Ascites Management in 2025: Emerging Therapies and Technologies
- Part 1: Introduction — What Is Ascites and Why Does It Matter?
- Part 2: Pathophysiology — Understanding the Mechanics Behind the Fluid
- Part 3: Diagnostic Approaches — How Do We Know What’s Going On?
- Part 5: Innovative Therapies — Changing the Game in Ascites Management
- Part 6: Surgical Interventions — When Medical Treatments Aren’t Enough
- Part 7: Recent Developments (2025–2026) — What’s New in Ascites Management?
- Part 8: Patient Management and Support — The Heart of Effective Care
- Frequently Asked Questions (FAQ)
- Conclusion — Toward a Brighter Future in Ascites Management
Introduction — What Is Ascites and Why Does It Matter?
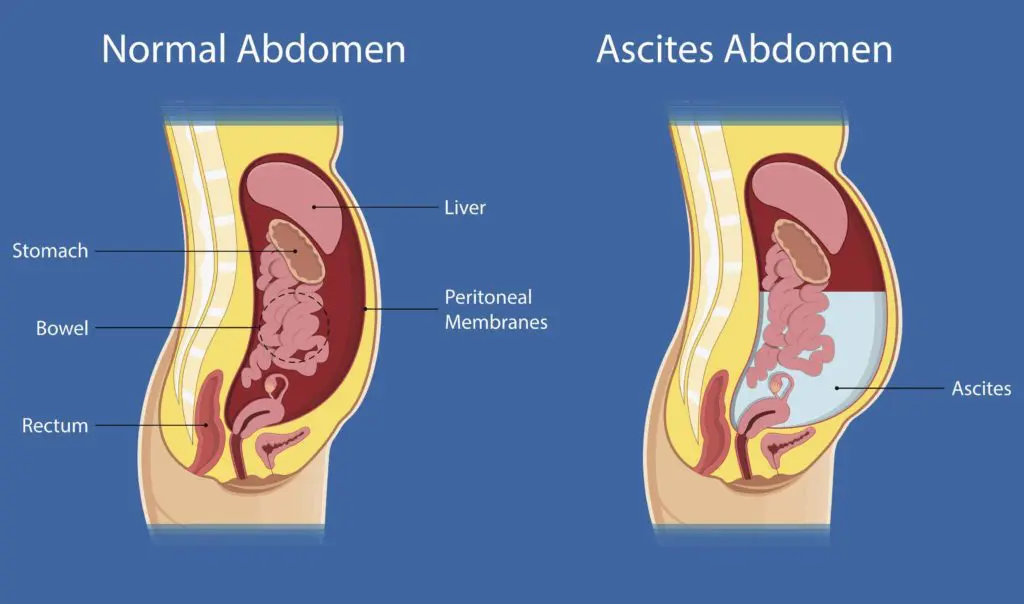
Ascites might sound like a complicated medical term, but at its core, it’s something quite simple — the buildup of fluid in the space inside your abdomen, called the peritoneal cavity. But this simple definition masks a complex problem. Why does fluid gather there in the first place? And why should we care beyond the obvious discomfort it causes?
Most often, ascites is a symptom rather than a disease itself. It signals that something deeper is going wrong inside the body. The most common cause is cirrhosis, which is scarring of the liver due to chronic damage from conditions like long-term alcohol use or hepatitis. When the liver is scarred, blood can’t flow through it properly, causing pressure to build up and forcing fluid out into the abdomen.
But cirrhosis isn’t the only culprit. Heart failure, kidney disease, certain cancers, and infections can all lead to ascites, each with its own unique underlying mechanisms. This means ascites isn’t just one condition to treat; it’s a signpost pointing toward a range of possible diseases that require different approaches.
Why Does Ascites Impact Quality of Life So Dramatically?
If you’ve never experienced ascites, it might be hard to grasp how profoundly it can affect someone’s daily life. Imagine your abdomen slowly swelling over weeks or months, becoming heavy and tight. Simple tasks like walking, bending, or even breathing deeply can become exhausting. Clothes stop fitting, sleep becomes uncomfortable, and the constant sense of bloating can sap your energy and mood.
