Trouble Breathing When Lying Flat: Diagnosis and Treatment Options
Orthopnea: A Key Cause of Trouble Breathing When Lying Flat
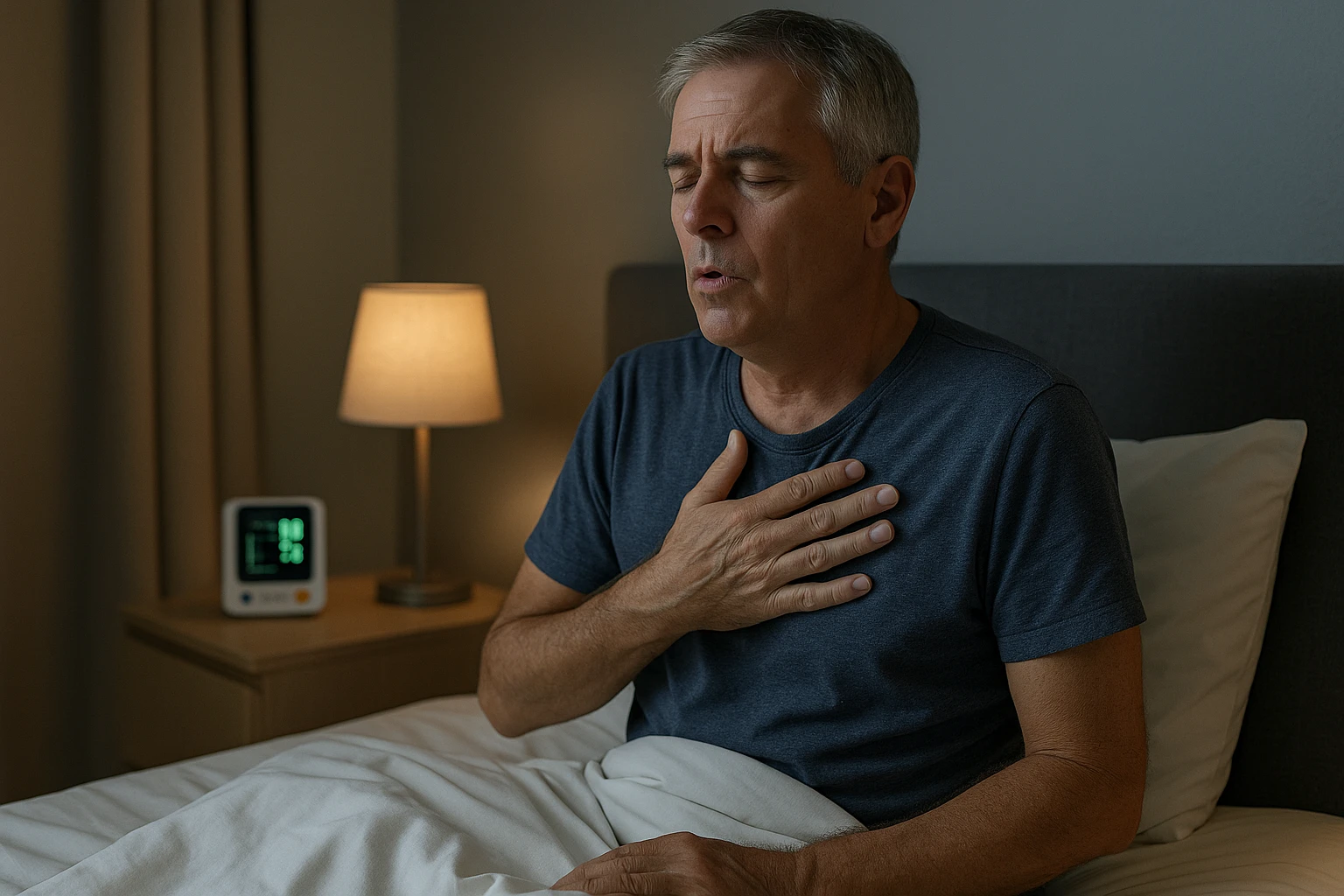
Orthopnea is a condition where a person experiences shortness of breath when lying down, which is typically relieved by sitting up or standing. This type of breathing difficulty can occur at night and may interfere with sleep, often causing people to wake up gasping for air. The relief that comes from sitting or standing is a hallmark of orthopnea, distinguishing it from other types of shortness of breath.
