Why You Feel Dizzy When You Stand Up: Understanding Orthostatic Hypotension and Related Conditions
Dizziness When You Stand Up
Many people experience a brief sense of lightheadedness or unsteadiness when they rise from sitting or lying down. This common sensation often occurs because blood pressure temporarily drops as the body adjusts to the change in position. While usually short-lived, this kind of dizziness-known medically as orthostatic dizziness-can sometimes signal an underlying issue with how the body regulates blood flow.
What Happens When You Stand
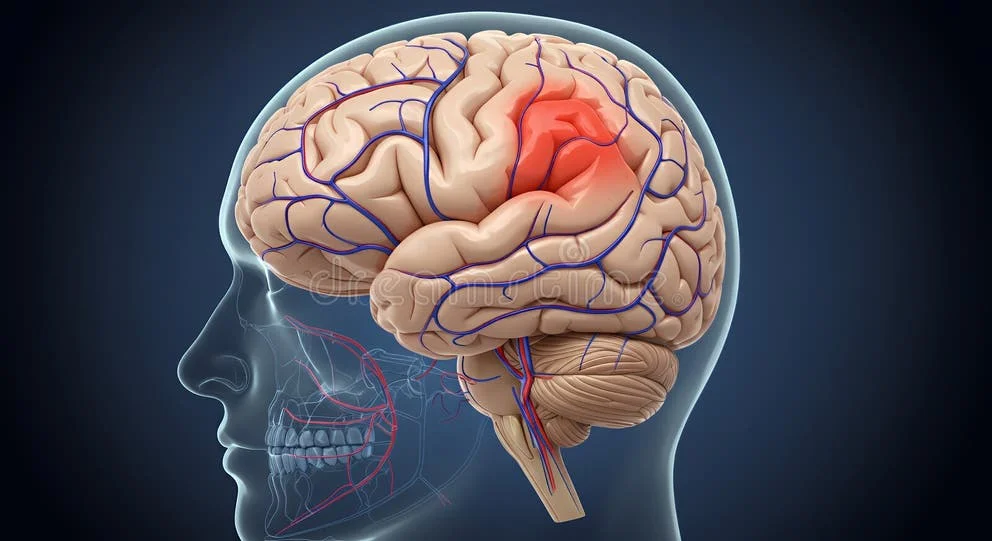
When you move from lying or sitting to standing, gravity pulls blood toward the lower parts of the body, especially the legs and abdomen. In response, your heart and blood vessels work together to keep enough blood flowing to the brain. The heart beats a little faster, and the blood vessels tighten slightly to maintain stable pressure. If this automatic adjustment is delayed or incomplete, blood flow to the brain can momentarily decrease, causing dizziness, dimmed vision, or a feeling that you might faint.
- Gravity causes blood to pool in the legs and abdomen.
- The heart rate increases slightly to maintain blood flow to the brain.
- Blood vessels constrict to stabilize blood pressure.
- If these adjustments are slow, dizziness or blurred vision may occur.
This momentary drop in blood flow is known as orthostatic or postural change. Normally, the body recovers within seconds, but if the response is weak or slow-due to dehydration, certain medications, or other health factors-the dizziness may last longer or happen more frequently.
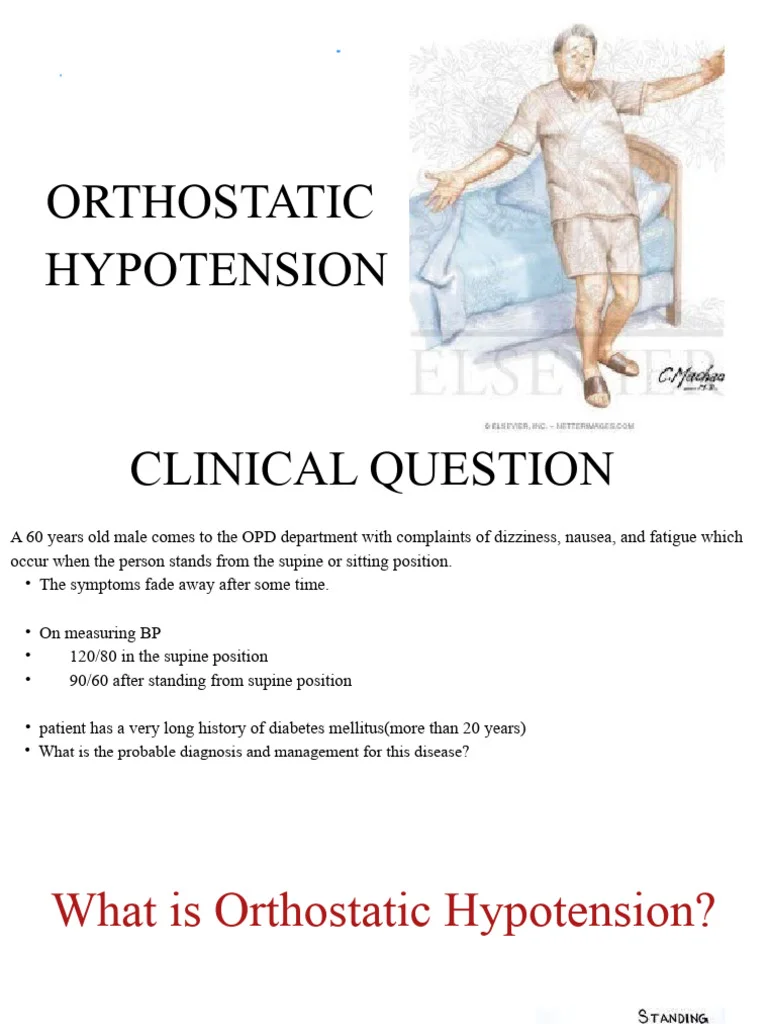
Defining Orthostatic Hypotension
Orthostatic hypotension refers to a measurable drop in blood pressure that occurs soon after standing. Clinically, it is defined as a fall in systolic blood pressure of at least 20 millimeters of mercury (mm Hg) or a drop in diastolic pressure of at least 10 mm Hg within three minutes of standing. This decrease can reduce blood flow to the brain, producing dizziness, blurred vision, or near-fainting.
| Measurement | Threshold Change Upon Standing |
|---|---|
| Systolic Blood Pressure | Decrease of ≥ 20 mm Hg |
| Diastolic Blood Pressure | Decrease of ≥ 10 mm Hg |
| Time Frame | Within 3 minutes of standing |
These changes reflect how the body’s circulatory control system-the autonomic nervous system-responds to posture shifts. When that system does not act quickly enough, symptoms become noticeable. While occasional lightheadedness is common, repeated or prolonged episodes warrant medical attention to understand the underlying cause.
