Mental Health Trends in 2025: Addressing the Global Crisis
Introduction: Mental Health in 2025 — Why It’s a Global Conversation Now
You’ve probably noticed how mental health topics seem more visible than ever before — in news headlines, workplace discussions, even casual chats with friends. But why is mental health suddenly such a widespread concern in 2025? It’s not like mental illness is new, right? It’s been around forever. So what has changed?
Mental health isn’t just about mood swings or stress; it’s the foundation of how we think, feel, and relate to others. It shapes how we handle everyday challenges and long-term struggles alike. And when mental health suffers on a large scale, it affects everything — families, communities, economies. Interestingly, some of the same structural inequities that complicate responses to chronic physical illnesses like malaria also ripple into mental health care — lack of infrastructure, regional disparities, and underfunding all play a part.
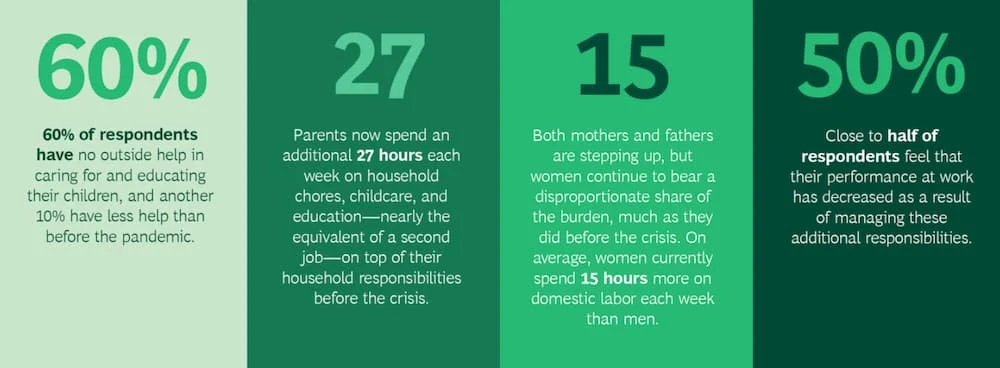
The past several years have thrown some serious curveballs. The COVID-19 pandemic, for instance, upended routines, separated loved ones, and brought uncertainty that lingered long after lockdowns ended. Many people faced isolation and grief in ways that deepened anxiety and depression. On top of that, our fast-paced, always-connected lives come with their own mental toll. Social media might keep us linked, but it can also amplify feelings of loneliness or inadequacy.
And then there’s the broader backdrop: economic instability, climate change, political unrest — all adding layers of chronic stress that quietly wear people down. When you consider how interconnected these forces are, it’s no surprise that mental health challenges have surged globally.
But here’s the paradox: even as more people talk openly about mental health and seek help, the systems designed to support them often struggle to keep up. Stigma, resource shortages, and uneven access continue to block many from getting timely care.
This series will explore the big picture — how mental health trends are evolving worldwide in 2025, what’s driving the crisis, and what promising changes are underway. Whether you’re deeply familiar with mental health or just starting to pay attention, understanding this landscape matters. Because mental health touches every life, whether directly or indirectly.
Have you ever paused to consider how mental wellness influences your daily life, your work, or your relationships? It’s not just an individual issue; it’s a collective one. And as we unpack the data, innovations, and challenges ahead, you’ll see why mental health is shaping the future of global health policy and care.
Epidemiology: Who’s Affected, How Many, and Why It Matters
When we talk about epidemiology, it’s easy to think only of infectious diseases — but mental health disorders follow patterns too, patterns that reveal who is most at risk, where, and why. And understanding these patterns is key to figuring out where to focus resources and how to intervene.
So, how widespread is mental illness today? The numbers are staggering. More than one in eight people worldwide live with some form of mental disorder — that’s over a billion individuals. Conditions like depression and anxiety top the list, affecting hundreds of millions globally. But these are just the cases we know about. Many more go undiagnosed or untreated, often because of stigma or lack of access.