But it’s more than just discomfort. Ascites can lead to serious complications such as infections inside the fluid (called spontaneous bacterial peritonitis), kidney dysfunction, and breathing difficulties when the fluid presses against the lungs. This combination of physical symptoms and the emotional weight of chronic illness can significantly reduce overall well-being.
So when we talk about managing ascites in 2025, we’re not just trying to remove fluid — we’re aiming to restore as much comfort and function as possible, improving quality of life in a way that feels sustainable.
Pathophysiology — Understanding the Mechanics Behind the Fluid
Have you ever wondered what’s actually happening inside your body when fluid starts to accumulate in the abdomen? It turns out that ascites is the result of a complicated chain reaction involving pressure changes, hormonal signals, and organ dysfunction.

At the center of most ascites cases, especially those linked to cirrhosis, is a phenomenon called portal hypertension. Picture the liver as a busy highway where blood flows smoothly. When the liver is damaged by scarring, this highway becomes clogged, forcing traffic (blood) to back up. This increased pressure pushes fluid out of the blood vessels and into the surrounding peritoneal cavity.
But pressure alone doesn’t explain everything. Another key factor is the drop in blood proteins, especially albumin, which helps keep fluid inside the blood vessels. When the liver can’t make enough albumin, the blood vessels lose their “pull,” allowing fluid to leak out more easily.
Then the body’s clever but sometimes frustrating compensatory mechanisms kick in—an echo of what we observe in other systemic diseases, such as H1N1 Influenza with Drug Resistance, where the body’s own defenses can sometimes complicate treatment and recovery.
It’s Not Always Cirrhosis: Other Paths to Fluid Buildup
Ascites isn’t a one-trick pony. Different diseases cause fluid accumulation in different ways. In cancer, for example, tumor cells can invade the lining of the abdomen, making blood vessels leakier and blocking the normal drainage of fluid. In heart failure, the heart’s inability to pump efficiently backs pressure up into the veins, leading to fluid leakage into the abdomen.
Even infections like tuberculosis can inflame the peritoneum and cause fluid to build up as part of the immune response.
Each of these pathways leads to the same problem — too much fluid where it doesn’t belong — but the underlying cause changes how doctors treat the condition.
Why Does This Complex Biology Matter?
You might wonder why it’s so important to understand these messy inner workings. The answer is that treatment isn’t one-size-fits-all. If we only focus on draining fluid without addressing the underlying pressures, protein imbalances, or hormonal signals, the problem keeps coming back.
Knowing the root cause helps doctors choose the right treatment, predict complications, and tailor care to each patient’s needs. It also opens doors for new therapies designed to interrupt these biological processes and offer longer-lasting relief.
Diagnostic Approaches — How Do We Know What’s Going On?
At first glance, diagnosing ascites might seem obvious—after all, a visibly swollen belly is hard to miss. But in medicine, things are rarely that simple. Sometimes the swelling can be subtle or mistaken for other conditions like weight gain or bloating from gas, especially in patients with a higher body mass or tense abdominal muscles. That’s why doctors rely on a careful combination of physical examination, imaging, and laboratory tests to confirm whether fluid has indeed accumulated in the abdomen, how much is there, and most importantly, what is causing it.
Despite the high-tech tools available today, the physical exam remains a valuable starting point. Skilled clinicians use their hands to feel (palpate) the abdomen and tap (percuss) to listen for differences in sound that indicate fluid presence. They perform maneuvers like the fluid wave test—pressing on one side of the belly and feeling for the ripple of fluid on the other—and shifting dullness, where changing the patient’s position causes the fluid to settle differently, changing the sound doctors hear when tapping. While these bedside tests can provide useful clues, they’re not foolproof. Small amounts of fluid may go undetected, and factors like obesity or muscle tone can make the exam less reliable.
