Ear Pain Symptoms, Diagnosis, and When to Seek Care
Ear Pain: Understanding Its Causes and Importance
Epidemiology and Burden
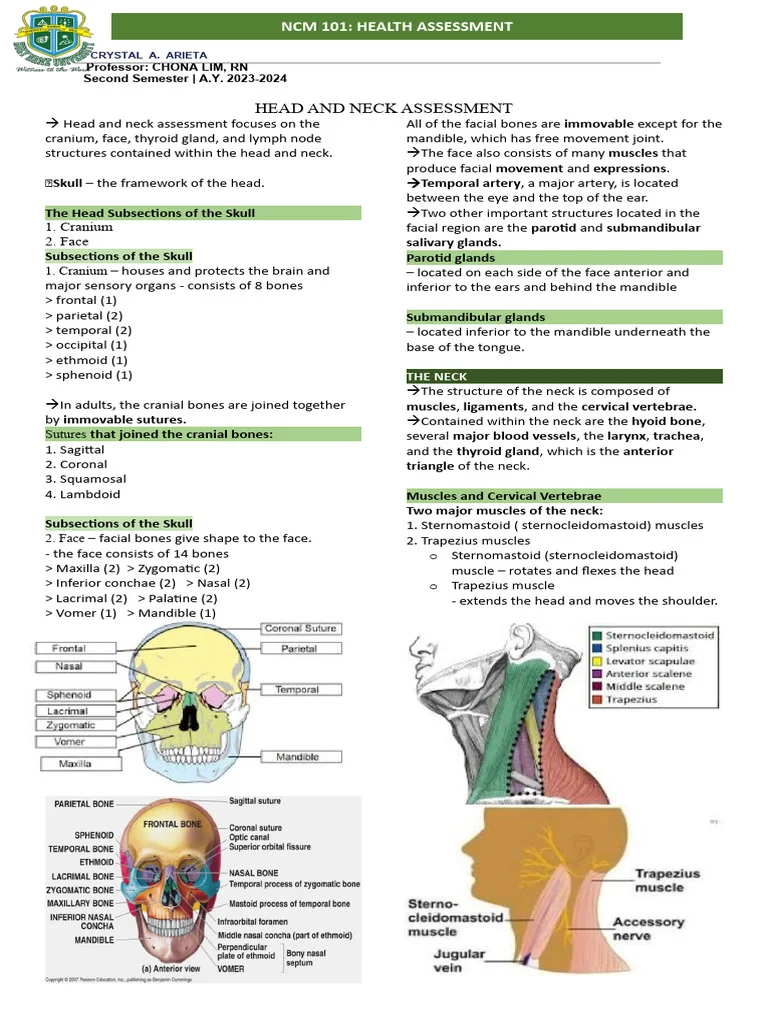
Ear pain, known medically as otalgia, is among the most common reasons people seek medical care in both primary and emergency settings. It affects all age groups but is particularly common in children. Acute otitis media, an infection of the middle ear, is one of the most frequent pediatric illnesses, with many children experiencing at least one episode by the age of three. Although ear pain is often benign, its frequency and potential to signal underlying disease make it a condition that requires careful evaluation.
For clinicians, ear pain presents both a diagnostic challenge and an opportunity for early intervention. Because symptoms can originate from structures within or beyond the ear, accurate assessment is essential to avoid unnecessary antibiotic use and identify less obvious but potentially serious causes.
How Ear Pain Develops
Otaligia can arise from two main mechanisms: primary and secondary causes.
- Primary otalgia: Pain originating within the ear itself-often due to infections or inflammation of the ear canal, eardrum, or middle ear. This type is more common in children due to their developing anatomy and higher incidence of ear infections.