How Common It Is
Dizziness when standing is not rare. Studies suggest that orthostatic hypotension affects roughly one in five adults over the age of sixty. Age-related changes in blood vessel elasticity, slower autonomic responses, and the use of certain medications can all make this group more susceptible. Younger individuals can also experience orthostatic dizziness, especially if they are dehydrated or recovering from illness.
Although the sensation is often mild, frequent or severe episodes can increase the risk of falls and may interfere with daily activities. Understanding why it happens is the first step toward managing it safely and effectively.
Causes and Risk Factors
Dizziness when standing, often linked to orthostatic hypotension, can arise from a range of medical, physiological, and lifestyle factors. The underlying issue usually involves the body’s inability to quickly stabilize blood pressure when moving to an upright position. This can occur due to fluid loss, certain medications, or conditions affecting the heart, nervous system, or hormone balance. Understanding the main causes helps explain why the problem is more common in some people than others.
Common Medical Causes
Several conditions and circumstances can contribute to dizziness when standing. Dehydration is a frequent trigger, as reduced fluid levels lower blood volume and make it harder for the body to maintain steady blood pressure. Cardiovascular problems-such as heart rhythm disturbances or weakened heart function-can also limit the body’s ability to circulate blood efficiently upon standing. Disorders affecting the autonomic nervous system, which controls automatic bodily functions like blood vessel tone and heart rate, may slow the normal compensatory response to gravity. Endocrine disorders, including diabetes or adrenal insufficiency, can further alter how blood pressure is regulated.
- Dehydration reducing overall blood volume
- Cardiovascular issues affecting circulation efficiency
- Autonomic nervous system dysfunction slowing reflexes
- Endocrine disorders like diabetes or adrenal insufficiency
- Medication effects on blood pressure or heart rate
Medications that lower blood pressure or affect the nervous system, such as diuretics, antidepressants, or drugs for Parkinson’s disease, may increase susceptibility to dizziness when standing. Age plays a significant role as well. Orthostatic hypotension occurs frequently in older adults, affecting about one in five people aged sixty and above, as blood vessels become less elastic and reflexes that maintain pressure slow down with age.