The prevalence of mental health disorders isn’t evenly spread. Young people, especially adolescents and young adults, are experiencing rising rates of anxiety and depression. Some experts suggest that factors like social media pressures, academic expectations, and uncertainty about the future play big roles. At the same time, older adults face challenges like loneliness, cognitive decline, and chronic illnesses that heighten their vulnerability.
Gender also influences risk. Women tend to report higher rates of depression and anxiety, while men have higher rates of substance use disorders and suicide. These differences reflect complex interactions between biology, social roles, and cultural expectations.
Then there are the socioeconomic factors — arguably some of the most powerful drivers. Poverty, job insecurity, and low educational attainment all increase mental health risks. Chronic stress from financial hardship can wear down anyone’s resilience over time. Living in neighborhoods with few opportunities, high violence, or poor housing only compounds the burden.
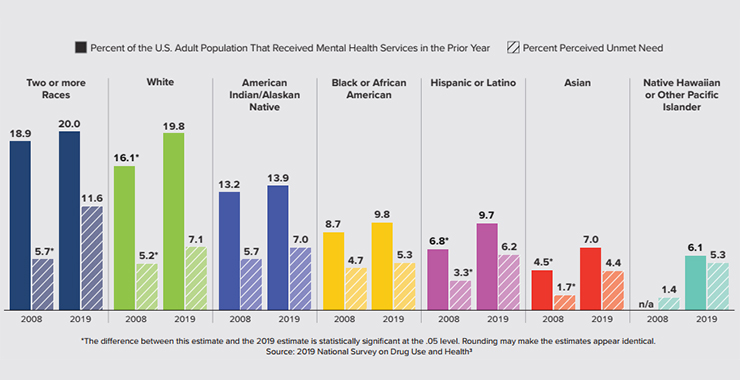
Geography matters too. Low- and middle-income countries face enormous challenges due to limited mental health infrastructure, fewer trained professionals, and stronger stigma in some cultures. But even wealthier countries are not immune, grappling with issues like urban isolation and inequality.
What’s striking is how these factors overlap. For example, a young woman from a low-income urban area may face multiple layers of vulnerability — financial stress, gender-related discrimination, and limited access to care — all interacting to increase risk.
The big question is whether these numbers are getting better or worse. The truth is complex. On one hand, more awareness and better diagnostics mean more people are getting identified and treated than ever before. On the other, prevalence rates for conditions like anxiety and depression seem to be climbing, fueled by the same social and economic pressures we touched on earlier.
This dual reality challenges us to rethink how we measure and respond to mental health needs. Because behind every statistic is a person — a teenager navigating school and social pressures, an adult balancing work and family stress, or an elderly person coping with loneliness.
Recognizing who is most affected and why sets the stage for targeted action — and that’s exactly where this conversation will take us next.
Access to Care: Why Getting Help Isn’t Always Easy (and What We’re Doing About It)
Understanding the scope of mental health challenges is one thing, but the real test lies in whether people can actually get help when they need it. You might assume that by 2025, with all the medical advances and awareness campaigns, accessing mental health care would be easier than ever. Yet, for many, the path to treatment remains tangled in obstacles — a reality that echoes barriers seen in managing other neglected conditions like tick-borne diseases, where geography, education, and systemic blind spots all limit access to timely interventions.
Take a moment to consider your own community or experience. Have you ever noticed how uneven mental health services can be? In many places around the world, specialists like psychiatrists or therapists are in painfully short supply, especially outside major cities. The World Health Organization estimates that in low- and middle-income countries, over three-quarters of people with mental disorders don’t receive any treatment at all. That’s not just a statistic — it’s a reflection of a systemic shortage that leaves millions without basic support.
Why does this shortage persist? Training mental health professionals is a lengthy and resource-intensive process, and many prefer urban or private practice settings with better pay and infrastructure. This concentration leaves rural and marginalized communities especially vulnerable, often relying on overstretched primary care or informal networks that might not be equipped to help.
