Abdominal Pain in Colorectal Cancer
Abdominal Pain in Colorectal Cancer: Causes, Diagnosis, and Relief
- What Does Abdominal Pain Mean in Colorectal Cancer?
- The Mechanism: Why Tumors Cause Abdominal Pain
- How Common Is Abdominal Pain in Colorectal Cancer?
- What Causes Abdominal Pain in This Cancer Type?
- When to Take Abdominal Pain Seriously
- Diagnostic Tools to Pinpoint the Source
- How Pain in Colorectal Cancer Is Treated
- Can This Pain Be Prevented or Reduced Early?
- Does the Pain Go Away Over Time?
- Insights from Oncologists on Managing Pain
- 15 Questions to Ask Your Doctor About Abdominal Pain in Colorectal Cancer (FAQ)
What Does Abdominal Pain Mean in Colorectal Cancer?
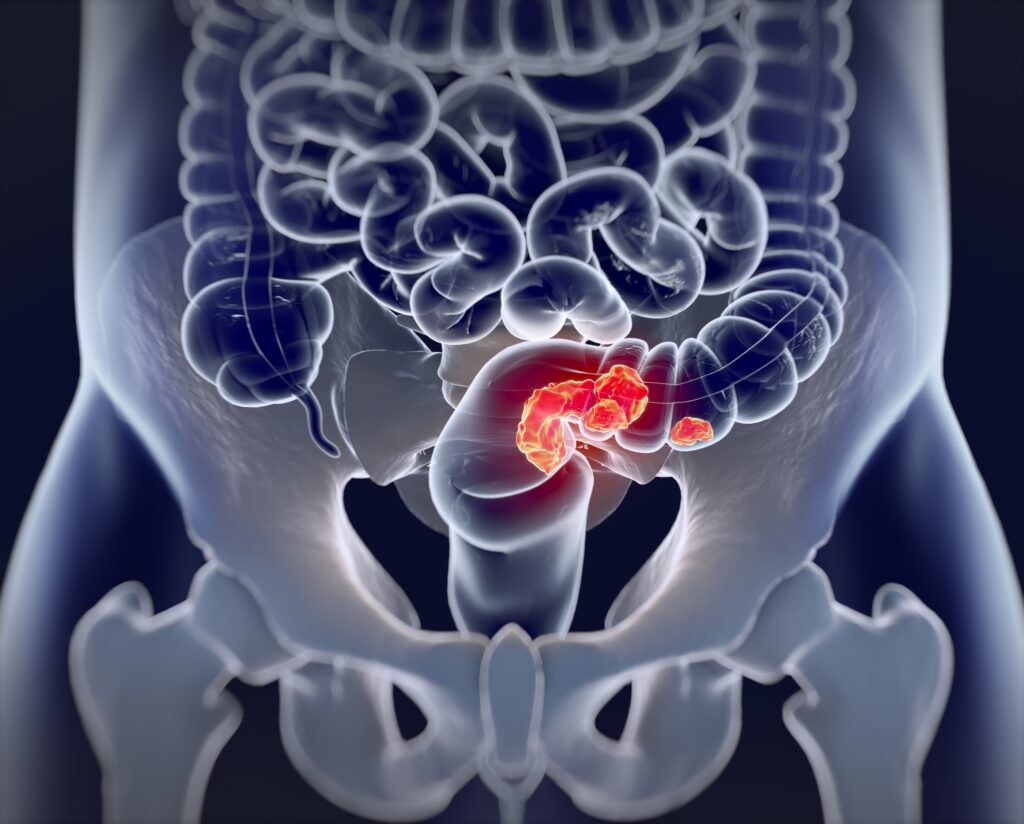
Abdominal pain is one of the most frequent and distressing symptoms in people with colorectal cancer. Unlike general pain, which can arise from benign digestive issues, this type of discomfort often suggests tumor growth, obstruction, or inflammation in the bowel wall. For some patients, it’s a dull ache that comes and goes; for others, it presents as sharp, localized cramping—especially during bowel movements or after eating.