That’s where imaging takes center stage. Ultrasound has become the gold standard for confirming ascites because it’s noninvasive, quick, and safe. It can detect even tiny pockets of fluid invisible to the naked eye or touch. Beyond simply confirming fluid’s presence, ultrasound guides procedures such as paracentesis, helping doctors insert needles precisely and safely. In more complex situations—such as suspected cancer or infection—CT scans or MRI offer detailed images of the abdomen, revealing abnormalities that may explain why fluid is accumulating.
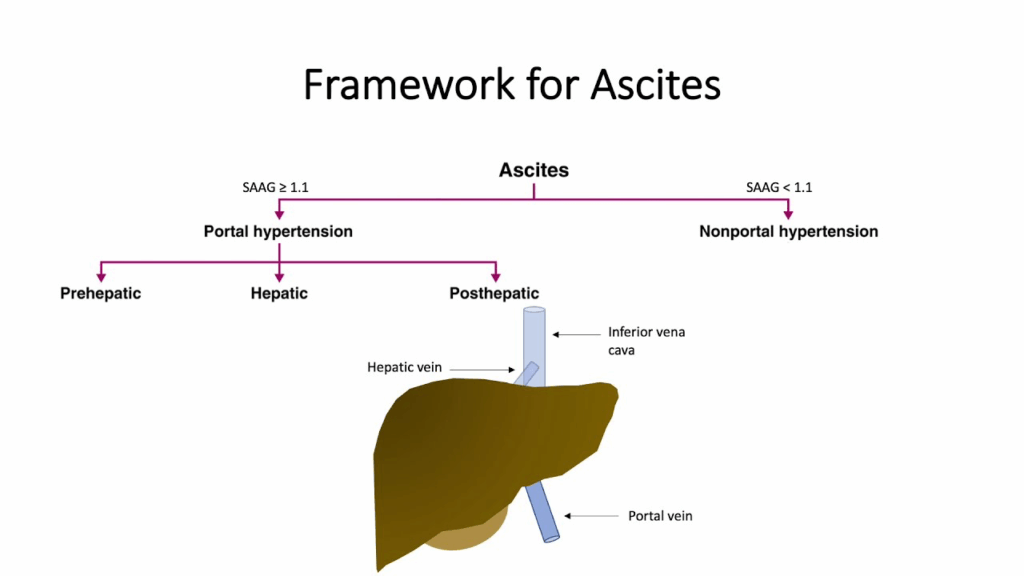
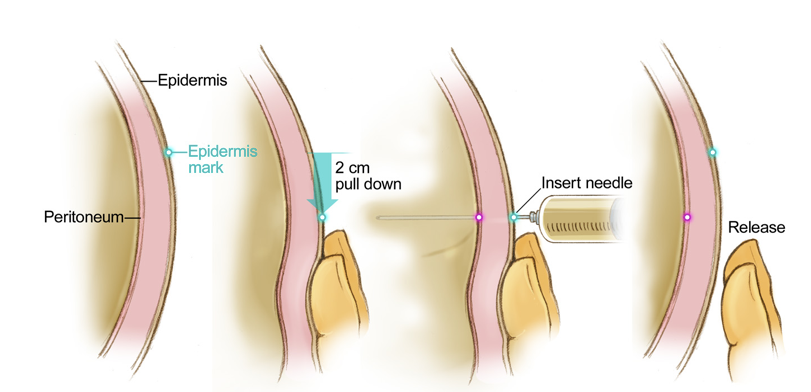
Lab testing of the fluid itself, obtained through paracentesis, is often the key to unlocking the mystery behind ascites. While the idea of a needle insertion might sound intimidating, paracentesis is usually performed with local anesthesia and minimal discomfort. The collected fluid undergoes thorough analysis—its clarity, protein content, and cell counts can indicate whether infection or cancer is present. A particularly important test is the serum-ascites albumin gradient (SAAG), which compares albumin levels in the blood and fluid to determine if portal hypertension is causing the ascites. This distinction is crucial, as it directs the choice of treatment.
