATM mutation can influence how doctors plan treatment for breast cancer. While standard therapies (surgery, chemo, hormone therapy) still apply, ATM status may affect the use of radiation and DNA-damaging chemotherapies.
| Treatment Area | Consideration with ATM Mutation |
| Surgery | No significant changes unless strong family history |
| Radiation therapy | May increase toxicity risk due to impaired DNA repair |
| Chemotherapy | Platinum-based chemo may be more effective in ATM carriers |
| Hormone therapy | Often used in ER-positive ATM-related cancers |
| PARP inhibitors | Currently under investigation; may be effective in ATM+ tumors |
Doctors evaluate the full genetic and clinical profile to individualize treatment and minimize long-term side effects. Clinical trials may also be an option, especially for therapies targeting DNA repair pathways—similar to those explored for Angiosarcoma of the Breast.
Should Family Members Get Tested for ATM Mutations?
Yes — if one person tests positive for an ATM mutation, cascade testing is often recommended for biological relatives. Since ATM mutations follow an autosomal dominant inheritance pattern, each first-degree relative (parent, sibling, child) has a 50% chance of carrying the same mutation.
| Family Member | Testing Recommendation |
| First-degree relatives | Strongly recommended |
| Second-degree relatives | Consider if there’s a strong family history |
| Children under 18 | Not routinely tested unless part of a syndrome |
| Spouses or in-laws | Not biologically relevant; no testing needed |
Genetic counselors help families navigate the decision-making process, ensuring testing is done ethically and with full understanding of implications for insurance, mental health, and medical planning.
Screening Guidelines for ATM Mutation Carriers
ATM mutation carriers follow enhanced screening protocols, especially for breast cancer. These begin earlier than in the general population and often involve alternating imaging modalities to improve detection rates.
Infographic: Screening Timeline for ATM Carriers (Females)
- Age 25: Annual clinical breast exam
- Age 30–35: Begin annual MRI with contrast
- Age 40: Add annual mammogram, alternate with MRI every 6 months
- Every 6–12 months: Professional breast exam by physician
- Consider additional screenings: Prostate (males), pancreas (family history), colon (if family history present)
These protocols may evolve as research improves our understanding of ATM’s role across cancers. Compliance with such schedules significantly improves early detection and survival.
Psychological and Ethical Considerations of ATM Genetic Testing
Learning about a pathogenic ATM mutation can be emotionally challenging. It affects not only the individual’s health outlook but also future family planning, feelings of responsibility, and anxiety about cancer. Ethical considerations must be addressed with sensitivity.
| Area of Concern | Patient and Family Impact |
| Anxiety and fear | Worry about future illness or passing it to children |
| Guilt | Feelings about “causing” genetic risk in offspring |
| Privacy and disclosure | Dilemma over sharing status with employers or insurers |
| Discrimination protection | GINA laws protect against genetic discrimination in U.S. |
| Reproductive decisions | May influence fertility preservation or preimplantation genetic testing |
Genetic counseling plays a vital role in helping individuals understand their options and cope with emotional responses in a supportive, informed setting.
Latest Research on ATM and Breast Cancer Therapies
ATM-related breast cancer is a growing focus in oncology research. Scientists are exploring how ATM-deficient tumors respond to targeted therapies, including PARP inhibitors, ATR inhibitors, and other agents that exploit defective DNA repair pathways.
| Research Area | Current Findings and Clinical Trials |
| PARP inhibitors (e.g., olaparib) | Show activity in ATM-deficient cells; being trialed in ATM+ patients |
| ATR inhibitors | Potentially lethal to ATM-deficient tumor cells |
| Immunotherapy | Early research suggests ATM loss may alter immune response |
| Synthetic lethality strategies | Combining DNA damage with repair blockade shows promise |
Although BRCA mutations are still the primary focus of targeted treatment, ATM mutations are increasingly part of precision oncology trials, paving the way for more personalized care in the future.
Lifestyle and Risk Reduction for ATM Carriers
While genetics cannot be changed, lifestyle choices can reduce overall cancer risk—even for those with ATM mutations. These include factors that support immune function, hormonal balance, and DNA repair mechanisms.
| Lifestyle Factor | Impact on Risk Reduction |
| Smoking cessation | Lowers risk of many ATM-related cancers |
| Balanced diet (rich in fiber, antioxidants) | Supports DNA repair, reduces inflammation |
| Physical activity | Linked to lower estrogen and insulin levels |
| Alcohol moderation | Excess alcohol increases risk of hormone-sensitive cancers |
| Weight management | Reduces inflammation and hormone-related cancer risk |
ATM carriers should also avoid unnecessary radiation exposure, especially from repeated scans or chest radiation during youth, which may compound risk due to impaired DNA repair.
