Pins and Needles in Legs: Common Causes and Treatments
Pins and Needles in the Legs
What Is Paresthesia?
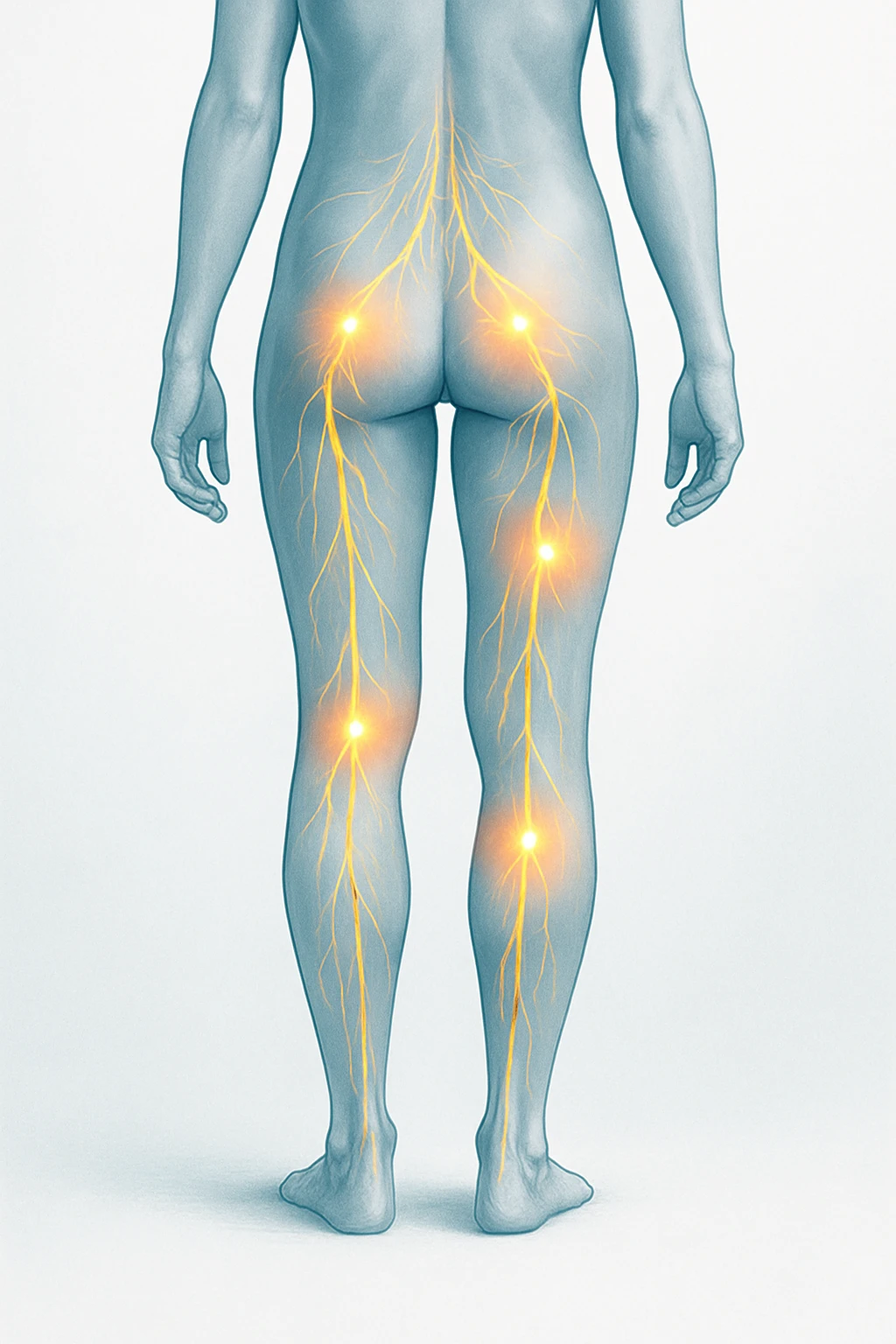
The familiar tingling or prickling feeling often described as pins and needles in the legs is known medically as paresthesia. It is an unusual sensory experience that differs from normal touch or pain. Instead of detecting a stimulus like pressure or temperature, the nerves send spontaneous signals that the brain interprets as tingling, buzzing, or prickling sensations.