Pain may originate directly from the tumor, particularly when it causes narrowing of the intestinal lumen or invades surrounding tissues. In advanced stages, pain may radiate to the lower back or pelvis. In some cases, this symptom is one of the early symptoms of colon cancer, though it’s often overlooked or mistaken for irritable bowel syndrome (IBS).
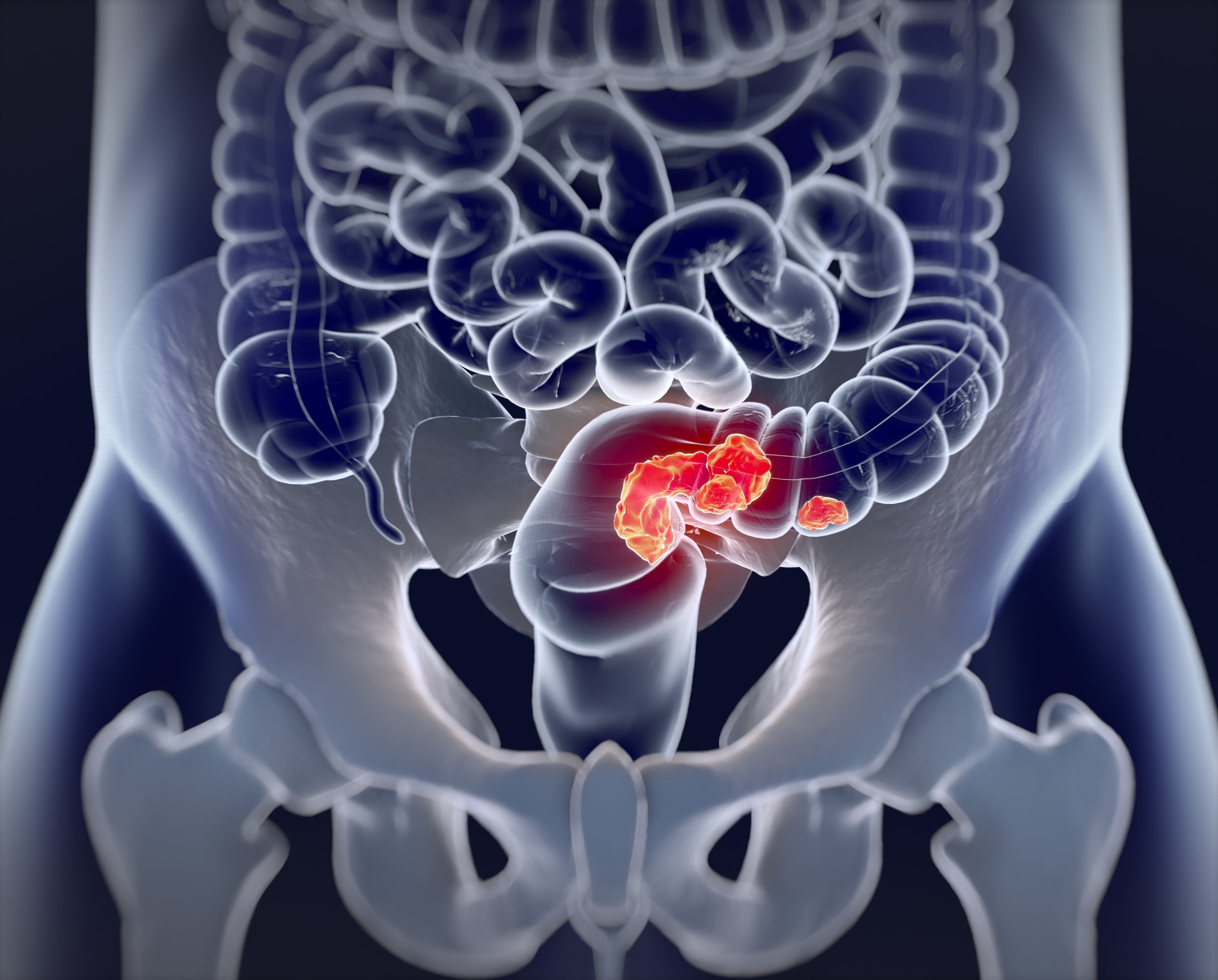
The Mechanism: Why Tumors Cause Abdominal Pain
Colorectal tumors disrupt the normal flow of digestive contents. As the tumor grows, it may partially or completely block the bowel, leading to pressure buildup and distension of the colon. This distension activates pain receptors in the bowel wall and surrounding peritoneal lining.