Cost is another critical barrier. Even in wealthier countries, mental health care can be prohibitively expensive, with insurance gaps and high out-of-pocket fees. This paradox—where those who need help the most often have the least ability to pay—is a major driver of untreated illness.
Then there’s the stubborn weight of stigma. Despite growing awareness and campaigns to normalize mental health struggles, many people still hesitate to seek help out of fear of judgment or shame. This silence can turn suffering inward, delaying treatment and worsening outcomes. It’s a reminder that solving mental health access isn’t just about clinics or medications — it’s about changing hearts and minds.
Navigating the mental health system itself can feel like an obstacle course. Complex referral processes, confusing insurance paperwork, and inconsistent communication between providers make it hard to stay engaged, especially when you’re already struggling. Imagine the frustration or discouragement someone might feel trying to make sense of this maze.
But there are bright spots. In 2025, innovations like telepsychiatry and digital therapeutics are transforming how care is delivered. Virtual therapy sessions and mental health apps bring support to people’s phones, removing geographic and time barriers that once seemed insurmountable. Of course, digital care isn’t a silver bullet — not everyone has reliable internet or feels comfortable with technology — but it’s an important step forward.
At the same time, integrating mental health into primary care is gaining momentum. Since most people see their primary care doctor regularly, training these providers to identify and manage common mental health issues means more people can get help early, without the wait times and stigma often associated with specialist care.
Community-based models are also making a difference. By involving trained lay counselors and peer support networks, care can become more culturally relevant and accessible, bridging gaps where formal services fall short. These approaches don’t just treat illness—they build social connections, reduce stigma, and empower communities.
Policy efforts and funding increases are beginning to support these changes, recognizing that investing in mental health is not just a moral imperative but an economic one. Healthier populations are more productive, more resilient, and better able to contribute to society.
Yet challenges remain. How do we ensure digital tools reach those without smartphones or stable internet? How do we protect privacy in an increasingly digital health landscape? And how can we scale training programs fast enough to meet demand?
These aren’t easy questions, but addressing them head-on is essential if we want to make real progress.
So when you think about access to mental health care today, it’s clear we’ve come far but still have a long way to go. The journey to equitable, affordable, stigma-free care is ongoing—and everyone, whether patient, provider, policymaker, or community member, has a role to play.
Innovations in Treatment: How Mental Health Care Is Changing in 2025
By now, you’ve seen how widespread mental health challenges are and how tough it can be for people to access care. But there’s reason for optimism — because 2025 is a time of remarkable innovation in how mental health is treated. New technologies, fresh approaches, and evolving medicines are reshaping the way we understand and manage mental health disorders.
One of the biggest game-changers has been the rise of telepsychiatry and digital therapeutics. Imagine being able to connect with a therapist or psychiatrist from your living room, without the stress of travel or long waitlists. This isn’t just convenience; it opens doors for people in rural areas, those with mobility challenges, or anyone juggling a busy schedule. Plus, mental health apps that offer guided meditation, mood tracking, or cognitive behavioral therapy exercises put powerful tools directly into people’s hands, often at a fraction of the traditional cost.
Of course, these tools aren’t meant to replace human connection, but they can complement in-person care and fill gaps where services are limited. Still, challenges remain around privacy, digital literacy, and ensuring these apps are evidence-based, but the progress is undeniable.
Beyond digital advances, we’re seeing exciting progress in pharmacotherapy — the medicines used to treat mental health conditions. After decades of relying on a handful of drugs, researchers are developing new classes of medications with fewer side effects and better effectiveness. For example, breakthroughs in psychedelics like psilocybin and ketamine are gaining scientific and regulatory attention as potential treatments for depression and PTSD, often when conventional therapies fall short. These developments signal a shift toward more personalized, targeted treatments.
On the psychotherapy front, innovations in delivery and approach are also flourishing. Therapies are becoming more tailored to individual needs, blending traditional talk therapy with techniques like mindfulness, trauma-informed care, and neurofeedback. The goal is to meet people where they are, recognizing that mental health is deeply personal and complex.