Subtypes and Patterns
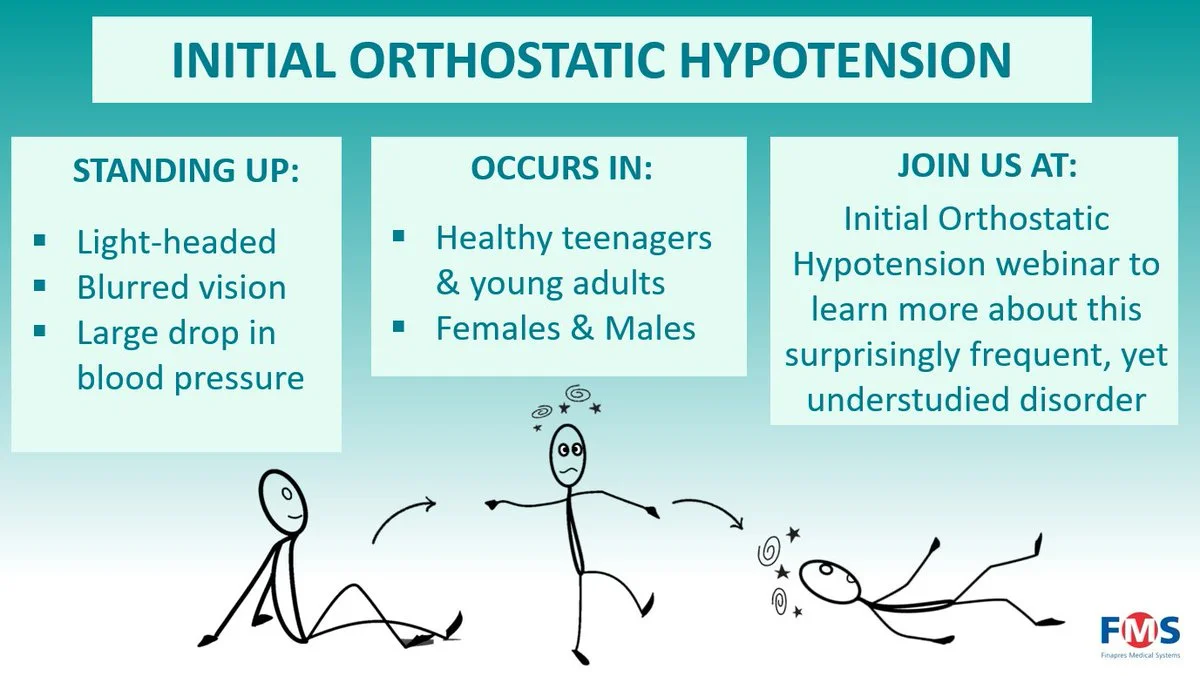
Not all forms of orthostatic hypotension are the same. Clinicians recognize several subtypes based on how quickly symptoms develop after standing. In initial orthostatic hypotension, blood pressure drops immediately upon standing but recovers within about half a minute, often producing brief dizziness or dim vision. Classic orthostatic hypotension describes a sustained drop in blood pressure occurring within three minutes of standing and is the most widely recognized form. Delayed orthostatic hypotension appears more gradually, typically after several minutes of standing, and may go unnoticed without specific testing.
| Subtype | Timing After Standing | Typical Duration |
|---|---|---|
| Initial | Immediately upon standing | Recovers within ~30 seconds |
| Classic | Within 3 minutes | Persistent unless corrected |
| Delayed | After several minutes | Gradual and may go unnoticed |
These patterns can help clinicians identify the underlying mechanism and guide further evaluation, particularly in people who experience frequent or unpredictable episodes of dizziness.
Recognizing the Symptoms
The hallmark symptom of orthostatic hypotension is a feeling of lightheadedness or unsteadiness soon after standing. Some people describe blurred or tunnel vision, weakness, or a sensation that they might faint. These symptoms usually resolve after sitting or lying down again. In milder cases, dizziness may last only a few seconds, but in more pronounced cases it can persist longer and increase the risk of falls, especially among older adults.
- Lightheadedness or unsteadiness
- Blurred or tunnel vision
- Weakness or near-fainting sensations
- Brief relief after sitting or lying down
Recognizing these sensations and the situations that trigger them-such as standing quickly, heat exposure, or prolonged inactivity-can help individuals and clinicians identify orthostatic patterns early and address contributing factors effectively.
Diagnosing Dizziness When Standing
When dizziness occurs mainly after standing up, doctors focus on understanding how the body’s blood pressure and heart rate respond to posture changes. Diagnosis involves a combination of direct measurements, medical history, and the exclusion of other possible causes. The goal is to identify whether the dizziness stems from a hemodynamic issue-such as orthostatic hypotension or postural orthostatic tachycardia syndrome-or from another unrelated condition.