In addition to mechanical obstruction, pain can also result from:
- Local inflammation around the tumor
- Ulceration or bleeding within the lesion
- Perforation of the bowel wall in advanced cases
- Tumor invasion of nearby organs or nerves
Sometimes, pain is indirectly caused by cancer therapies such as radiation, surgery, or chemotherapy-induced enteritis. The bowel becomes more sensitive, and even normal peristalsis can be painful.
How Common Is Abdominal Pain in Colorectal Cancer?
Abdominal pain is reported in up to 60–80% of patients with colorectal cancer at some point in their illness. Its prevalence depends on the tumor location and stage at diagnosis.
| Tumor Site | Likelihood of Pain |
| Left-sided colon cancer | Moderate to high |
| Right-sided colon cancer | Low to moderate |
| Rectal cancer | Variable (depends on depth and nerve involvement) |
| Metastatic disease | High, especially with peritoneal or liver spread |
Pain is more common in obstructive cancers of the left colon or sigmoid region, where the stool is firmer and the bowel diameter narrower. In contrast, early right-sided colon cancers may grow significantly before causing pain due to the more spacious cecum.
What Causes Abdominal Pain in This Cancer Type?
The sources of pain in colorectal cancer are multifactorial. They include not only the tumor itself but also effects of treatment, secondary complications, and metabolic shifts.
| Cause Category | Examples |
| Tumor-related | Bowel obstruction, bleeding, ulceration, perforation |
| Inflammatory | Tumor-associated colitis or peritumoral inflammation |
| Treatment-induced | Post-surgical adhesions, radiation enteritis, chemotherapy-related mucositis |
| Metabolic/secondary | Constipation, gas retention, bacterial overgrowth, ascites from colorectal cancer spread |
| Referred Pain | Invasion of pelvic nerves, sacral plexus, or ureters |
Identifying the correct origin is key to selecting the most effective treatment strategy, especially when managing chronic or refractory pain.
When to Take Abdominal Pain Seriously
Not every abdominal ache is a crisis, but in the context of colorectal cancer, specific pain patterns warrant immediate medical attention. Pain that becomes constant, progressively worse, or suddenly severe may signal complications like obstruction, perforation, or infection.
Look out for the following red flags:
| Symptom | Possible Concern |
| Severe cramping after meals | Partial or complete bowel blockage |
| Sudden, sharp, persistent pain | Bowel perforation or peritonitis |
| Fever with abdominal pain | Abscess or tumor-related infection |
| Inability to pass gas or stool | Acute obstruction |
| Pain with rectal bleeding or black stool | Tumor ulceration or upper GI bleeding |
In such cases, emergency imaging (CT scan or abdominal X-ray) is essential. Rapid intervention may prevent life-threatening outcomes.
Diagnostic Tools to Pinpoint the Source
When abdominal pain develops or worsens in a patient with known or suspected colorectal cancer, physicians use a range of diagnostic tools to clarify the cause. The workup often includes a combination of labs and imaging studies.
| Diagnostic Method | Purpose |
| Complete Blood Count (CBC) | Detects anemia or infection |
| CEA and other tumor markers | Tracks colorectal cancer progression |
| Abdominal X-ray | Useful for identifying bowel obstruction |
| CT Scan with contrast | Gold standard for tumor mapping and complications |
| Colonoscopy or Sigmoidoscopy | Direct tumor visualization and biopsy |
| MRI or PET-CT | Evaluates spread, including peritoneal or liver metastases |
In some cases, exploratory laparoscopy is necessary, especially when imaging is inconclusive but the patient has persistent, unexplained pain.
