Relieving Phlegm in Throat: Proven Ways to Clear Mucus Buildup
Causes of That Persistent Phlegm in the Throat Sensation
How Mucus Normally Works
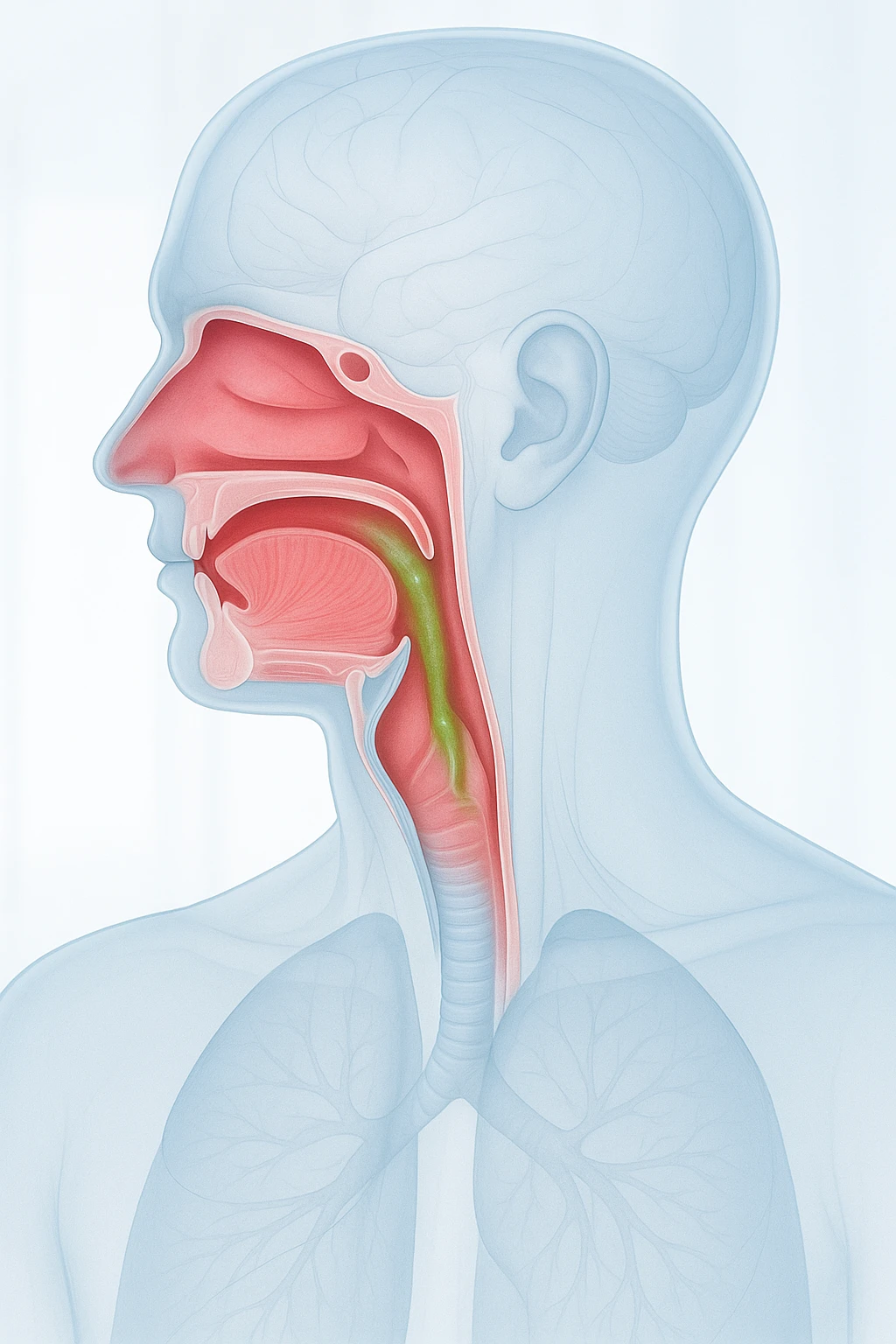
Mucus is a natural and essential fluid produced by the lining of the nose, sinuses, and throat. It acts as the body’s built-in filter, trapping dust, allergens, and germs before they can reach the lungs. Normally, this thin layer of mucus moves silently through the throat and is swallowed without notice. Under healthy conditions, this process keeps the airways moist and protected.