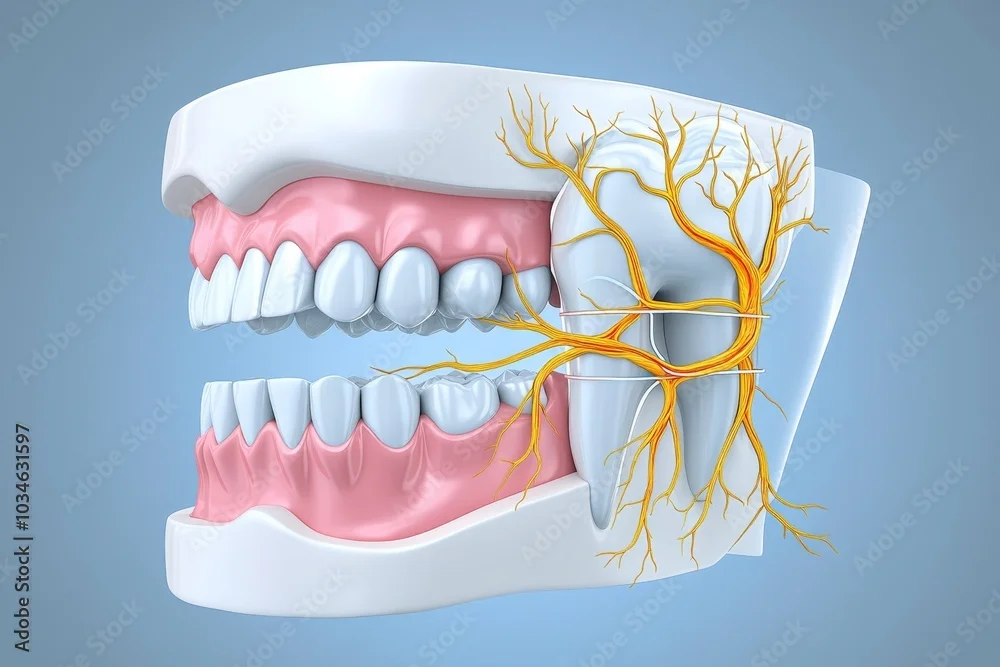
- Secondary (referred) otalgia: Pain transmitted from non-ear sources such as the teeth, jaw, throat, or neck. Adults are more likely to experience this type of referred ear pain.
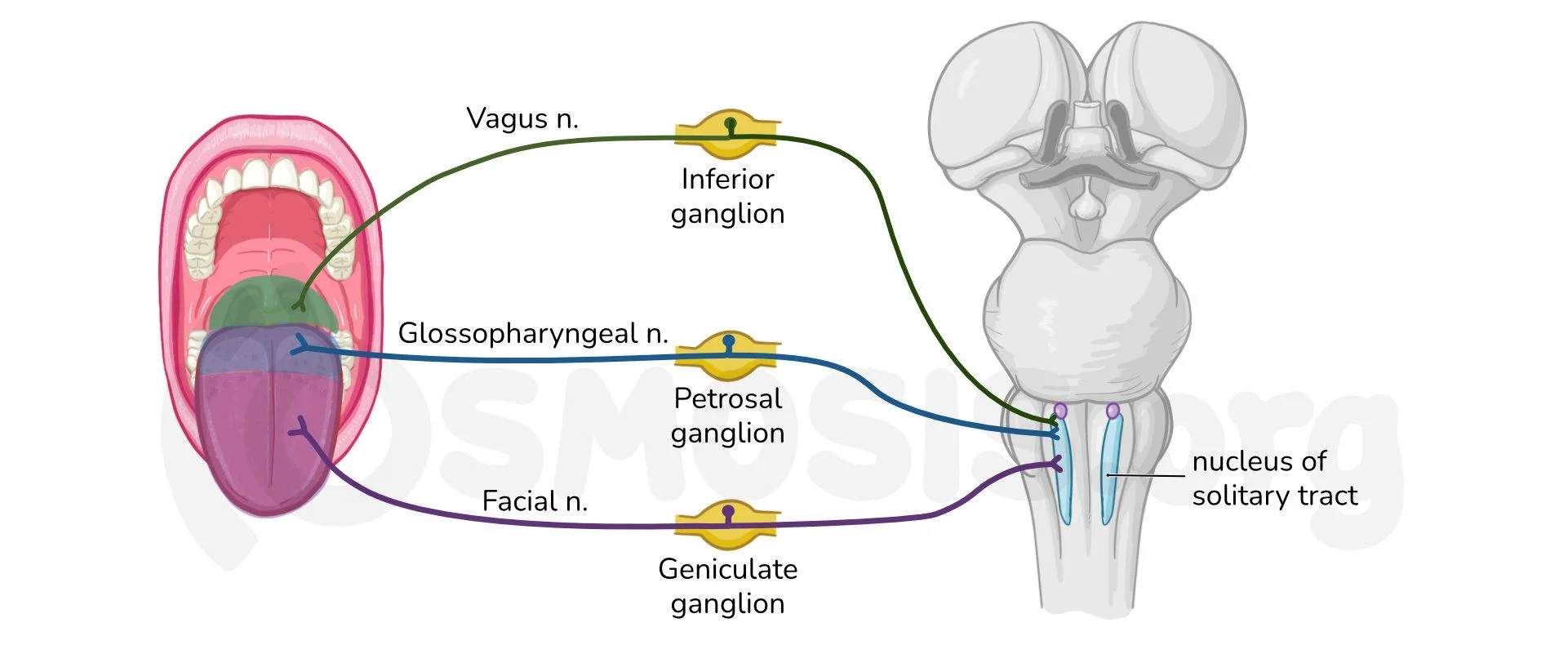
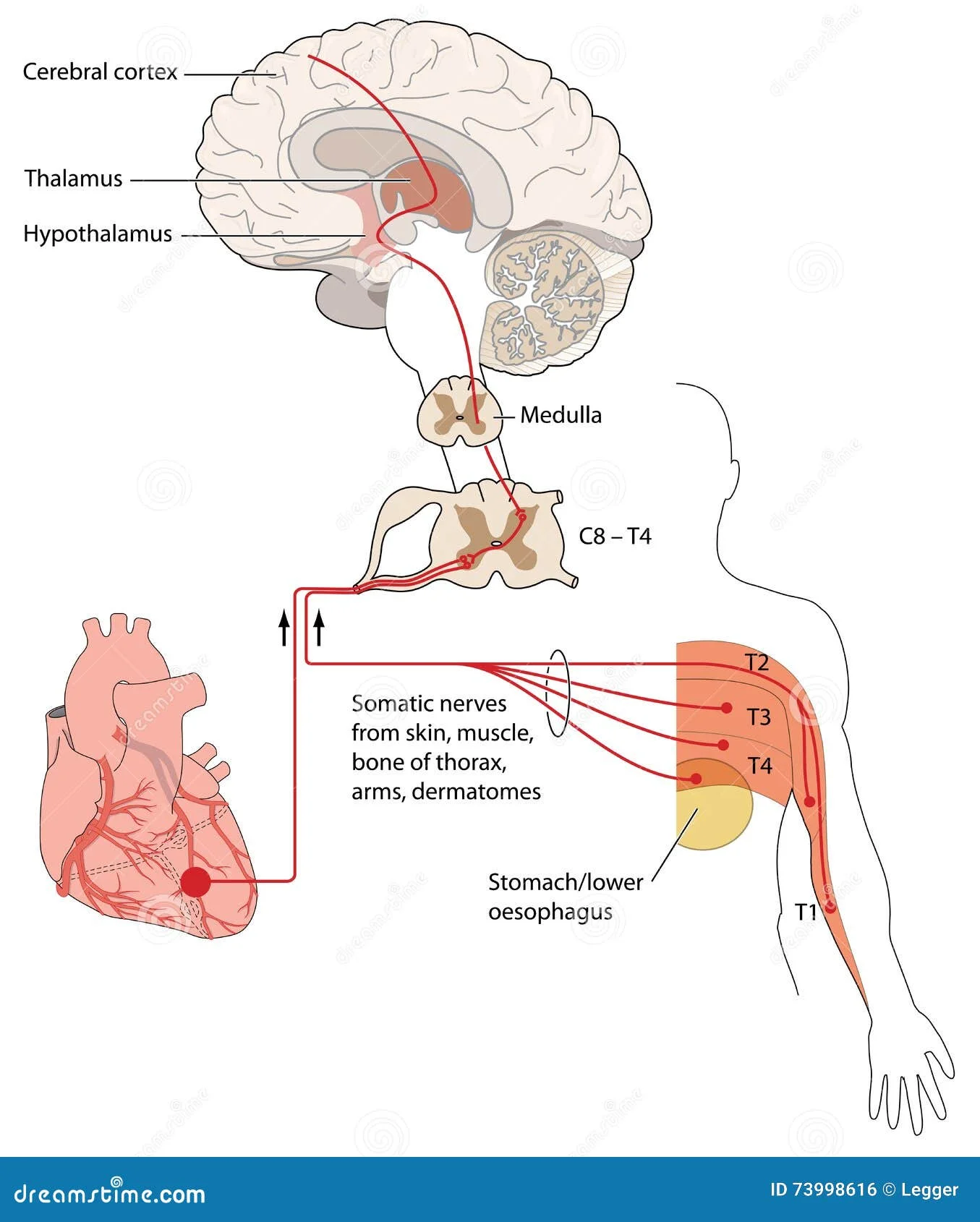
The reason referred pain occurs lies in the ear’s complex nerve supply. Sensory innervation is provided by multiple cranial nerves-trigeminal (V), facial (VII), glossopharyngeal (IX), and vagus (X)-along with upper cervical nerves (C2 and C3). These shared pathways mean that disorders in nearby regions, including the oral cavity or throat, can produce the sensation of ear pain even when the ear appears normal on examination.