But it’s not just about new tools — it’s about integrating these advances into systems that are accessible and compassionate. The future of mental health treatment in 2025 is increasingly holistic, combining medication, therapy, community support, and technology in ways that respect each person’s unique experience.
Have you encountered any new mental health tools or therapies yourself? Maybe a smartphone app that helped track your mood or a teletherapy session that felt surprisingly effective? These innovations aren’t just buzzwords — they’re changing lives and expanding what’s possible in mental health care.
Integration with Primary Care: Why Mental Health Can’t Stay Separate
If you think about your own visits to a doctor, you probably picture a primary care provider—your family doctor, general practitioner, or nurse practitioner—handling everything from your flu shot to managing chronic conditions like diabetes. But have you ever wondered how mental health fits into this picture? Surprisingly, in many places, mental health care has traditionally been siloed away from primary care, treated almost like a specialty branch that you have to seek out separately.
That separation creates a real problem. Mental health issues rarely exist in isolation. They influence and are influenced by physical health, lifestyle, and social factors. When mental health is disconnected from the frontline of healthcare, many people fall through the cracks.
In 2025, one of the most promising shifts is bringing mental health care right into primary care settings. This integration means your primary care provider isn’t just treating your blood pressure or back pain but is also equipped to screen for depression, anxiety, substance use, and other common mental health conditions.
Why is this so important? For one, most people see their primary care provider regularly, even if they never step foot in a mental health clinic. That makes primary care a natural place to catch mental health concerns early, before they spiral into crises. It also helps reduce stigma — going to your family doctor doesn’t carry the same weight of “I’m sick” or “there’s something wrong with me” that visiting a psychiatrist might.
But integration isn’t as simple as just adding a checklist to a routine visit. It requires training primary care providers to recognize and manage mental health problems effectively. Many doctors feel underprepared for this role. Mental health diagnoses can be complex, symptoms overlap, and treatment plans often need careful monitoring and adjustment. So, ongoing education and support are essential.
One model gaining traction is the collaborative care approach. In this setup, primary care providers work closely with mental health specialists, care managers, and sometimes social workers to deliver coordinated care. Imagine it like a team sport, where each player brings their expertise, but everyone is focused on the same goal: the patient’s overall well-being. Studies show that collaborative care improves outcomes, especially for depression and anxiety, while also being cost-effective.
From a practical standpoint, what does this mean for patients? Instead of waiting months for a psychiatrist appointment, you might get immediate screening and support during your next doctor’s visit. If needed, your provider can refer you quickly and stay in the loop with specialists. There might also be in-house counselors or mental health nurses who follow up regularly.
Still, the road to fully integrated care isn’t without bumps. Electronic health records often don’t communicate well between primary care and mental health services, and privacy concerns can limit how much information is shared. Funding models and insurance reimbursements don’t always support integrated services either.
But these challenges are being tackled. Governments and health systems recognize that integration isn’t just a “nice-to-have” — it’s essential for improving access and outcomes. Many training programs now include mental health modules for primary care professionals. Pilot projects are proving the effectiveness of collaborative teams. Technology is evolving to facilitate better data sharing while protecting privacy.
If you’ve ever felt frustrated by bouncing between different doctors for physical and mental health issues, integration could be a game-changer. It brings care closer to where people already are and makes mental health a routine part of overall health — because, frankly, it should be.
Policy and Advocacy: Changing Systems, Changing Lives
You might wonder, with all these challenges in mental health care—access gaps, stigma, workforce shortages—what role do governments and organizations actually play? After all, no single doctor, therapist, or community group can solve a crisis this vast alone. This is where policy and advocacy come into the spotlight, shaping the framework that either supports or stalls progress.
Think of policy as the blueprint for how mental health resources are allocated, what laws protect patients, and how services are structured. Advocacy is the engine pushing those blueprints forward, often led by passionate individuals, nonprofits, or even people with lived experience demanding change.
Why Does Policy Matter So Much?