The feeling of phlegm in the throat-or “something stuck” in the throat-arises when this balance changes. When mucus becomes thicker or the body produces it in greater amounts, people may become aware of its movement. The body’s response, such as frequent throat clearing or mild coughing, is a way of trying to remove the excess.
Postnasal Drip and Why It Happens
Postnasal drip describes mucus from the nasal cavity and sinuses draining down the back of the throat. This flow is normal, but it becomes bothersome when the mucus is too thick, sticky, or plentiful. The sensation of constant drainage, a lump in the throat, or a need to clear the throat often points to this process.
Postnasal drip is part of a broader condition known as Upper Airway Cough Syndrome. In this situation, mucus accumulation and throat irritation can trigger coughing or hoarseness. While uncomfortable, these symptoms are usually not dangerous-they simply reflect how sensitive the upper airway can be to even small changes in mucus consistency.
Common Triggers
Many everyday factors can increase mucus production or make it thicker:
- Allergies and sinus issues: Allergic and non-allergic rhinitis-often triggered by pollen, dust, or strong odors-are leading causes.
- Infections: Sinus infections and common colds can inflame the nasal lining, prompting excess mucus that flows into the throat.
- Viral colds: During infection, the mucus naturally becomes denser and more noticeable.
- Reflux: Stomach acid moving toward the throat (laryngopharyngeal reflux) may mimic or worsen postnasal drip sensations.
- Environmental irritants: Cigarette smoke, air pollution, or dry indoor air can thicken secretions and intensify throat discomfort.
Recognizing and minimizing these triggers can help reduce the sensation of persistent mucus and improve overall throat comfort.
Recognizing Symptoms and Knowing When to Seek Help
Typical Sensations and Associated Symptoms
People with excess throat mucus often describe a sensation of fullness, dripping, or something “stuck” in the throat. This feeling is usually more noticeable when lying down or after waking in the morning. Because the mucus irritates the throat lining, many individuals find themselves clearing their throat frequently throughout the day.
Coughing is another common feature, especially when the mucus becomes thick or irritates the upper airway. The cough may be dry or produce a small amount of mucus but rarely indicates anything serious by itself. These symptoms typically reflect postnasal drainage or mild throat irritation rather than infection or disease.
- Frequent throat clearing
- Sensation of mucus dripping or being stuck in the throat
- Mild, often dry cough
- Worsening at night or upon waking
When to See a Doctor
In most cases, phlegm in the throat is temporary and harmless, improving as the underlying cause-such as a cold or mild allergy-resolves. However, persistent or worsening symptoms may point to another issue. Doctors usually make the diagnosis based on medical history and a physical examination, since there is no single test that confirms postnasal drip or related upper airway conditions. Evaluation focuses on identifying potential causes such as sinus disease, reflux, or chronic nasal inflammation.
Parents and adults should be aware of warning signs that require medical attention. These include symptoms lasting several weeks despite self-care, mucus that is bloody or discolored, or breathing difficulties that interfere with sleep or daily activities. In such cases, a clinician can rule out other causes and guide appropriate treatment.
Red flags:
- Phlegm lasting longer than three weeks
- Blood-streaked or discolored mucus
- Fever or shortness of breath
- Unexplained weight loss
How Clinicians Identify the Cause of Phlegm in the Throat
Clinical Assessment
When someone reports a constant sensation of mucus or phlegm in the throat, clinicians begin with a detailed history. They ask about when symptoms began, how long they have lasted, and what factors make them better or worse. Information about allergies, sinus infections, acid reflux, or environmental exposures helps narrow down possible causes. Because postnasal drip is a symptom rather than a measurable disease, the goal is to understand the pattern and triggers of mucus buildup.