Myth vs Fact: ‘Ear Pain Always Means an Ear Infection’
| Myth | Fact |
|---|---|
| Every episode of ear pain is caused by an ear infection that needs antibiotics. | While ear infections are common, especially in children, many cases of ear pain originate from other areas such as dental problems, temporomandibular joint disorders, or throat inflammation. Recognizing this distinction helps clinicians target treatment effectively and avoid unnecessary medication. |
Understanding that ear pain may reflect conditions outside the ear encourages timely diagnosis and better patient outcomes.
Causes of Ear Pain: Primary and Referred Sources
Primary Causes
Ear pain that originates within the ear itself is termed primary otalgia. It usually results from infection or inflammation affecting the external or middle ear. Common primary causes include:
- Acute otitis media
- Acute otitis externa
- Otitis media with effusion
- Auricular inflammation
These conditions often present with visible abnormalities on otoscopic examination, such as redness, swelling, or fluid. In acute otitis media, inflammation and fluid accumulation behind the eardrum cause pressure and pain, often with fever or hearing difficulty. Acute otitis externa, or swimmer’s ear, affects the external canal and produces tenderness when the ear is touched or moved. Otitis media with effusion involves noninfectious fluid buildup in the middle ear, leading to a sensation of fullness or mild discomfort. Recognizing these differences helps clinicians determine whether the pain stems directly from the ear or another source.
Secondary or Referred Causes
Secondary (referred) otalgia occurs when the source of pain lies outside the ear, but shared nerve pathways transmit the sensation to the ear region. Because several cranial and cervical nerves serve both the ear and neighboring structures, discomfort from other areas can be perceived as ear pain even when the ear appears normal. Frequent referred sources include:
- Dental infections
- Temporomandibular joint disorders
- Pharyngeal or tonsillar inflammation
- Sinus disease
- Cervical spine pathology
In some cases, referred ear pain may signal serious conditions. Tumors of the upper aerodigestive tract or skull base can cause ear pain as an early or isolated symptom, even when the ear itself appears normal. Persistent, unexplained pain-especially with a normal otoscopic exam-warrants careful evaluation to exclude deeper or malignant causes. Understanding referred otalgia helps reduce unnecessary antibiotic use and guides clinicians toward the true source of pain.
Myth vs Fact: ‘If the Ear Looks Normal, It Can’t Be Serious’
| Myth | Fact |
|---|---|
| A normal ear exam rules out any significant problem. | Some of the most serious causes of ear pain originate outside the ear and may not alter its appearance. Conditions involving the throat, jaw, or neck-and, in rare cases, tumors-can present as ear pain despite a healthy-looking ear. Persistent or unexplained otalgia should always be evaluated to rule out hidden causes. |
Recognizing Ear Pain Symptoms and Red Flags
Typical Presentations
Ear pain varies in character and intensity-often described as sharp, dull, throbbing, or pressure-like. It may occur with hearing changes or discharge, depending on the underlying condition. In primary ear disease, the pain is usually localized and may be associated with visible abnormalities on examination.
| Condition | Characteristic Features |
|---|---|
| Otitis externa | Pain worsens when the tragus or pinna is touched or moved; canal swelling, redness, or discharge are common. |
| Acute otitis media | Bulging, inflamed tympanic membrane with middle ear effusion; deep, throbbing pain often accompanied by fever or transient hearing loss. |
Recognizing these distinct symptom patterns helps differentiate external from middle ear disease and guides appropriate management.