Without strong policy backing, even the best treatments and innovations risk falling short. Imagine a city with plenty of therapists but no funding to subsidize care for low-income families, or a country where mental health is excluded from health insurance coverage altogether. That’s why governments need to prioritize mental health as a fundamental part of public health.
Globally, we’ve seen progress. In recent years, many countries have launched national mental health strategies aimed at increasing funding, integrating services, and reducing stigma. The WHO’s Mental Health Action Plan, updated regularly, serves as a global guidepost, encouraging nations to set measurable goals. But policy adoption doesn’t happen overnight, and implementation often lags behind ambition.
Practical Insights from the Field
From an expert’s perspective, one of the most effective policy moves is increasing dedicated mental health budgets. Many countries still allocate less than 2% of their health budgets to mental health, despite its huge burden. Shifting even a small percentage more funding can dramatically expand services, train professionals, and support community programs.
Another practical lever is legislative reforms. For example, enacting parity laws that require insurance companies to cover mental health on par with physical health can remove financial barriers for millions. Countries that have enforced these laws see increased treatment uptake and better outcomes.
Advocacy groups also play a critical role in holding governments accountable and pushing for reforms. Grassroots campaigns can amplify voices that otherwise go unheard, especially from marginalized communities. When people with lived experience share their stories publicly, it humanizes mental health issues and chips away at stigma.
But advocacy isn’t just about raising awareness—it’s about shaping policies that are culturally sensitive and locally relevant. A “one size fits all” policy rarely works across diverse populations. Effective advocacy groups understand their communities deeply and tailor recommendations accordingly.
Challenges and the Road Ahead
Still, there are hurdles. Political will can fluctuate, especially when mental health competes with other pressing issues like infectious diseases or economic crises. Policy continuity is fragile—changes in leadership or budget priorities can stall progress. And even the best policies need robust systems for monitoring and evaluation, which are often missing.
What’s promising, though, is the increasing recognition that mental health is essential to economic development and social stability. Governments are starting to see mental health investment not as a cost, but as a driver of workforce productivity and societal resilience. This shift is encouraging more strategic, long-term planning.
So, when you think about the big picture of mental health in 2025, policy and advocacy are the engines that can transform individual advances into widespread change. Without them, innovations and care models struggle to reach everyone who needs them. This is especially true when we consider overlapping pressures like rising antimicrobial resistance — an issue exemplified by threats such as Candida auris, which remind us how strained health systems can falter across multiple domains if proactive policy and equitable investment aren’t prioritized.
Recent Developments (2025–2026): What’s New, What’s Working, and What’s Next
By now, you’ve got a solid understanding of the global mental health landscape — the challenges, the gaps, and the big-picture policies. But mental health care isn’t static. In fact, the past couple of years have been a whirlwind of fresh programs, groundbreaking research, and shifts in practice that are actively reshaping how we approach mental wellness around the world.
You might ask, what exactly has changed recently? Are these just incremental improvements, or are we talking about something more transformative?
New Programs and Services: Innovation Meets Reality
One of the most exciting trends is the scaling up of community-based mental health programs. Take, for instance, countries in Sub-Saharan Africa and South Asia, where mental health professionals are scarce. NGOs and governments have teamed up to train community health workers and lay counselors to deliver basic psychological support. This approach isn’t just theoretical—it’s being implemented at scale and showing promising outcomes in reducing depression and anxiety symptoms.
Closer to home, many health systems in Europe and North America are expanding integrated care models, embedding mental health specialists directly within primary care clinics, schools, and workplaces. This proximity makes mental health care more routine and less intimidating. It also means people get quicker, more coordinated support.
Another notable development is the rapid growth of digital mental health platforms, which have evolved from simple apps into sophisticated ecosystems offering everything from AI-guided therapy chatbots to remote monitoring of symptoms through wearable devices. The pandemic accelerated this shift, but these tools have proven their staying power. They’re increasingly being covered by insurance and endorsed by clinicians, signaling mainstream acceptance.