Insurance and Financial Considerations for Genetic Carriers
Testing positive for an ATM mutation may raise concerns about insurance eligibility and cost of care. Fortunately, in many countries, legal protections are in place, but coverage still varies by policy and region.
| Issue | Details and Implications |
| Genetic Information Nondiscrimination Act (GINA) | Protects against employment and health insurance discrimination (U.S.) |
| Life insurance | Not protected under GINA; applicants should inquire carefully |
| Testing costs | Often covered for high-risk individuals or with family history |
| Surveillance costs | MRI and specialist visits may have co-pays or deductibles |
| Coverage for relatives | May be excluded unless proven to carry the mutation |
Early conversations with insurers and financial counselors can help plan long-term care strategies and avoid unexpected expenses.
Differences in Management by Age or Gender
ATM mutation–associated cancer risks affect individuals differently across life stages and sexes. Management must be personalized to optimize prevention and minimize unnecessary intervention.
| Demographic Group | Clinical Recommendations |
| Young adult women (20s–30s) | Begin surveillance early; delay risk-reducing meds unless high-risk |
| Postmenopausal women | Evaluate for hormone-modulating agents if ER-positive |
| Men | Begin PSA screening early; consider pancreatic monitoring |
| Seniors (70+) | Surveillance continues, but intensity may be reduced |
Men may be less aware of ATM-related risk, especially for prostate and pancreatic cancer, highlighting the need for tailored outreach and education across genders.
Advocacy and Support Resources for ATM Mutation Carriers
Living with an inherited cancer risk can be isolating. Fortunately, several advocacy organizations offer education, emotional support, and connection with others facing similar challenges.
| Resource Name | Focus Area |
| FORCE (Facing Our Risk of Cancer Empowered) | Peer support, education for hereditary cancers |
| Bright Pink | Young women’s breast and ovarian cancer prevention |
| ATM Rare Disease Support | Ataxia-telangiectasia community (for biallelic cases) |
| Genetic counselors (via NSGC.org) | Personalized risk planning and family guidance |
| Clinical trial registries | Find ATM-targeted studies via clinicaltrials.gov |
These resources empower carriers to take charge of their health while remaining informed and emotionally supported.
FAQ – ATM Mutation & Breast Cancer
1. Can men carry ATM mutations?
Yes, ATM mutations affect both men and women. In men, they increase the risk for prostate and pancreatic cancer, not breast cancer directly.
2. Is ATM mutation linked to any rare cancer types?
There’s emerging evidence linking ATM mutations to rare tumors like medullary thyroid cancer and soft tissue sarcomas, but these are less common.
3. Does ATM mutation affect treatment side effects?
Possibly. Because ATM is involved in DNA repair, chemotherapy or radiation side effects may be heightened, but this varies individually.
4. Can someone have both ATM and BRCA mutations?
Yes, though rare. Dual mutation carriers may need significantly modified risk-reduction and screening plans.
5. Is ATM mutation the same as ataxia-telangiectasia?
Only if two defective copies are inherited (homozygous), which causes A-T disease. Most breast cancer–related cases are heterozygous.
6. Are there prenatal testing options for ATM mutations?
Yes, options like PGD (preimplantation genetic diagnosis) exist for couples undergoing IVF and carrying ATM mutations.
7. What is a variant of uncertain significance (VUS)?
It’s a mutation that hasn’t been proven harmful or benign. No action is typically taken unless new data emerges.
8. Can ATM mutation be found accidentally on other tests?
Yes, some people discover ATM status incidentally during multigene panel testing or tumor sequencing.
9. Does ATM mutation cause early menopause or fertility issues?
No direct link is known, but treatment decisions in ATM+ patients may impact reproductive choice
10. Can ATM mutations skip generations?
No, but they may appear to skip generations if a parent carried the mutation but didn’t develop cancer.
11. Do lifestyle changes reverse mutation risk?
Lifestyle helps lower the overall cancer burden but does not eliminate the elevated genetic risk.
12. Are there supplements or diets specific for ATM carriers?
There’s no proven supplement, but diets rich in antioxidants and low in inflammation may support DNA repair.
13. Can ATM carriers donate blood or organs?
Yes. There are no restrictions unless the donor has an active cancer diagnosis.
14. Is there a specific blood test to monitor ATM-related cancer development?
No single marker exists; imaging and clinical exams remain the primary methods of surveillance.
15. Are ATM mutations considered rare?
They are less common than BRCA mutations but not extremely rare—found in approximately 1% of the population.