Paracentesis doesn’t stand alone. Blood tests complement the picture by assessing liver and kidney function, electrolyte balance, and markers of inflammation or cancer. Together, these tests help clinicians understand not only the presence of ascites but also the severity and nature of the underlying disease. This comprehensive approach ensures that treatment plans are tailored to each patient’s unique situation.
Advances in technology are further transforming diagnosis. Portable ultrasound devices now fit in the palm of a hand, enabling bedside imaging even in remote or resource-limited settings. Artificial intelligence is beginning to assist radiologists by identifying subtle changes in imaging that might otherwise be missed. Meanwhile, researchers are exploring biomarkers—molecules in blood or fluid that could speed up diagnosis of infections or cancer, allowing earlier intervention.
So, while a swollen belly might seem like a straightforward symptom, figuring out the exact cause and extent of ascites is a nuanced process that blends old-school examination skills with cutting-edge technology. This thorough detective work lays the foundation for effective, personalized treatment that targets the problem precisely rather than just treating symptoms.
Traditional Treatment Modalities: The Foundation We Still Lean On
When it comes to managing ascites, the approaches we’ve relied on for decades still form the backbone of treatment. It’s interesting because, at first glance, the goal seems simple—reduce that excess fluid and relieve symptoms. But anyone who’s dealt with ascites, or cared for someone who has, knows it’s never quite that straightforward.
Take dietary changes, for example. The advice to restrict salt might sound like a no-brainer, but it’s actually a delicate balance. Salt, or sodium, plays a huge role in how much fluid your body holds onto. So cutting back on salt is crucial because it helps reduce the volume of fluid accumulating in the abdomen. But here’s the catch: salt is everywhere in our food, and limiting it isn’t just about taste—it’s about retraining the body’s internal mechanisms that regulate fluid. Patients often find this challenging, especially since a strict low-sodium diet can make meals less satisfying and adherence difficult over the long haul.
Because diet alone often isn’t enough, doctors turn to diuretics, the medications designed to flush excess water and salt through the kidneys. You’ve probably heard of drugs like spironolactone and furosemide. They work together to block the body’s tendency to retain sodium, especially the hormone aldosterone, which signals the kidneys to hoard salt and water. But diuretics are a double-edged sword—if dosed incorrectly, they can lead to dehydration, electrolyte imbalances, or even kidney damage. That means patients require careful monitoring, regular blood tests, and dose adjustments, which can feel like a constant balancing act.
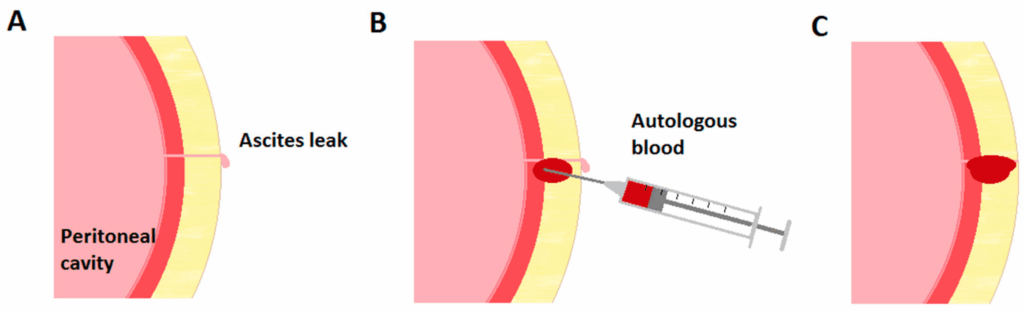
When ascites becomes severe, those medications might not be enough to provide relief quickly. That’s when paracentesis, the procedure to drain fluid directly from the abdomen with a needle, comes into play. It can be a literal lifesaver, offering immediate comfort by reducing abdominal pressure and making breathing and movement easier. But paracentesis is not a cure; the fluid usually comes back, sometimes quickly. Repeated procedures are inconvenient and carry risks such as infection or bleeding. Plus, for many patients, the cycle of drainage and reaccumulation can be emotionally draining as well.