The physical examination includes checking the nasal passages, throat, and sometimes the ears for inflammation or drainage. Doctors may gently inspect the back of the throat or use a small lighted scope to view the nasal cavity. These findings, combined with the patient’s description of symptoms, often provide enough information to guide an initial diagnosis. In many cases, improvement after targeted therapy-such as nasal sprays or reflux management-helps confirm the suspected cause.
- Symptom history: onset, duration, and triggers
- Examination of nasal passages, throat, and ears
- Use of a lighted scope for closer nasal or throat inspection
- Monitoring improvement after targeted treatment
Additional Testing
There is no single objective test for postnasal drip or Upper Airway Cough Syndrome. Testing is reserved for persistent or unclear cases. If allergy is suspected, skin or blood tests may identify specific triggers. Imaging of the sinuses may be ordered if structural problems or chronic sinus disease are possible. In patients with reflux-like symptoms, evaluation of stomach acid flow or referral to a specialist may be considered.
Ultimately, diagnosis focuses on excluding other common causes of throat discomfort and cough. By combining careful history with selective testing, clinicians determine whether nasal, sinus, or reflux conditions are responsible for the persistent phlegm sensation.
| Possible Test | Purpose |
|---|---|
| Allergy skin or blood tests | Identify allergic triggers |
| Sinus imaging | Detect structural problems or chronic sinus disease |
| Reflux evaluation | Assess stomach acid involvement in throat symptoms |
Evidence-Based Treatments That Relieve Phlegm in the Throat
Targeted Medical Treatments
Treatment depends on the underlying cause rather than a single remedy. When nasal or sinus inflammation is responsible, saline nasal irrigation can help flush out thick mucus and reduce irritation. Many clinicians also recommend intranasal corticosteroid or antihistamine sprays for people with allergic or chronic nasal inflammation. These medicines reduce swelling in the nasal passages, allowing mucus to flow normally and preventing it from collecting in the throat.
- Saline nasal irrigation to clear thick mucus
- Intranasal corticosteroid or antihistamine sprays to reduce inflammation
- Antihistamine-decongestant combinations for rhinitis-related symptoms
- Reflux management through lifestyle or prescribed acid-reducing medications
Because postnasal drip and related symptoms can have multiple causes, the most effective treatment often combines several of these approaches based on individual needs.
Home and Lifestyle Measures
Simple home strategies can ease the feeling of phlegm in the throat. Staying well hydrated helps thin mucus so it can move more freely and be swallowed comfortably. Using a humidifier in dry environments adds moisture to the air, preventing mucus from becoming sticky or difficult to clear. Avoiding irritants such as cigarette smoke and strong chemical fumes can also reduce throat inflammation and mucus buildup.
- Drink plenty of water to keep mucus thin
- Use a humidifier to moisten dry indoor air
- Avoid cigarette smoke and chemical irritants
- Rinse nasal passages gently with saline if prone to allergies or colds
These non-medicated measures complement medical treatments to support ongoing relief and prevent symptom recurrence.
What Doesn’t Work
Despite common beliefs, certain habits and remedies do not reduce mucus production. One persistent myth is that drinking milk causes more phlegm. In reality, milk does not increase the body’s mucus output-it may simply leave a temporary coating in the mouth that makes mucus feel thicker during a cold. Similarly, antibiotics are rarely useful for throat phlegm unless a bacterial infection is confirmed. Overusing antibiotics can lead to side effects and resistance without addressing the real cause of excess mucus.
| Myth | Fact |
|---|---|
| Drinking milk increases mucus | Milk does not increase mucus; it may only feel thicker during infections. |
| Antibiotics help clear mucus | Antibiotics are not effective unless a bacterial infection is confirmed. |
Myth vs Fact: Myth: Drinking milk increases mucus. Fact: Research shows it does not; mucus only feels thicker during infections.
Phlegm in Children and Family Prevention Tips
Phlegm in Children
Children often experience phlegm in the throat more frequently than adults because their airways are smaller and their immune systems are still developing. Common triggers include viral colds, allergies, and sinus infections, all of which can increase mucus production in the upper airways. During a cold, mucus naturally becomes thicker, leading to more noticeable throat clearing or mild coughing. Younger children may also have difficulty describing the sensation, so parents may notice frequent swallowing, sniffling, or nighttime coughing.