Recognizing Red Flags
While most ear pain is benign, certain features indicate possible serious disease. Persistent unilateral ear pain with a normal otoscopic examination may reflect referred pain from the throat, jaw, or deeper head and neck structures, including malignancy. Similarly, severe or disproportionate pain in individuals with diabetes or compromised immunity may indicate an aggressive infection requiring urgent evaluation. Other warning signs include pain with unexplained weight loss, difficulty swallowing, or hoarseness.
Red Flags at a Glance
- Persistent or recurrent ear pain with a normal ear examination
- Unilateral pain associated with sore throat, hoarseness, or neck mass
- Severe or escalating pain in diabetic or immunocompromised patients
- Associated neurological symptoms, dysphagia, or unexplained weight loss
- Pain unresponsive to standard treatment or persisting beyond expected recovery
Recognizing these warning features helps clinicians and patients identify when ear pain may represent more than a simple infection, supporting earlier diagnosis and intervention.
Diagnosis: How Clinicians Identify the Cause of Ear Pain
Initial Evaluation
The diagnostic process for ear pain begins with a focused medical history and careful otoscopic examination. A detailed history explores the onset, duration, and character of pain, associated symptoms such as hearing loss, discharge, or systemic illness, and any contributing factors like water exposure or recent upper respiratory infection. The clinician then inspects the outer ear and canal for redness, swelling, discharge, or lesions. Otoscopy allows visualization of the tympanic membrane, helping identify inflammation, effusion, or perforation indicating primary ear disease.
- History: Onset, duration, pain characteristics, and associated symptoms such as hearing loss, discharge, or fever.
- External examination: Observe for redness, swelling, or discharge.
- Otoscopy: Inspect the tympanic membrane for effusion, bulging, or perforation.
If abnormalities are present, the findings typically indicate otitis externa, otitis media, or another local ear condition. A normal ear examination, however, suggests the need to evaluate for referred pain sources.
Beyond the Ear
When otoscopic findings are normal, systematic assessment of surrounding structures is essential. The clinician examines:
- Teeth and jaw: Look for dental decay, abscess, or temporomandibular joint dysfunction.
- Oropharynx and tonsils: Identify infections or masses that may cause referred pain.
- Nose and sinuses: Evaluate for inflammation or congestion.
- Neck and cervical spine: Palpate for muscular tension or arthritic changes radiating discomfort to the ear.
This structured approach ensures both primary and secondary causes are considered early, preventing misdiagnosis and reducing unnecessary antibiotic use when the ear itself is not the pain source.
When to Refer or Order Imaging
Advanced testing is not always necessary but becomes essential when symptoms persist or red flags arise. If warning signs such as persistent unilateral pain, unexplained weight loss, or cranial nerve abnormalities are present, further investigation is warranted. Imaging-typically CT or MRI-can identify deep infections, bone involvement, or occult masses. Endoscopic examination of the nasopharynx and upper aerodigestive tract may also be indicated when referred or malignant causes are suspected.
Referral to an otolaryngologist (ENT specialist) is recommended for cases unresolved with initial management or when diagnostic uncertainty persists. This stepwise, methodical process helps distinguish benign ear conditions from potentially serious diseases, ensuring accurate diagnosis and timely care.
Ear Pain Treatment and Prevention: Relieving Discomfort and Protecting Ear Health
Pain Relief and Supportive Care
Effective management of ear pain begins with controlling discomfort, regardless of the underlying cause. Analgesia using paracetamol or nonsteroidal anti-inflammatory drugs (NSAIDs) is recommended for all patients with otalgia, whether caused by infection, inflammation, or referred pain. These agents help relieve both pain and fever while allowing clearer assessment of the patient’s condition.