There’s also the role of intravenous albumin in some cases, particularly after large-volume paracentesis. Albumin is a protein that helps pull fluid back into the bloodstream and supports kidney function, preventing some of the complications that can arise from rapid fluid shifts. However, albumin infusions are costly and must be used thoughtfully, weighing the benefits against the financial and medical costs.
In essence, while these traditional treatments have saved countless lives and improved quality of life for many, they often address the symptom of ascites rather than the underlying problem. They also don’t always prevent the fluid from returning, meaning patients face ongoing discomfort, frequent hospital visits, and repeated interventions.
It’s this very reality—the limitations and burdens of traditional therapy—that has propelled research and innovation toward more effective, patient-friendly options. As you might guess, the next wave of treatments aims not just to drain fluid but to change how and why it accumulates in the first place, promising a future where managing ascites feels less like a relentless battle and more like a controlled part of life.
Innovative Therapies — Changing the Game in Ascites Management
If traditional treatments for ascites feel like managing the symptoms on a revolving door, emerging therapies in 2025 offer a glimpse into a future where that door might finally slow down. Over the past few years, the medical community has been energized by new technologies and drugs designed to target the underlying causes more effectively, reduce hospital visits, and improve patients’ day-to-day lives.
One of the most exciting advances is the development of implantable devices like the alfapump®. Imagine having a small, battery-powered pump implanted inside the body that automatically moves excess fluid from the abdomen into the bladder, where it can be eliminated naturally through urination. This technology reduces the need for repeated paracentesis, sparing patients the discomfort and inconvenience of frequent hospital procedures. It’s like having an internal drainage system that works continuously, quietly, and safely.
Of course, implantable pumps aren’t for everyone—they require careful patient selection and ongoing management—but for many, they represent a major leap forward. The convenience and autonomy they offer can restore a sense of normalcy and freedom that traditional treatments often take away.
Alongside device innovations, pharmacological advances are reshaping the landscape. Researchers are developing new drugs that more precisely target the hormonal and vascular pathways responsible for fluid retention. Some novel agents aim to reduce portal hypertension, the high blood pressure in the veins leading to the liver that plays a key role in fluid leakage. Others focus on modulating the body’s inflammatory responses or improving kidney function, addressing the problem from multiple angles.
These therapies often come with fewer side effects and better tolerability than older medications, potentially allowing patients to manage ascites with less frequent doctor visits and less disruption to their daily routines.
Another promising area is the use of biologics—specialized drugs made from living organisms—which can target specific molecules involved in the cascade of events leading to ascites. While still in early stages, these treatments hold the potential to transform care by intervening deeper in the disease process.
What makes these innovations so hopeful is not just their scientific sophistication, but their focus on patient experience. Managing ascites is not just about controlling fluid; it’s about improving quality of life, reducing hospital admissions, and giving patients back control.
Of course, with any new therapy, there are questions about cost, accessibility, and long-term outcomes. Clinical trials and real-world experience continue to build our understanding, helping refine who benefits most and how best to integrate these advances into everyday practice.
Looking ahead, the combination of implantable devices, smarter drugs, and personalized care plans paints a promising picture. For patients and clinicians alike, these emerging therapies offer a way to move beyond symptom management toward more sustainable, effective control of ascites.
Surgical Interventions — When Medical Treatments Aren’t Enough
For many patients with ascites, traditional therapies like diet, diuretics, and fluid drainage provide meaningful relief. But sometimes, the underlying problems causing fluid buildup are so severe or resistant to treatment that surgery becomes the next step. Surgical interventions aren’t the first line of defense—they’re reserved for carefully selected patients who might benefit most from a more invasive approach.
One of the most common and effective surgical procedures for ascites related to liver disease is the Transjugular Intrahepatic Portosystemic Shunt, better known as TIPS. This procedure creates a channel inside the liver connecting two major veins, allowing blood to bypass the scarred liver tissue. By reducing the high pressure in the portal vein (portal hypertension), TIPS helps decrease the driving force pushing fluid into the abdomen.