- Common triggers: viral colds, allergies, and sinus infections
- Typical signs: frequent swallowing, sniffling, or nighttime coughing
- Thicker mucus: during colds may cause throat clearing or mild cough
Allergic and nonallergic rhinitis are frequent causes of persistent mucus in children, especially during certain seasons or after exposure to dust, pet dander, or pollen. Most cases improve with simple measures like nasal saline rinses and avoiding irritants. However, if symptoms persist for weeks, interfere with sleep, or are accompanied by fever or breathing difficulty, a pediatric evaluation is important to rule out infection or asthma.
Preventing Recurrence
Prevention begins with identifying and managing each child’s main triggers. Keeping nasal passages clear with gentle saline sprays and ensuring proper hydration helps mucus stay thin and easier to clear. A humidifier in the bedroom can be particularly helpful during dry winter months. Managing known allergies-by minimizing exposure or following prescribed treatments-reduces the likelihood of recurring congestion and throat phlegm.
- Use saline sprays to keep nasal passages clear
- Encourage frequent hydration
- Use humidifiers during dry seasons
- Limit exposure to smoke, pollutants, and strong chemicals
- Promote regular handwashing and cold prevention habits
Parents should also limit exposure to common irritants. Tobacco smoke, household pollutants, and strong cleaning chemicals can inflame the nasal lining and worsen mucus buildup. Encouraging children to wash their hands regularly and avoid close contact with people who have colds helps lower the risk of viral infections that thicken mucus.
Healthy Home Habits
Creating a supportive home environment makes a noticeable difference in airway health for the whole family. Maintaining a smoke-free home is one of the most effective ways to prevent chronic throat irritation and mucus formation. Balanced meals rich in fruits and vegetables support immune defenses that help the body recover faster from colds. Regular handwashing and adequate rest further protect against infections that lead to thickened mucus.
- Keep the home smoke-free
- Serve balanced meals rich in fruits and vegetables
- Encourage consistent sleep routines and adequate rest
- Reinforce frequent handwashing
These small, consistent actions-hydration, clean air, and early management of nasal or allergic symptoms-can greatly reduce how often children experience throat phlegm and promote long-term respiratory comfort for the entire family.
Frequently Asked Questions About Phlegm in the Throat
- Why do I constantly feel mucus or phlegm in my throat?
- This sensation often happens when mucus from the nose and sinuses drains into the throat, a process known as postnasal drip. Allergies, sinus inflammation, or reflux are common underlying causes.
- Is phlegm in the throat always a sign of infection?
- Not necessarily. Many cases are due to allergies, mild irritation, or environmental factors like smoke or dry air, rather than an infection.
- Can acid reflux make throat mucus worse?
- Yes. Stomach acid that reaches the throat can irritate its lining, causing inflammation and an increased feeling of mucus buildup.
- Why is the problem worse at night or in the morning?
- When lying down, mucus can collect in the back of the throat. Overnight, it thickens slightly, making symptoms more noticeable in the morning.
- When should I see a doctor about persistent phlegm?
- If symptoms last more than three weeks, include blood-streaked mucus, fever, or shortness of breath, medical evaluation is important to rule out other conditions.
- Can allergies cause phlegm in the throat?
- Yes. Allergic rhinitis can lead to nasal congestion and drainage that moves down the throat, often causing throat clearing or a mild cough.
- Does drinking milk really make mucus worse?
- No. Milk does not increase mucus production. It may only leave a coating that makes the mucus feel thicker during a cold.
- How do doctors diagnose the cause of throat phlegm?
- Doctors review your symptoms, check your nose and throat, and may recommend allergy testing or sinus imaging if needed. Diagnosis usually relies on clinical evaluation rather than one specific test.
- What home remedies can help ease throat mucus?
- Staying hydrated, using a humidifier, and rinsing nasal passages with saline can help thin mucus and relieve discomfort. Avoiding smoke and irritants also reduces symptoms.
- How can families prevent frequent throat phlegm in children?
- Keeping the home smoke-free, managing allergies, and maintaining good hand hygiene can reduce mucus buildup. Encouraging hydration and proper rest supports airway health.