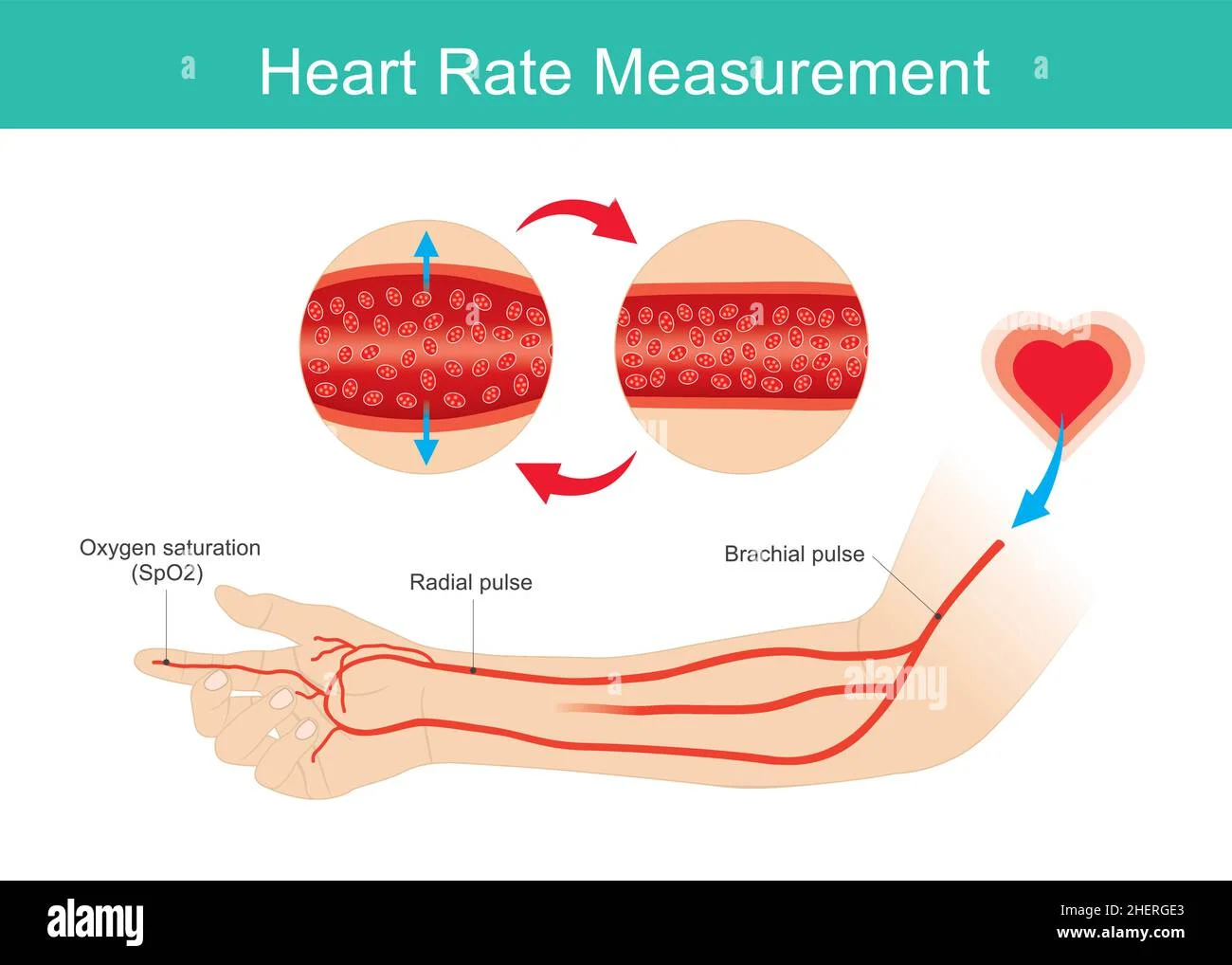
Measuring Orthostatic Vital Signs
The first step in evaluation is usually measuring orthostatic vital signs. This means checking blood pressure and heart rate while lying down, then again after standing or using a tilt table to simulate standing. A consistent drop in blood pressure or an unusual rise in heart rate can help confirm a hemodynamic cause. In orthostatic hypotension, for example, blood pressure falls significantly within a few minutes of standing, while in postural orthostatic tachycardia syndrome, the pulse rate increases markedly without a major pressure drop.
- Blood pressure and heart rate are measured while lying down and again after standing.
- A tilt-table test may be used to reproduce the standing position safely.
- A drop in blood pressure suggests orthostatic hypotension.
- A sharp rise in heart rate without a blood pressure drop suggests postural orthostatic tachycardia syndrome.