The beauty of TIPS lies in how it tackles the root cause of ascites: elevated pressure within the liver’s circulation. By diverting blood flow, it reduces portal pressure and, as a result, fluid accumulation. For patients who don’t respond to diuretics or continue to have frequent, troublesome ascites despite repeated paracentesis, TIPS can be a game-changer, significantly improving symptoms and quality of life.
However, TIPS isn’t suitable for everyone. The procedure carries risks, including worsening liver function or precipitating hepatic encephalopathy—a condition where toxins normally cleared by the liver affect brain function. That’s why careful patient selection is crucial. Doctors evaluate liver function, overall health, and potential risks before recommending TIPS. Close monitoring after the procedure helps manage any complications and assess its effectiveness.
In rare cases, more extensive surgical options may be considered, especially when ascites is linked to cancers or infections that require removing diseased tissue or relieving blockages. These procedures tend to be more complex and carry higher risks, so they’re typically reserved for very specific situations.
Surgical interventions offer hope to patients struggling with refractory ascites—fluid buildup that refuses to respond to standard treatments. While surgery may sound daunting, advances in techniques and postoperative care have made these options safer and more effective than ever before. For many, it represents a vital step toward regaining control over a condition that can otherwise feel overwhelming.
As we continue exploring ascites management, it becomes clear that the best care often blends multiple approaches—medical, procedural, and surgical—tailored to each patient’s unique situation. This personalized strategy maximizes benefits while minimizing risks.
Recent Developments (2025–2026) — What’s New in Ascites Management?
As we step into the mid-2020s, the landscape of ascites treatment is evolving faster than ever before. Building on years of foundational research and innovation, 2025 and 2026 have brought a wave of exciting clinical trial results and regulatory approvals that are reshaping how patients with ascites are cared for.
One of the most significant advances is the FDA approval of next-generation implantable devices that expand on the success of earlier pumps like the alfapump®. These newer devices are more compact, have longer battery lives, and include enhanced safety features such as real-time monitoring of fluid volume and automated adjustments based on patient needs. This means patients can expect fewer hospital visits, more consistent fluid control, and greater peace of mind.
Parallel to these device improvements, several novel pharmacological agents have gained traction. Trials of drugs that more precisely target portal hypertension have shown promising results, reducing not just fluid accumulation but also improving overall liver function markers. These medications often come with better side effect profiles, which is a big win for patients who struggle with the fatigue, electrolyte disturbances, or kidney issues associated with older drugs.
Another exciting area is the integration of biomarkers and personalized medicine into clinical practice. Researchers have identified molecular signatures in blood and ascitic fluid that help predict which patients are likely to develop complications or respond best to specific treatments. This allows clinicians to tailor therapies much more precisely than before, avoiding the trial-and-error approach and focusing on what will work best for each individual.
On the technology front, digital health platforms and wearable devices are becoming integral to patient care. These tools enable remote monitoring of symptoms, fluid status, and vital signs, allowing healthcare teams to intervene early if a patient’s condition worsens. For patients, this means greater connection with their care team without the burden of frequent in-person visits.
Of course, integrating these advancements into everyday clinical practice requires collaboration across specialties—hepatologists, interventional radiologists, surgeons, and primary care providers working together. Many hospitals are establishing multidisciplinary ascites management teams, which have been shown to improve outcomes, reduce hospital readmissions, and enhance patient satisfaction.
While there’s still much to learn, these recent developments signal a clear trend: ascites management is moving toward more precise, less invasive, and more patient-centered care. This progress brings hope for better quality of life and fewer complications for people living with this challenging condition.
Patient Management and Support — The Heart of Effective Care
Managing ascites isn’t just about procedures and medications—it’s about supporting the whole person. In 2025, the importance of a multidisciplinary approach to care is clearer than ever. Patients don’t just need treatment for fluid buildup; they need coordinated support that addresses their physical symptoms, emotional well-being, and day-to-day challenges.
At the center of this approach are teams that bring together hepatologists, nephrologists, interventional radiologists, nutritionists, social workers, and nursing specialists. Each professional offers a unique perspective and skill set, ensuring that care plans are comprehensive and responsive to changing needs.
