High Blood Pressure in Evening Causes and Health Risks
Evening Blood Pressure: Understanding, Risks, and Management
What Is Evening Blood Pressure?
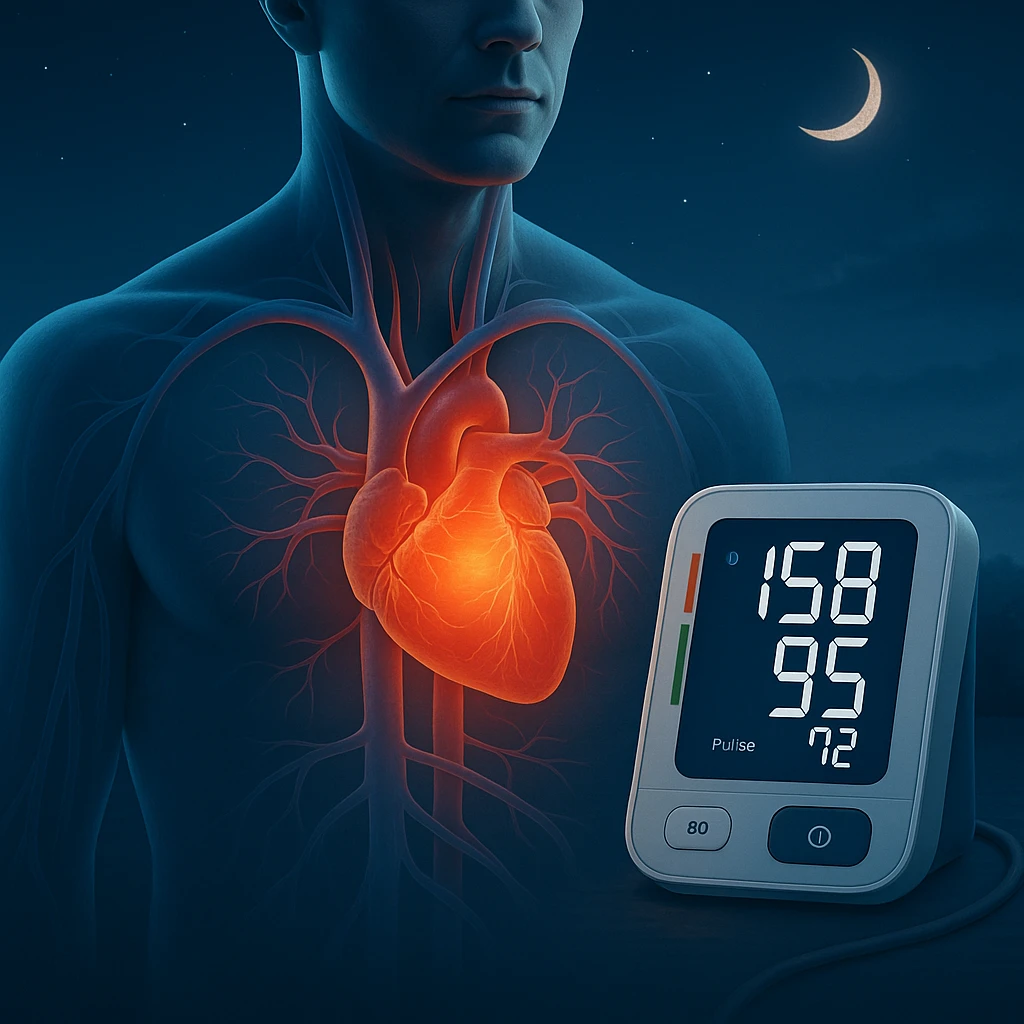
Evening blood pressure refers to the measurements of blood pressure typically taken between 6 pm and 10 pm. Unlike morning or daytime readings, evening values can reveal important cardiovascular patterns that may not be evident during standard clinical visits. For most individuals, blood pressure follows a natural circadian rhythm — it rises during the day to support activity and gradually decreases at night during sleep.
However, some people do not experience this expected nighttime decline. Instead, their blood pressure may remain elevated or even increase during the evening or night. These variations are classified as:
- Non-dipping pattern — blood pressure fails to decrease at night as expected.