These readings are interpreted alongside the patient’s symptoms-particularly if dizziness, unsteadiness, or visual dimming improves after sitting or lying down. This pattern helps distinguish hemodynamic orthostatic dizziness, where reduced blood flow or abnormal heart rate adjustment is the root cause, from other types of dizziness.
Excluding Other Causes
Because dizziness can arise from many different systems in the body, doctors also consider and rule out non-hemodynamic causes. Vestibular disorders, such as inner ear imbalances, may lead to spinning sensations that are unrelated to standing posture. Neuropathy, affecting nerve communication in the legs or blood vessels, and certain gait or balance disorders can also mimic orthostatic dizziness. Evaluating these factors helps ensure the diagnosis is accurate and that the right treatment approach is chosen.
- Vestibular (inner ear) disorders causing spinning or vertigo sensations
- Peripheral neuropathy affecting nerve control of blood vessels
- Gait or balance disorders that can resemble dizziness on standing
In some cases, additional neurological or cardiovascular testing may be used to clarify complex presentations, especially when symptoms occur unpredictably or coexist with other medical conditions. A thorough evaluation helps identify the exact mechanism behind dizziness and prevents overlooking other treatable conditions.
When to See a Doctor
Recurrent dizziness, fainting, or confusion after standing should prompt medical evaluation, especially in older adults. Early assessment helps determine whether a blood pressure or heart rate problem is contributing and reduces the risk of falls or other complications.
Managing and Treating Orthostatic Dizziness
Most people who experience dizziness when standing improve once the underlying cause is identified and addressed. Treatment focuses on stabilizing blood pressure and preventing sudden drops when moving upright. Doctors usually begin with simple lifestyle measures before considering medication, tailoring each approach to the individual’s health needs and the specific type of orthostatic hypotension involved.
Lifestyle and Non-Drug Strategies
Non-drug measures are the foundation of managing orthostatic dizziness. Maintaining adequate fluid intake helps keep blood volume stable, while increasing dietary salt-if recommended by a clinician-can support blood pressure. Standing up gradually, especially after lying down for a long time, allows the body to adjust more smoothly to position changes. Physical counter-maneuvers, such as crossing the legs or tensing the calf muscles before standing, can help push blood back toward the heart and brain.
- Stay well hydrated throughout the day to maintain blood volume.
- Increase dietary salt only under medical supervision.
- Rise slowly from sitting or lying positions.
- Use physical counter-maneuvers (leg crossing, calf tensing) before standing.
- Wear compression garments, such as waist-high stockings or abdominal binders.
- Review medications that might lower blood pressure with a healthcare provider.
Compression garments, including waist-high stockings or abdominal binders, reduce blood pooling in the lower body and help maintain circulation to the brain. Reviewing medications is also an important step, as some drugs used to treat blood pressure, depression, or Parkinson’s disease may contribute to orthostatic symptoms. Adjusting or replacing these under medical supervision can significantly lessen dizziness episodes. These strategies are often effective and can be customized to a person’s lifestyle and physical condition.
Medication Options
If symptoms persist despite lifestyle adjustments, medication may be introduced. Drug therapy aims to increase blood pressure or improve the body’s ability to regulate it. The choice of medication depends on whether the orthostatic hypotension is neurogenic-arising from nervous system dysfunction-or non-neurogenic, related to other causes such as dehydration or medication effects. In neurogenic forms, specific agents that enhance blood vessel constriction or expand blood volume may be used to reduce dizziness and prevent fainting.
| Stage | Focus | Examples |
|---|---|---|
| First-line | Lifestyle and volume management | Hydration, salt intake, compression garments, slow posture changes |
| Second-line | Medication review and adjustment | Identify drugs contributing to low blood pressure |
| Third-line | Targeted pharmacologic therapy | Medications tailored to neurogenic or non-neurogenic causes |
Medication is typically added only after non-drug strategies have been optimized, and doses are tailored to minimize side effects while maintaining stability throughout the day. Ongoing monitoring allows adjustments as symptoms change or as other health conditions evolve. With proper management, many individuals experience a marked reduction in dizziness and regain confidence in standing and moving about safely.
Dizziness When Standing
Many people experience a brief sense of lightheadedness or unsteadiness when they rise from sitting or lying down. This common sensation often occurs because blood pressure temporarily drops as the body adjusts to the change in position. While usually short-lived, this kind of dizziness-known medically as orthostatic dizziness-can sometimes signal an underlying issue with how the body regulates blood flow.
What Happens When You Stand
When you move from lying or sitting to standing, gravity pulls blood toward the lower parts of the body, especially the legs_