Paresthesia occurs when the normal communication between nerves and the brain is momentarily disrupted. This can happen when a nerve is compressed, irritated, or deprived of adequate blood flow. Most people experience this occasionally, such as when a leg “falls asleep” after sitting in one position for too long.
- Key characteristics: tingling, prickling, or buzzing sensations.
- Common triggers: temporary nerve compression or restricted blood flow.
- Typical duration: resolves within minutes once pressure is relieved.
Why It Happens
Short episodes of tingling in the legs commonly occur when pressure or awkward posture temporarily squeezes a nerve or limits circulation. The affected nerve fibers stop transmitting signals normally, leading to the characteristic pins-and-needles feeling. Once movement or blood flow returns, the nerve resumes normal function, and the sensation fades within minutes.
Although these transient cases are harmless, similar sensations can also arise when nerves are affected by underlying conditions such as chronic compression, metabolic imbalances, or systemic illness. In those situations, tingling may occur more frequently or persist longer, signaling that the nerves are under ongoing strain rather than short-term pressure.
Temporary vs. Persistent Tingling
Doctors classify paresthesia as transient or chronic. Transient paresthesia is short-lived and fully reversible-typically caused by nerve or blood vessel compression that resolves once the body changes position or circulation improves. It is a normal response and rarely indicates disease.
| Type | Typical Duration | Common Cause | Indication |
|---|---|---|---|
| Transient Paresthesia | Minutes | Temporary nerve compression or poor posture | Normal, resolves on its own |
| Chronic Paresthesia | Persistent or recurring | Underlying disease or nerve damage | May require medical evaluation |
In contrast, chronic or recurrent paresthesia lasts longer or returns regularly and may point to a medical problem affecting nerve health or metabolism. Conditions such as diabetes or persistent nerve injury can lead to ongoing pins and needles in the legs. Recognizing whether tingling is brief or persistent helps determine whether simple posture changes or medical evaluation is needed.
Common Causes of Pins and Needles in the Legs
Short-Term or Benign Causes
Short episodes of tingling in the legs are often linked to temporary changes in posture or pressure on a nerve. When you sit cross-legged, squat, or remain in one position for a long time, pressure can build on the peripheral nerves or local blood vessels. This briefly disrupts normal nerve signaling, leading to the tingling or prickling sensation often described as the leg “falling asleep.”
- Sitting or standing in one position for a long time
- Crossing the legs or squatting
- Pressure on peripheral nerves or local blood vessels
These benign cases of pins and needles typically fade within a few minutes after movement resumes and circulation improves. They are a normal physiological response rather than a sign of disease. Gentle stretching or repositioning usually restores normal sensation once pressure is released and blood flow returns to the affected area.
Chronic and Systemic Causes
When tingling in the legs persists or recurs frequently, it may reflect an underlying medical condition affecting nerve or metabolic function. One of the most common causes is peripheral neuropathy-a type of nerve damage that can develop over time. Peripheral neuropathy may result from diabetes, chronic alcohol misuse, exposure to toxins, certain medications, kidney disease, or deficiencies in vitamins such as B12.
- Peripheral neuropathy: Linked to diabetes, alcohol misuse, or toxin exposure
- Kidney disease: Can lead to buildup of toxins affecting nerve health
- Vitamin deficiencies: Especially low vitamin B12 levels
- Endocrine disorders: Diabetes and thyroid dysfunction that alter nerve metabolism
Other systemic factors can also play a role. Endocrine and metabolic disorders, including diabetes and thyroid dysfunction, may alter nerve metabolism and blood flow, leading to persistent paresthesia in the legs. In these cases, the sensation tends to last longer and may be accompanied by numbness, burning, or weakness, depending on the extent of nerve involvement.