- Reverse-dipping pattern — blood pressure increases during the evening or nighttime hours.
Both patterns are associated with a higher risk of cardiovascular disease, including heart attack and stroke. Understanding evening blood pressure variations helps identify individuals who may require closer monitoring or adjusted therapy.
Prevalence and Health Implications
Evening high blood pressure is more common than many realize. Studies show that elevated readings during early evening hours affect over 40% of adults undergoing 24-hour monitoring. Among people with diagnosed hypertension, up to two-thirds experience elevated evening blood pressure.
These elevations are not simply numbers — they represent ongoing stress on the cardiovascular system. Both evening and nighttime hypertension are linked to increased risk of stroke, heart disease, and kidney complications. Persistent elevation during evening hours can accelerate arterial stiffness and impair heart function over time.
People most at risk include those with pre-existing hypertension, disrupted sleep-wake cycles, irregular medication schedules, and conditions that affect autonomic regulation such as diabetes or sleep apnea.
How to Manage Elevated Evening Blood Pressure
Effective management of evening blood pressure requires a combination of targeted medication timing, lifestyle changes, and continuous monitoring. One proven strategy is chronotherapy — adjusting the timing of antihypertensive medication to align with an individual’s circadian rhythm.
The 2025 OMAN Trial demonstrated that bedtime dosing of antihypertensive medications reduced nighttime systolic blood pressure by approximately 3 mm Hg compared to morning dosing. This approach supports better 24-hour blood pressure control and may enhance cardiovascular protection.
In addition to medication timing, lifestyle adjustments play a vital role. Key strategies include:
- Reducing sodium intake and avoiding heavy evening meals
- Maintaining consistent physical activity
- Limiting caffeine and alcohol in the evening
- Managing stress through relaxation techniques or mindfulness
Patients should establish regular home monitoring routines, measuring blood pressure at the same time each evening. This helps clinicians assess patterns and optimize treatment schedules.
Emerging Research and Future Directions
Recent studies identify evening blood pressure as an important and modifiable cardiovascular risk factor. Efforts are underway to establish standardized diagnostic criteria for “evening hypertension,” which will improve detection and treatment consistency across clinical settings.
Technological innovation is driving progress in this area. Advanced monitoring tools now allow for better data collection and personalized care:
- Wearable, cuffless monitors providing continuous, non-invasive measurements
- Smart home devices tracking daily blood pressure variations
- AI-driven analytics that predict hypertension risk based on evening trends
These developments are transforming patient engagement, making self-monitoring easier and more accurate. Both clinicians and patients can now respond more effectively to evening blood pressure changes, reducing long-term cardiovascular risk.
Frequently Asked Questions: High Blood Pressure in the Evening
- Why does blood pressure sometimes rise in the evening?
- Evening blood pressure can rise due to stress, disrupted sleep cycles, medication timing, or autonomic dysfunction.
- Is evening hypertension more dangerous?
- Yes. Persistent evening elevation increases the risk of stroke, heart disease, and kidney damage due to prolonged vascular strain.
- How can wearable devices help?
- Wearables track blood pressure throughout the evening and night, identifying fluctuations that traditional measurements may miss.
- What lifestyle habits influence evening blood pressure?
- High sodium intake, late heavy meals, lack of physical activity, alcohol, and stress all contribute to elevated evening readings.
- Does bedtime medication help?
- Evidence shows bedtime dosing can significantly reduce evening and nighttime blood pressure by aligning medication effect with biological rhythms.
- How often should I check my evening blood pressure?
- Measure at least 3–4 times per week, at the same time each evening, to identify consistent trends.
- Can evening hypertension occur without daytime hypertension?
- Yes, it can appear in people with normal daytime readings, serving as an early indicator of developing hypertension.
- What are warning signs of problematic evening blood pressure?
- Consistently high readings, headaches, fatigue, or difficulty sleeping may signal underlying issues that need medical attention.
- How does managing evening blood pressure improve health?
- Proper control lowers the heart’s workload overnight, reduces vascular stress, and decreases long-term cardiovascular risks.
- What’s next in research?
- New technologies, AI-based prediction models, and personalized chronotherapy protocols are expected to redefine hypertension management in coming years.