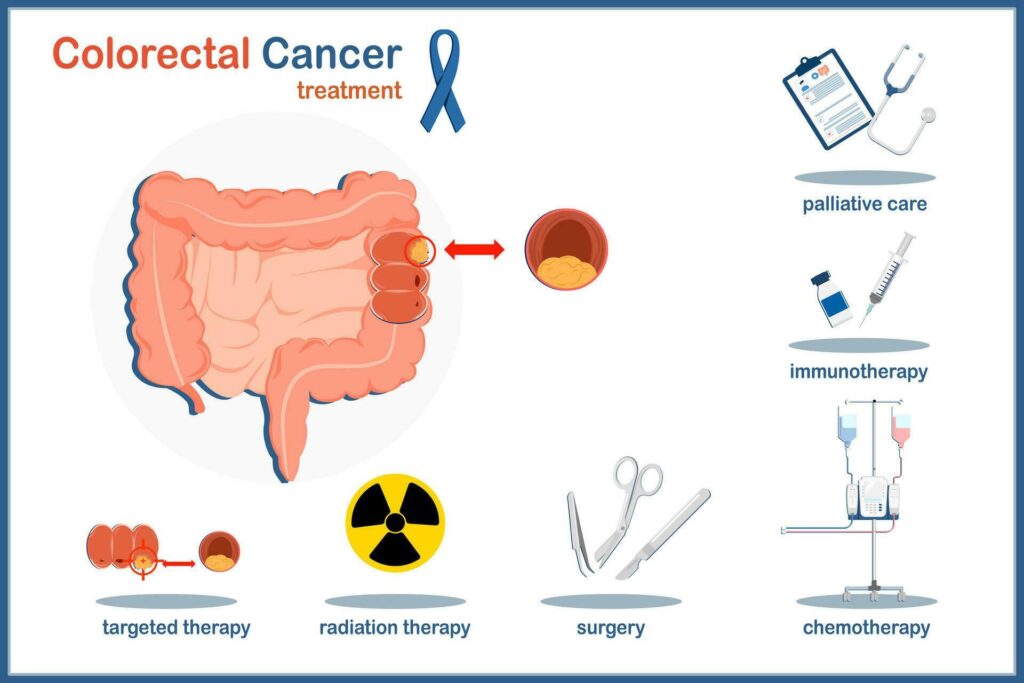
How Pain in Colorectal Cancer Is Treated
Pain management must be personalized. Treatment depends on tumor stage, exact cause of pain, and the patient’s overall condition. In most cases, a combination of medical, procedural, and supportive approaches yields the best results.
| Treatment Type | Indication |
| NSAIDs or acetaminophen | Mild to moderate pain |
| Opioid analgesics | Moderate to severe or chronic cancer pain |
| Antispasmodics (e.g. hyoscine) | Cramping due to bowel spasm |
| Chemotherapy or targeted therapy | To reduce tumor burden |
| Radiation therapy | For localized pain relief in metastasis |
| Surgical resection or bypass | For obstruction or tumor-related pain |
| Palliative care consultation | Multidisciplinary pain and symptom control |
Non-drug interventions such as gentle abdominal massage, guided relaxation, and heat application may also help relieve discomfort.
Can This Pain Be Prevented or Reduced Early?
While not all cancer-related abdominal pain is preventable, several strategies can delay or reduce its severity—especially when implemented early in the course of colorectal cancer.
| Preventive Measure | How It Helps |
| Early screening (e.g. colonoscopy) | Detects tumors before they obstruct |
| Monitoring for early symptoms of colon cancer | Enables prompt treatment |
| Regular bowel management | Prevents constipation-related distension |
| Nutritional support | Reduces gas, bloating, and mucosal irritation |
| Routine imaging follow-up | Catches recurrence or spread early |
Additionally, identifying and managing pain as a dynamic and multifactorial symptom—rather than a fixed issue—empowers both patients and clinicians to adapt care strategies as needed.