Cutting-Edge Research Shaping Practice
Behind these service innovations lies a wealth of new research that’s changing what clinicians consider “best practice.” For example, studies on precision psychiatry—where treatment is tailored to an individual’s genetics, brain imaging, and lifestyle—are beginning to move from the lab to the clinic. Although still early, this promises more personalized and effective treatments with fewer side effects.
Research on the therapeutic potential of psychedelics has also advanced rapidly. Clinics in countries like Canada, the US, and parts of Europe are running controlled programs using psilocybin-assisted therapy for treatment-resistant depression and PTSD. It’s not just hype; emerging evidence suggests these approaches can offer profound, lasting improvements for some patients.
On the psychotherapy front, trauma-informed care models have become standard in many places, recognizing how past trauma shapes mental health and requiring providers to adapt their approach accordingly. This isn’t just about therapy styles—it’s influencing hospital policies, schools, and even law enforcement training.
Practical Takeaways for Clinicians and Caregivers
For healthcare providers, keeping up with these developments can feel overwhelming. What should you prioritize? How do you balance emerging tools with established methods?
A practical approach is to stay grounded in evidence-based practice, while remaining open to integrating new modalities cautiously and thoughtfully. Collaborating across disciplines—psychiatry, psychology, social work, primary care—enhances care quality. Also, embracing technology thoughtfully, such as telehealth and symptom monitoring apps, can extend reach and improve patient engagement.
If you’re a caregiver or someone supporting a loved one, these developments mean there are more options than ever. Don’t hesitate to ask providers about digital tools, integrated care programs, or new therapies. Being proactive and informed helps tailor support to the individual’s needs.
What’s on the Horizon?
Looking forward, the biggest challenge—and opportunity—is scaling these innovations equitably. How do we ensure rural communities and low-income countries benefit from precision medicine or digital tools? How do we maintain quality while expanding access? Addressing these questions will define the next phase of the global mental health response.
Also, watch for continued emphasis on data-driven decision making. Governments and organizations are investing in better mental health surveillance systems to track outcomes and adapt programs in real time. This feedback loop is critical for sustainable progress.
So, as you can see, 2025 and beyond aren’t just about talking more about mental health—they’re about putting new ideas into action. This dynamic phase of development gives reason for cautious optimism, but it also reminds us how much work remains.
Cultural and Societal Considerations: Why Context Matters More Than Ever
When we talk about mental health, it’s easy to think about diagnoses, treatments, and policies — the clinical and systemic sides of the issue. But mental health doesn’t exist in a vacuum. It’s deeply embedded in culture, community, and society. Understanding that context is not just a bonus; it’s essential for real progress.
Have you ever noticed how mental health conversations can vary wildly between cultures? What’s accepted, what’s stigmatized, and how people seek help can look completely different depending on where you are or who you talk to. For instance, in some communities, emotional struggles are expressed through physical symptoms — headaches, stomachaches — rather than what we might label as “depression” or “anxiety.” Without appreciating this, clinicians might miss the true nature of someone’s suffering.
Stigma: The Invisible Barrier
Stigma remains one of the most persistent cultural barriers worldwide. Even in places with advanced health systems, people may avoid seeking help because of shame or fear of discrimination. But stigma isn’t uniform; it changes shape based on cultural beliefs about mental illness, gender roles, religion, and social status.
What’s interesting — and hopeful — is how community-based interventions are showing real promise in breaking down these walls. Programs that involve local leaders, faith groups, or respected elders can shift attitudes in ways that top-down messaging cannot. When a trusted figure says, “It’s okay to talk about mental health,” it opens doors that policy alone can’t unlock.
Tailoring Interventions to Culture
From an expert’s standpoint, one of the biggest mistakes in global mental health has been trying to export Western models without adaptation. Evidence-based treatments like cognitive behavioral therapy (CBT) are effective but often need cultural tailoring to resonate.
For example, some cultures emphasize collective wellbeing over individualism. Therapy that focuses solely on personal achievement or self-expression might miss the mark. Instead, approaches that integrate family, community, or spiritual dimensions tend to be more acceptable and effective.