Nerve and Spine-Related Factors
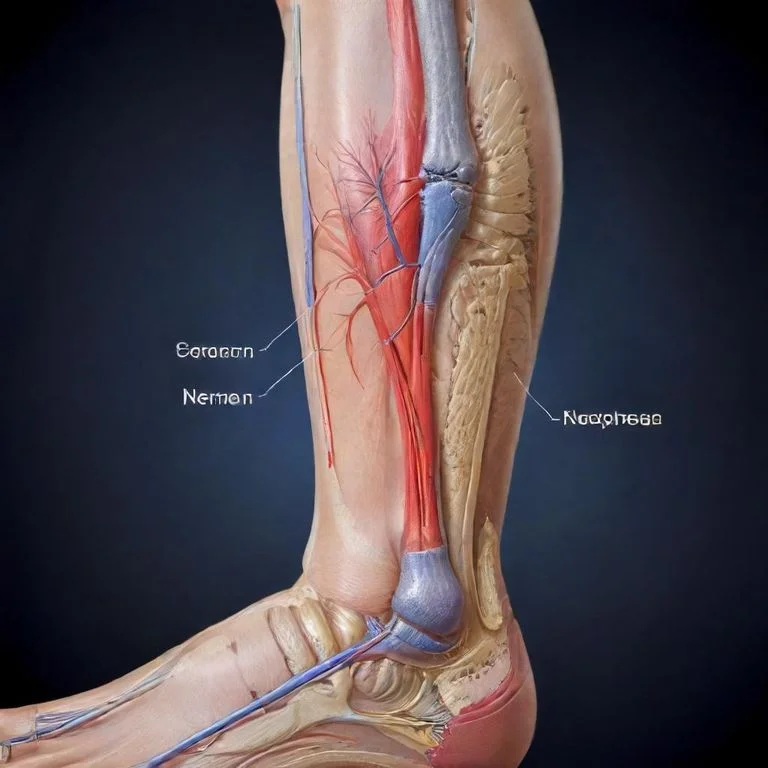
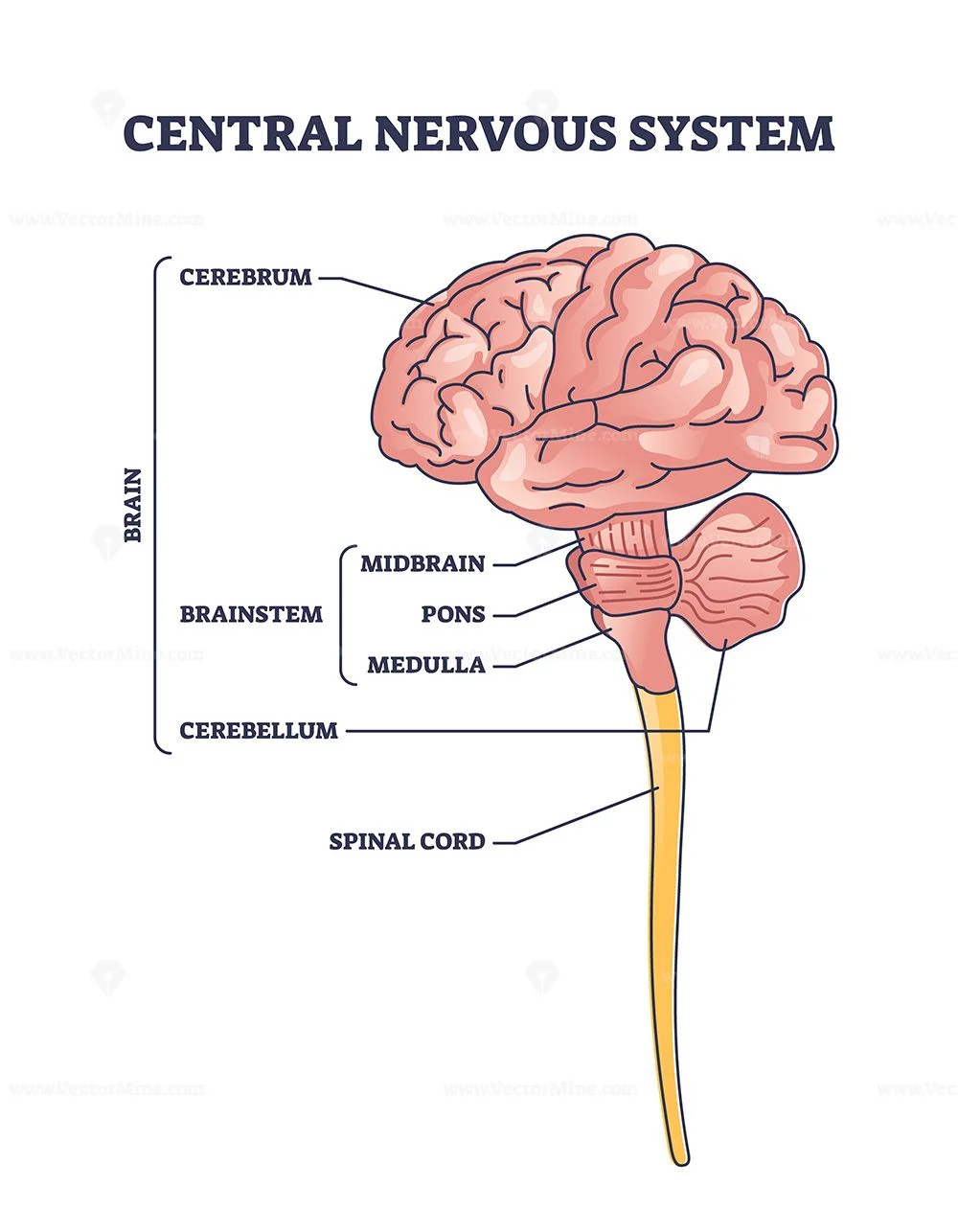
Problems affecting the spine or the pathways of the nerves can also produce tingling sensations. Spinal degenerative disease, disc herniation, or spinal stenosis may compress the nerve roots that exit the spinal cord and travel to the legs. This compression can cause radiating tingling or numbness along the course of the affected nerve, sometimes felt on only one side of the body.
| Condition | Main Mechanism | Typical Sensation |
|---|---|---|
| Spinal stenosis | Compression of spinal nerves | Tingling or numbness in both legs when standing or walking |
| Disc herniation | Pressure on a single nerve root | Sharp, radiating tingling down one leg |
| Localized nerve entrapment | Compression or irritation of a specific peripheral nerve | Focal tingling or numbness in a defined area |
In some cases, localized nerve entrapment-where a single nerve becomes compressed or irritated-can create similar symptoms confined to a specific area. These nerve-related causes are distinct from circulation issues, though they may coexist. Persistent or worsening tingling of this nature often warrants medical evaluation to determine the exact source of compression or injury.

When to Worry: Red Flags and Medical Evaluation
When to See a Doctor
Most tingling in the legs is temporary and harmless, but some patterns deserve closer attention. Progressive weakness, loss of coordination, or difficulty walking alongside tingling may signal a more significant nerve or spinal problem. Likewise, numbness that spreads or persists despite rest can indicate underlying nerve damage or metabolic disease that requires medical assessment.
Red Flags: When Tingling Needs Urgent Care
- Sudden numbness or weakness on one side of the body
- Difficulty walking or maintaining balance
- Severe back pain accompanied by bladder or bowel problems
- Rapid worsening or spreading of symptoms
What to Expect at the Clinic
When you visit a healthcare provider for persistent or unexplained pins and needles in the legs, the doctor will begin by asking detailed questions about your symptoms. The core assessment focuses on onset, duration, distribution, and symmetry-whether one or both legs are affected-and any triggers or relieving factors. They may also review medical history, medications, substance use, and family history to identify possible contributors.