Orthopnea is often a symptom of an underlying health condition. Some of the most common causes include:
- Heart failure
- Chronic obstructive pulmonary disease (COPD)
- Obesity
- Sleep apnea
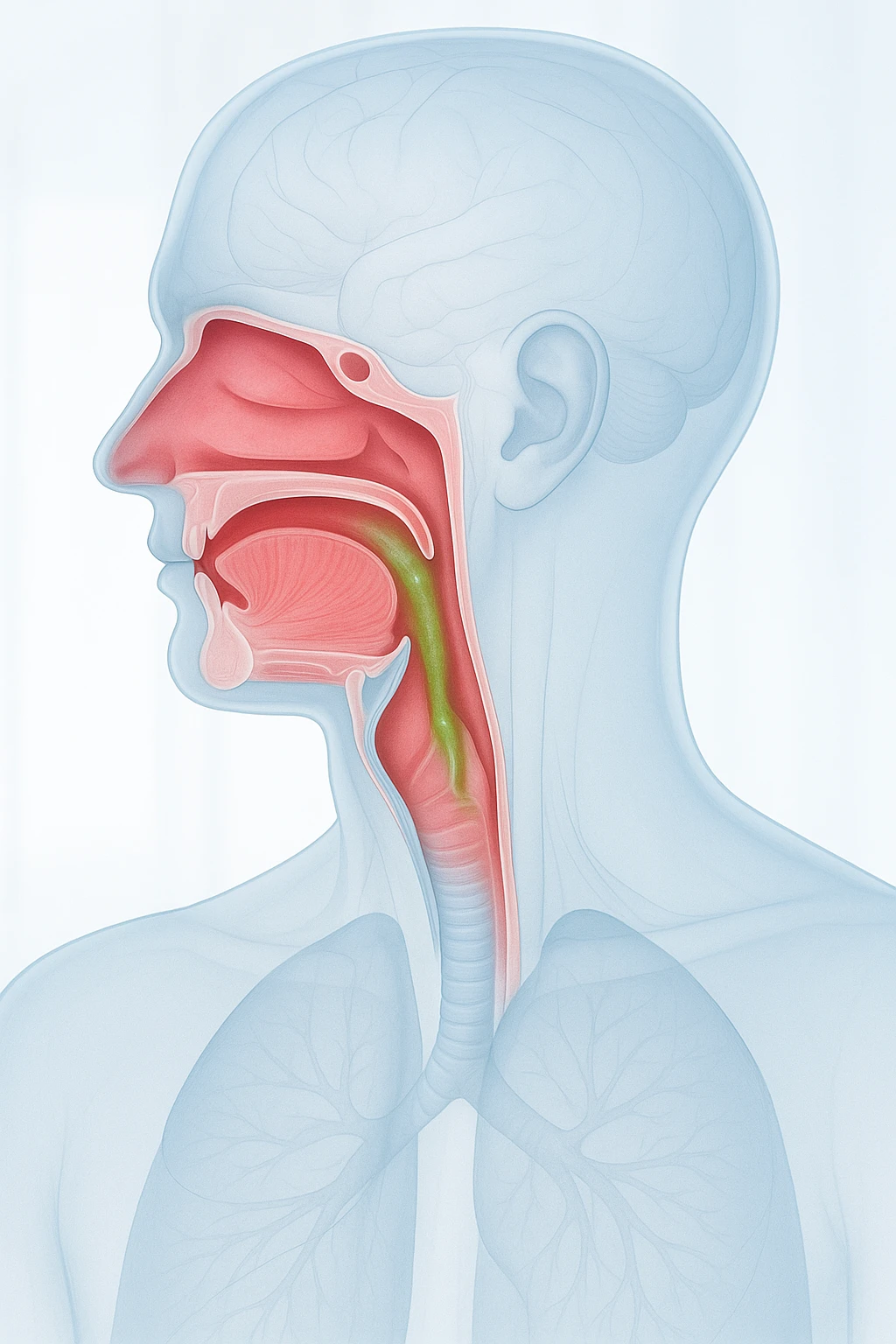
In heart failure, for example, the heart’s inability to pump blood efficiently leads to fluid buildup in the lungs, which worsens when lying flat. In COPD, the narrowing of airways makes it harder to breathe, and gravity can worsen this effect when lying down.
While orthopnea can occur for a variety of reasons, the key to managing the condition lies in addressing the root cause. Treatment usually involves managing the underlying condition, whether through medications, lifestyle changes, or other therapies. Understanding the cause of orthopnea is important for effective treatment and improving quality of life.
Common Causes of Trouble Breathing When Lying Flat
Heart-Related Causes
Heart failure is one of the most common causes of orthopnea. In heart failure, the heart’s ability to pump blood efficiently is compromised. This leads to fluid buildup in the lungs, a condition known as pulmonary congestion. When lying flat, gravity causes this fluid to distribute more evenly throughout the lungs, making breathing more difficult. As a result, individuals may experience increased shortness of breath when lying down, which is relieved by sitting up or standing, allowing gravity to help move the fluid away from the lungs.