This means training providers not just in clinical skills, but in cultural humility and local knowledge. It also means involving communities in designing and delivering mental health services — a process sometimes called co-production. When people see their values and voices reflected in care, engagement and outcomes improve.
Addressing Social Determinants Through Community
Mental health is tightly linked to social and economic conditions — poverty, discrimination, violence, education, and housing all play roles. Community-based interventions that address these broader determinants are increasingly recognized as critical.
Programs that combine mental health support with job training, housing assistance, or violence prevention tackle the root causes, not just symptoms. This holistic view is especially important in marginalized communities, where multiple challenges intersect.
Practical Takeaways: What Can Clinicians and Advocates Do?
If you’re a clinician, approaching mental health with cultural sensitivity isn’t just ethical; it’s effective. Take time to understand a patient’s cultural background, belief systems, and support networks. Use that insight to adapt treatment plans and communication.
For advocates and policymakers, investing in community partnerships is key. Supporting grassroots organizations that reflect and respect local culture can make all the difference in reducing stigma and improving access.
And for anyone curious about mental health globally, remember: one size never fits all. Appreciating cultural nuance isn’t a distraction — it’s a necessity.
Frequently Asked Questions (FAQ)
1. Why is mental health considered a global crisis in 2025?
Mental health challenges have surged worldwide due to factors like the pandemic’s aftermath, social isolation, economic stress, and environmental concerns. Increased awareness has brought these issues to light, revealing gaps in care and the vast number of people affected.
2. How prevalent are mental health disorders, and who is most at risk?
Over one in eight people globally live with mental health conditions, with depression and anxiety being the most common. Young people, women, those in low socioeconomic groups, and residents of low- and middle-income countries face higher risks due to various social, economic, and cultural factors.
3. What are the main barriers to accessing mental health care?
Key barriers include a shortage of mental health professionals, high costs, stigma, fragmented healthcare systems, and geographic disparities. These factors make it difficult for many to receive timely and effective treatment.
4. How is technology influencing mental health treatment today?
Telepsychiatry, mental health apps, and digital therapeutics are expanding access and offering flexible treatment options. While promising, these tools must be evidence-based, secure, and accessible to avoid widening disparities.
5. Why is integrating mental health into primary care important?
Since most people regularly visit primary care providers, embedding mental health screening and treatment there enables early detection, reduces stigma, and improves coordination, making care more accessible and holistic.
6. What role do policy and advocacy play in improving mental health care?
Government policies set funding priorities, regulate insurance coverage, and shape service delivery. Advocacy drives these policies forward, amplifies marginalized voices, and pushes for culturally sensitive, equitable mental health reforms.
7. What recent developments have shaped mental health care in 2025 and beyond?
Scaling community-based care, advancements in pharmacotherapy (including psychedelics), integration of technology, and precision psychiatry are key trends influencing current practice and research.
8. How do culture and society affect mental health and treatment?
Cultural beliefs shape how mental illness is expressed, understood, and treated. Tailoring interventions to local contexts and addressing social determinants through community involvement are critical for effective care and stigma reduction.
Conclusion: Progress Made, Challenges Ahead, and the Path Forward
Looking across the mental health landscape in 2025, it’s clear we’re at a pivotal moment. On one hand, awareness and innovation have never been greater. Digital tools, new therapies, integrated care models, and policy momentum offer real hope. Communities worldwide are pushing back against stigma and building support systems that resonate culturally and socially.
Yet, the crisis remains daunting. Millions still lack access to care, stigma persists, and the social and economic roots of mental distress run deep. The journey toward truly equitable, effective mental health care is ongoing—and it demands commitment from all sectors: healthcare providers, policymakers, communities, and individuals alike.
What can you take away from this? Mental health is everyone’s business. Whether you’re a clinician, an advocate, a policymaker, or simply someone who cares about the wellbeing of those around you, your voice and actions matter. Keep asking questions, supporting innovation, and fostering compassion.
Together, progress is possible—not just in treating illness but in promoting mental wellness as a fundamental human right and cornerstone of thriving societies.