A neurological examination is then performed to assess sensation, muscle strength, reflexes, coordination, and walking pattern. These findings help localize which part of the nervous system might be affected, whether in the spine, peripheral nerves, or elsewhere.
Tests That May Be Ordered
If the initial evaluation suggests an underlying medical condition, your doctor may order laboratory or diagnostic tests. Typical blood tests include:
- Glucose or HbA1c – to check for diabetes
- Complete blood count (CBC) – to evaluate general health and rule out anemia or infection
- Basic metabolic panel – to assess kidney and electrolyte function
- Vitamin B12 levels – to detect deficiencies affecting nerve health
- Thyroid-stimulating hormone (TSH) – to assess thyroid function
For more complex or chronic cases, additional studies such as nerve conduction tests or spinal imaging may be considered. These investigations help pinpoint the exact cause of nerve dysfunction and guide appropriate treatment.
Treating and Managing Leg Tingling
Targeting the Underlying Cause
Effective management of pins and needles in the legs begins with identifying and addressing its underlying cause. In many cases, the sensation results from reversible conditions that can be corrected with targeted treatment. For example, improving blood sugar control in people with diabetes can help prevent further nerve irritation. Similarly, restoring normal vitamin levels-particularly vitamin B12-may reverse symptoms caused by nutritional deficiencies.
- Improve blood sugar control to protect nerve health.
- Correct vitamin deficiencies such as vitamin B12.
- Stabilize thyroid or kidney function when imbalances affect nerves.
- Adjust medications or address metabolic disorders as guided by a physician.
When endocrine or metabolic conditions such as thyroid imbalance or kidney disease contribute to nerve dysfunction, stabilizing those disorders is central to symptom control. Medical treatment may involve adjusting medications, optimizing chronic disease management, or correcting metabolic abnormalities to promote healthier nerve signaling and prevent progression of tingling sensations.
Relieving Nerve Symptoms
When tingling stems from nerve injury or chronic neuropathy, doctors often combine medication and supportive therapies to relieve discomfort. Pharmacologic options for neuropathic pain are prescribed according to clinical guidelines and may reduce tingling, burning, or electric sensations associated with nerve damage. Non-pharmacologic measures such as physical therapy, massage, or gentle stretching can also help improve muscle strength and circulation around affected nerves.
- Medication to relieve neuropathic discomfort
- Physical therapy and massage for improved circulation
- Stretching and ergonomic adjustments to ease nerve pressure
In mechanical or posture-related cases, ergonomic adjustments-like changing sitting positions, modifying work setups, or using supportive seating-can reduce ongoing nerve pressure. These strategies prevent recurring symptoms and encourage better long-term nerve health without the need for intensive medical intervention.
At-Home Support
For mild or intermittent tingling, simple lifestyle adjustments can make a meaningful difference. Regular movement breaks during long periods of sitting, light stretching, and good posture help maintain healthy blood flow and reduce temporary nerve compression. Many people find that gentle leg exercises or short walks relieve transient sensations caused by inactivity.
- Take short movement breaks when sitting for long periods.
- Incorporate gentle stretching or walking into daily routines.
- Maintain good posture and avoid tight clothing that restricts circulation.
Home management should focus on consistency-maintaining good posture, avoiding tight clothing that restricts circulation, and keeping legs active throughout the day. While these measures support nerve health, persistent or worsening symptoms should always be evaluated by a healthcare professional to ensure appropriate diagnosis and treatment.

Preventing Recurrence and Supporting Long-Term Nerve Health
Healthy Habits for Nerve Care
Protecting nerve health over the long term starts with maintaining overall wellness and addressing reversible causes of nerve irritation. For people with diabetes or metabolic conditions, keeping blood sugar levels well controlled is essential to prevent or slow nerve damage. Similarly, correcting vitamin deficiencies-especially vitamin B12-can improve or stabilize nerve function and reduce recurring tingling sensations.