One key aspect is regular monitoring. Ascites can fluctuate, and early signs of worsening—like subtle weight gain or abdominal discomfort—can be missed without vigilant follow-up. Modern clinics often employ remote monitoring technologies, including wearable devices and smartphone apps, allowing patients to track symptoms and communicate easily with their care team. This proactive approach helps catch problems early, reducing hospital admissions and complications.
Nutrition support also plays a crucial role. Maintaining adequate protein intake without excessive sodium is a delicate balance that can be tough to achieve. Dietitians work closely with patients to craft individualized plans that keep them nourished and strong, helping to prevent malnutrition, which can worsen outcomes.
Emotional and psychological support is just as vital—especially considering how chronic conditions like ascites can mirror broader patterns in mental health struggles, as explored in our feature on Mental Health Trends 2025, where chronic physical stress often contributes to emotional burnout and depression.
Education empowers patients, too. Understanding why certain treatments are necessary, how to recognize early warning signs, and when to seek help equips patients to be active partners in their care. This shared decision-making improves adherence and satisfaction.
In short, effective ascites management is as much about relationships and communication as it is about medical interventions. The best outcomes come when patients feel supported, informed, and cared for by a responsive, knowledgeable team.
Frequently Asked Questions (FAQ)
What exactly is ascites and why does it happen?
Ascites is the abnormal buildup of fluid in the abdominal cavity, most often caused by liver disease such as cirrhosis, but also by heart failure, cancer, infections, or kidney problems. It happens because of increased pressure in blood vessels, low blood protein levels, and hormonal changes that cause the body to retain fluid.
How do doctors diagnose ascites?
Diagnosis involves a physical exam, imaging like ultrasound, and sometimes fluid sampling via paracentesis. Blood tests help identify the underlying cause and assess organ function. Modern tools such as portable ultrasounds and biomarkers improve accuracy and speed.
What are the traditional treatments for ascites?
Treatment often begins with dietary sodium restriction and diuretics to reduce fluid buildup. When necessary, paracentesis removes fluid directly from the abdomen. Intravenous albumin may be given to support blood volume during fluid removal.
What new therapies are available for ascites management?
Recent innovations include implantable pumps that automatically drain fluid, novel drugs targeting hormonal and vascular pathways, and biologics that intervene deeper in the disease process. These therapies aim to reduce symptoms with fewer side effects and improve quality of life.
When is surgery considered for ascites?
Surgical options like the Transjugular Intrahepatic Portosystemic Shunt (TIPS) are used for patients with refractory ascites unresponsive to medical treatment. TIPS lowers portal vein pressure by creating a bypass inside the liver, reducing fluid accumulation. Surgery requires careful patient selection due to risks.
How important is ongoing patient support in managing ascites?
It’s critical. Multidisciplinary care teams provide medical treatment, nutrition advice, psychological support, and monitoring. Remote technologies and education empower patients to manage symptoms and seek timely care, improving outcomes and quality of life.
What are the recent developments in ascites care?
In 2025 and beyond, advances include improved implantable devices with better safety and monitoring features, new drugs with fewer side effects, personalized medicine using biomarkers, and digital health tools for remote patient monitoring.
Conclusion — Toward a Brighter Future in Ascites Management
Ascites has long been a challenging condition that signals serious underlying illness and significantly impacts patients’ lives. While traditional treatments remain essential, they often focus on symptom relief rather than the root causes, leaving many patients trapped in a cycle of fluid buildup and drainage.
The past few years have brought remarkable progress. Innovative devices, smarter drugs, and personalized care approaches are transforming how we manage ascites—shifting from reactive to proactive, from repetitive procedures to sustainable control. Multidisciplinary teams and digital technologies enhance patient support, helping people live fuller, more comfortable lives despite their condition.
As research continues and new therapies emerge, the outlook for patients with ascites is improving—much like in the case of Malaria, where recent developments have steadily shifted outcomes in favor of more effective, patient-centered interventions in previously hard-to-manage conditions.