- Analgesics: Paracetamol and NSAIDs for pain and fever relief.
- Topical analgesics: Can be used when the tympanic membrane is intact.
- Supportive care: Maintain hydration, avoid manipulating the ear canal, and get adequate rest.
Treating Common Ear Infections
Management strategies differ depending on whether the ear pain arises from the external or middle ear. In acute otitis externa, topical eardrops are the first-line treatment for uncomplicated cases. These often contain antiseptic, antibiotic, or corticosteroid components to reduce inflammation and bacterial load. Systemic antibiotics are reserved for patients with disease extending beyond the ear canal or those who are immunocompromised.
| Condition | Main Treatment | When to Use Antibiotics |
|---|---|---|
| Acute Otitis Externa | Topical eardrops (antiseptic/antibiotic/corticosteroid) | Only if infection extends beyond the ear canal or in high-risk patients |
| Acute Otitis Media | Observation or antibiotics depending on age, severity, and certainty of diagnosis | For confirmed bacterial cases or severe symptoms |
For acute otitis media, diagnosis requires both middle ear effusion and clinical signs of inflammation such as a bulging tympanic membrane. Treatment may involve observation or antibiotics depending on the patient’s age, severity of symptoms, and diagnostic certainty. In mild or uncertain cases, observation with pain control is appropriate, while confirmed bacterial infections or severe presentations warrant targeted antibiotic therapy.
Prevention and When to Seek Help
- Avoid ear canal trauma and keep the ears dry.
- Maintain up-to-date immunizations (influenza, pneumococcal).
- Practice smoking cessation and allergy control to reduce recurrence.
- Seek medical attention for persistent, severe, or recurrent ear pain, or if accompanied by discharge, fever, or hearing loss.
- Urgent evaluation is needed in diabetics or immunocompromised patients, or when malignancy is suspected.
Myth vs Fact: ‘Antibiotics Are Always Needed for Ear Pain’
| Myth | Fact |
|---|---|
| Every case of ear pain requires antibiotic treatment. | Most ear pain improves with accurate diagnosis and supportive care alone. Antibiotics are reserved for confirmed bacterial infections. |

Frequently Asked Questions About Ear Pain
- Is all ear pain caused by an ear infection?
- No. While infections are a frequent cause, ear pain can also come from dental issues, jaw disorders, throat inflammation, or neck problems that refer pain to the ear.
- When should ear pain be considered serious?
- Persistent, one-sided ear pain, especially with normal ear appearance or in people with diabetes or weak immunity, may suggest a deeper infection or serious condition needing prompt evaluation.
- Why does ear pain sometimes worsen when touching the outer ear?
- Pain that increases when moving the pinna or pressing the tragus often indicates inflammation of the external ear canal, known as otitis externa or swimmer’s ear.
- Can ear pain occur without visible ear changes?
- Yes. Referred ear pain from the throat, jaw, or cervical spine can cause discomfort even when the ear appears healthy on examination.
- What are the most common causes of ear pain in adults?
- In adults, dental infections, temporomandibular joint disorders, sinus disease, and referred pain from the throat or neck are common non-ear sources of discomfort.
- How is the cause of ear pain diagnosed?
- Diagnosis begins with a focused history and otoscopic examination, followed by assessment of nearby areas such as the teeth, jaw, throat, and neck if ear findings are normal.
- Do all cases of ear pain require antibiotics?
- No. Many cases improve with pain relief and supportive care alone. Antibiotics are reserved for confirmed bacterial infections or severe cases.
- Can ear pain be prevented?
- Keeping ears dry, avoiding trauma to the ear canal, maintaining vaccinations, and limiting tobacco smoke exposure can help reduce the risk of ear infections and related pain.
- Why is ear pain more common in children?
- Children have shorter, more horizontal eustachian tubes that make fluid buildup and middle ear infections more likely, leading to frequent episodes of otitis media.
- When should someone see a specialist for ear pain?
- Referral to an ear, nose, and throat specialist is advised when pain persists despite treatment, recurs frequently, or is accompanied by symptoms such as hearing loss, weight loss, or neck masses.