- Maintain healthy blood sugar levels if you have diabetes or metabolic conditions.
- Ensure adequate vitamin intake, especially vitamin B12.
- Eat a balanced diet rich in nutrients and stay hydrated.
- Engage in regular physical activity to improve circulation and nerve oxygenation.
Balanced nutrition, hydration, and consistent physical activity support healthy circulation, helping nerves receive the oxygen and nutrients they need. These habits are particularly important for older adults and individuals at higher risk for peripheral neuropathy due to chronic illnesses or medication effects.
Posture and Movement Tips
Mechanical or posture-related tingling is often preventable through simple daily adjustments. Avoid sitting or standing in one position for too long, as prolonged pressure on nerves or blood vessels can trigger temporary numbness or pins and needles in legs. Stretching your legs periodically, shifting weight during long standing periods, and using supportive seating can relieve pressure points and promote better blood flow.
- Take short movement breaks throughout the day.
- Shift weight or change positions when standing for long periods.
- Use chairs and desks adjusted to a comfortable height.
- Encourage children to stretch or move after sitting still.
For desk work or study sessions, ensure that chairs and desks are set to a comfortable height to prevent unnecessary leg compression. Encouraging both children and adults to move regularly throughout the day helps maintain nerve health and lowers the likelihood of recurring sensations of pins and needles in the legs.
Questions Parents Often Ask
Parents sometimes notice their children mentioning that their legs feel tingly or “asleep.” Occasional tingling after sitting cross-legged or staying still is normal and goes away quickly with movement. However, if a child frequently experiences unexplained tingling, weakness, or balance changes, it’s a good idea to discuss it with a healthcare provider to rule out underlying issues.
In most cases, pins and needles are temporary and harmless, but consistent healthy routines-such as movement breaks, good posture, and a balanced diet-help keep nerves functioning well and reduce the chance of recurrence over time.

Frequently Asked Questions About Pins and Needles in the Legs
- Is it normal to feel pins and needles in the legs after sitting?
- Yes. Temporary tingling after sitting or crossing your legs is common and usually results from brief pressure on nerves or reduced blood flow. It typically fades once you move.
- When does leg tingling become a medical concern?
- Seek medical attention if tingling is persistent, spreads, or is accompanied by weakness, pain, or balance problems. These symptoms can suggest nerve or spinal involvement.
- Can poor circulation cause pins and needles in the legs?
- Yes. Reduced blood flow, such as from peripheral arterial disease, may cause tingling, cramping, or leg weakness, especially during walking or exertion.
- What medical conditions commonly lead to chronic tingling?
- Chronic or recurring tingling often relates to diabetes, thyroid disease, vitamin B12 deficiency, or peripheral neuropathy caused by nerve damage over time.
- How do doctors determine the cause of persistent tingling?
- Clinicians evaluate symptom patterns and medical history and may order blood tests for glucose, vitamin B12, and thyroid function, or imaging and nerve studies if needed.
- Can posture or work habits make tingling worse?
- Yes. Staying in one position too long or sitting with poor ergonomics can compress nerves. Regular movement and supportive seating reduce recurrence.
- Is leg tingling ever linked to spinal problems?
- Conditions like disc herniation or spinal stenosis can compress nerve roots, causing radiating tingling, numbness, or pain down one or both legs.
- Do vitamin deficiencies really cause pins and needles?
- They can. Low vitamin B12 affects nerve function and is a known cause of leg tingling, particularly in older adults or those with absorption issues.
- Can exercise help reduce tingling sensations?
- Gentle activity and stretching improve circulation and can reduce mild, posture-related tingling. Regular movement supports long-term nerve and vascular health.
- What should parents do if a child often feels tingling in their legs?
- Occasional tingling from sitting still is normal, but frequent or unexplained episodes with weakness or balance issues should be checked by a doctor.