Lung-Related Causes
Lung diseases like chronic obstructive pulmonary disease (COPD) and pneumonia can also contribute to orthopnea. COPD causes narrowing of the airways, which reduces airflow and makes it harder to breathe, especially when lying flat. In pneumonia, infection causes inflammation and fluid accumulation in the lungs, further hindering the ability to breathe normally. In both conditions, lying down exacerbates the difficulty in getting enough air, as the lungs’ ability to expand and contract is impaired.
Other Contributing Factors
Several other factors can also worsen orthopnea symptoms:
- Obesity: Increases pressure on the diaphragm and lungs, making it harder to breathe while lying down.
- Sleep apnea: A condition where breathing temporarily stops during sleep, can also cause breathing difficulties when lying flat.
- Anxiety: May contribute by triggering a sensation of breathlessness, especially when lying down.
- Diaphragm paralysis: Reduces the ability to breathe deeply and effectively.
- Pleural effusion: Fluid around the lungs, which can interfere with lung expansion.
- Ascites: Fluid buildup in the abdomen that can exert pressure on the diaphragm and lungs.
Paroxysmal Nocturnal Dyspnea (PND) and Its Impact on Sleep
Paroxysmal Nocturnal Dyspnea (PND) is a specific form of orthopnea, a condition where a person experiences shortness of breath when lying down. Unlike general orthopnea, which may occur at any time, PND typically occurs suddenly during sleep. It often causes a person to wake up abruptly, feeling as if they cannot catch their breath. This is a distressing experience, as the sensation of not being able to breathe can lead to feelings of panic and anxiety.
The key difference between PND and general orthopnea is that PND happens while the person is asleep, often waking them from rest, whereas general orthopnea can occur when awake or while trying to sleep. The breathlessness from PND is usually relieved when the person sits up or stands, as gravity helps move fluid away from the lungs, improving their ability to breathe.
Causes of Paroxysmal Nocturnal Dyspnea
PND is often associated with heart conditions, particularly heart failure, where fluid can accumulate in the lungs during sleep, leading to sudden shortness of breath. Individuals experiencing PND may find it helpful to sleep with their head elevated or in a more upright position to reduce the frequency of these episodes. While PND can be frightening, it can be managed by addressing the underlying cause, such as heart failure or other respiratory issues.
How Orthopnea Impacts Daily Life and Well-Being
Orthopnea, or shortness of breath when lying down, can significantly affect a person’s daily life. The condition often leads to sleep disturbances, making it difficult to fall or stay asleep. Individuals with orthopnea may wake up during the night feeling breathless, leading to fragmented sleep and a lack of restful recovery. This can contribute to daytime fatigue, irritability, and difficulty focusing on everyday tasks.
Impact on Physical Activity
Physical activity can also become challenging for people with orthopnea. The difficulty breathing when lying down may extend to physical exertion, particularly when bending over or engaging in activities that involve lying flat. This limitation can reduce one’s ability to participate in regular exercise or daily tasks, affecting overall fitness and quality of life.
Mental Health Effects
In addition to physical effects, orthopnea can have a profound impact on mental health. The discomfort and fear of not being able to breathe properly can lead to anxiety, stress, and feelings of helplessness. Over time, the stress of managing orthopnea can contribute to depression or worsen existing mental health conditions. Addressing the underlying causes of orthopnea is essential to improving not only physical health but also emotional well-being.
Managing Orthopnea: Treatment and Practical Steps
Medications and Therapies
The treatment of orthopnea primarily focuses on managing the underlying conditions that cause shortness of breath. Common treatments include medications such as diuretics for heart failure and oxygen therapy for respiratory conditions like COPD. CPAP therapy may be used for sleep apnea, helping to keep airways open during sleep and prevent breathing interruptions.
Lifestyle Modifications
In addition to medications, certain lifestyle changes can help reduce symptoms. These include managing weight, maintaining a healthy diet, and incorporating regular exercise, all of which help improve lung and heart function. It is essential to consult a healthcare provider before starting any exercise program, especially for individuals with heart or lung conditions.
Positioning and Sleep Adjustments
Adjusting sleep positions is a practical strategy for managing orthopnea. Raising the head of the bed or using extra pillows can reduce fluid buildup in the lungs, making it easier to breathe while lying down. For children with orthopnea, sleeping in a more upright position can also help alleviate symptoms.
What to Expect During the Diagnosis of Orthopnea and Trouble Breathing When Lying Flat
Initial Diagnosis
The process of diagnosing orthopnea, a condition involving trouble breathing when lying flat, typically begins with a detailed medical history and a physical examination. Your doctor will ask about your symptoms, including when shortness of breath occurs and how severe it is. They will also inquire about any underlying health conditions, such as heart disease, lung disorders, or obesity, as these are common contributors to orthopnea. During the physical exam, your doctor may listen to your lungs and heart to check for signs of fluid buildup, abnormal lung sounds, or other indicators of a medical condition that could be causing the breathlessness.