Does the Pain Go Away Over Time?

The trajectory of abdominal pain in colorectal cancer varies depending on tumor stage, response to treatment, and any complications that arise. In early-stage disease, pain may completely resolve after surgical resection or effective chemotherapy. Many patients experience significant relief once the tumor is debulked and bowel function is restored.
However, in advanced cases or when the cancer has spread to the peritoneum or nearby organs, the pain may persist and require long-term symptom management. Palliative care can help control pain while improving quality of life. Pain may also fluctuate during cycles of chemotherapy or in response to treatment side effects.
| Scenario | Pain Outcome |
| Post-surgery, early-stage tumor | Often resolves completely |
| Tumor shrinkage after chemotherapy | Pain typically improves or stabilizes |
| Advanced stage with metastasis | Chronic or recurrent pain likely |
| Post-obstruction management | Variable, depends on residual damage |
Monitoring and re-assessing pain regularly is crucial. What begins as treatment-related discomfort may evolve into chronic cancer pain or signal new disease progression.
Insights from Oncologists on Managing Pain
Oncologists stress that abdominal pain should never be dismissed—especially in patients with a colorectal cancer history. According to clinicians, the location, intensity, and pattern of pain often provide the first clues to obstruction, inflammation, or tumor recurrence.
A gastrointestinal oncologist from a major cancer center explains:
“Pain in the lower abdomen or pelvis can tell us a lot. If it’s cramping, we’re thinking about blockage. If it’s sharp and constant, we’re concerned about invasion or nerve compression. Imaging and labs confirm, but it starts with the patient’s description.”
Specialists also highlight the importance of collaborative care: pain management often involves surgeons, medical oncologists, gastroenterologists, and palliative care professionals working in tandem.
Many recommend keeping a daily symptom journal and bringing it to appointments to help tailor treatment adjustments. Timely reporting can mean faster diagnosis of a complication like perforation or infection—both of which may present first with subtle or vague abdominal pain.
15 Questions to Ask Your Doctor About Abdominal Pain in Colorectal Cancer (FAQ)
1. What exactly is causing my abdominal pain?
Understanding the root—whether tumor pressure, treatment effect, or obstruction—guides management.
2. Is this pain a sign that the cancer has grown or spread?
Your doctor may use imaging and blood tests to determine if the pain correlates with progression.
3. Should I get a scan to investigate the cause of pain?
A CT, MRI, or ultrasound can help identify new lesions, obstruction, or inflammation.
4. What type of pain relief do you recommend?
Ask whether NSAIDs, opioids, or other agents like antispasmodics are appropriate for you.
5. Can this pain be controlled without strong medications?
There may be non-opioid options or non-drug methods such as acupuncture or massage.
6. Does pain during bowel movements mean obstruction?
Cramping or straining may signal partial blockage; further testing might be needed.
7. Will chemotherapy help reduce the pain?
Tumor shrinkage often relieves pressure and associated symptoms.
8. Could the pain be from previous surgery or scar tissue?
Post-surgical adhesions are a known cause of chronic abdominal pain.
9. Is this kind of pain common in patients like me?
Your doctor can compare your symptom pattern to known clinical presentations.
10. What red flags should prompt me to seek urgent care?
Symptoms like vomiting, fever, and inability to pass stool may require emergency attention.
11. Could this pain be related to constipation or dietary issues?
Discuss bowel habits and possible triggers with your care team.
12. Will the pain go away after surgery or treatment ends?
Pain resolution depends on individual factors, including tumor type and location.
13. Are there foods I should avoid that worsen the discomfort?
Your provider or dietitian may suggest low-residue or low-gas diets.
14. Is palliative care only for end-stage patients?
No—palliative specialists help manage symptoms at any stage of cancer.
15. How can I track my pain to help you treat it better?
A symptom diary or pain log can be a valuable communication tool.