Advanced Diagnostic Tools
If your doctor suspects that orthopnea is related to an underlying condition, they may recommend further diagnostic tests. These may include:
- Echocardiogram: To assess heart function and detect issues like heart failure, which can cause fluid buildup in the lungs.
- Pulmonary function tests: Used to evaluate lung capacity and detect conditions like chronic obstructive pulmonary disease (COPD).
- Sleep study: To assess for sleep apnea, a condition that can also contribute to orthopnea and trouble breathing when lying flat.
These tests help your doctor determine the root cause of your symptoms, enabling them to recommend the most appropriate treatment.
Effective Treatment and Management of Orthopnea
Medications and Therapies
The treatment of orthopnea primarily focuses on managing the underlying conditions that cause the shortness of breath. In many cases, medications are used to address these conditions. Diuretics are commonly prescribed for individuals with heart failure to reduce fluid buildup in the lungs. Oxygen therapy may also be recommended for those with respiratory conditions like chronic obstructive pulmonary disease (COPD) to help improve oxygen levels and reduce breathlessness. For conditions such as sleep apnea, continuous positive airway pressure (CPAP) therapy may be used to help keep the airways open during sleep, preventing interruptions to breathing.
Lifestyle Modifications
In addition to medications, certain lifestyle changes can help reduce the symptoms of orthopnea. Consider the following:
- Maintaining a healthy diet and managing weight are key factors in reducing the pressure on the diaphragm and improving lung function.
- Regular physical activity can strengthen the heart and lungs, which may help alleviate some of the breathing difficulties associated with orthopnea.
- Consulting with a healthcare provider before starting an exercise program, especially for individuals with heart or lung conditions.
Positioning and Sleep Adjustments
Adjusting sleep positions is another practical step that can help manage orthopnea. Consider these strategies:
- Sleeping with the head elevated, using extra pillows, or even sleeping in a recliner can help reduce fluid buildup in the lungs and make breathing easier.
- For children with orthopnea, raising the head of the bed or using specially designed pillows can provide relief.
These positioning strategies are effective in managing symptoms, particularly at night when orthopnea tends to be most problematic.
- Orthopnea is shortness of breath that occurs when lying flat and is relieved by sitting or standing.
- Heart failure is a common cause of orthopnea and trouble breathing when lying flat.
- Orthopnea can also result from lung diseases like COPD, pneumonia, and sleep apnea.
- Other causes include obesity, diaphragm paralysis, pleural effusion, ascites, and anxiety.
- Managing the underlying condition is essential in treating orthopnea.
- Common treatments for orthopnea include medications, lifestyle changes, and oxygen therapy.
- Paroxysmal Nocturnal Dyspnea (PND) is a type of orthopnea that occurs during sleep, often relieved by sitting up.
- What is orthopnea? Orthopnea is shortness of breath that occurs when lying flat, often relieved by sitting up or standing. It is commonly associated with heart failure, sleep apnea, and other conditions.
- Why does orthopnea happen when lying down? When lying flat, gravity affects how fluid is distributed in the lungs, making it harder to breathe, especially in conditions like heart failure or COPD.
- Can orthopnea happen at night? Yes, orthopnea often occurs at night, disturbing sleep and causing people to wake up gasping for air. This can significantly impact sleep quality.
- How can orthopnea be treated? Treatment typically involves addressing the underlying condition. Common treatments include medications like diuretics, oxygen therapy, and lifestyle changes like weight management and regular exercise.
- What is Paroxysmal Nocturnal Dyspnea (PND)? PND is a type of orthopnea that occurs suddenly during sleep, often waking a person up feeling breathless. It is relieved by sitting up or standing.
- What causes paroxysmal nocturnal dyspnea? PND is often linked to heart failure, where fluid accumulates in the lungs during sleep, leading to shortness of breath.
- Can obesity contribute to orthopnea? Yes, obesity can increase pressure on the diaphragm, making it more difficult to breathe when lying down, leading to orthopnea symptoms.
- How does sleep apnea relate to orthopnea? Sleep apnea is a condition where breathing temporarily stops during sleep. It can worsen orthopnea symptoms, especially when lying flat.
- Is anxiety a factor in orthopnea? Yes, anxiety can trigger breathlessness, particularly when lying down, making orthopnea symptoms worse in some individuals.
- Can I manage orthopnea at home? Yes, adjusting sleep positions, such as using extra pillows or sleeping with your head elevated, can provide relief from orthopnea symptoms.