Prostate Cancer Treatment Options: Radiation, Hormone Therapy, and New Approaches in 2025
“In my 12 years of medical practice, I have often met patients who discovered a lump on their neck and felt immediate concern. While cancer is always something to rule out, most neck lumps are not dangerous — they may be swollen lymph nodes after an infection, benign cysts, or lipomas. In this guide, I will walk you through which neck lumps truly need urgent medical attention, how doctors approach diagnosis, and the treatment options available.”
Hearing the words “prostate cancer” can feel overwhelming. The good news is that in 2025 men have more prostate cancer treatment options than ever before. Choices range from active surveillance and surgery to radiation therapy for prostate cancer and advanced hormone-based approaches. The right decision not only helps control the disease but also protects quality of life.
From my own medical practice, I know that no two cases are alike. Age, stage of cancer, overall health, and personal goals all play a role in choosing therapy. In this article, we will review the most common methods, explain how many radiation therapy sessions for prostate cancer are usually needed, discuss hormone therapy for prostate cancer, and highlight new advances available in the USA in 2025. My goal is to give you clear, evidence-based guidance so you can talk confidently with your doctor about the best path forward.
Why the Right Treatment Choice Matters
Choosing the right treatment for prostate cancer makes a direct impact on survival, long-term health, and quality of life. With more therapies available in 2025, patients and doctors need to balance medical effectiveness with personal goals.
How stage and grade influence decisions
Doctors determine treatment based on two critical factors: the stage of the cancer (how far it has spread) and the grade (how aggressive the tumor looks under the microscope). Early-stage prostate cancer may not require immediate aggressive action, while advanced cases often need a combination of therapies.
For example, a low-grade, localized tumor might be managed with active surveillance or targeted radiation, while a high-grade tumor that shows rapid growth usually calls for surgery or systemic therapy. Understanding these details helps patients choose a plan that matches the seriousness of their condition.
Why personalized care is growing in importance
Prostate cancer is not the same disease for every man. Genetics, age, other health issues, and lifestyle all change how the body responds to treatment. Personalized care takes these factors into account, rather than applying one standard approach to everyone.
In 2025, doctors use advanced imaging, genetic testing, and biomarker analysis to tailor therapy. This ensures that each man receives treatment that not only targets the cancer but also respects his overall well-being, minimizing side effects and supporting long-term recovery.
Current Treatment Paths for Prostate Cancer
Men diagnosed with prostate cancer today face several established treatment methods. Doctors consider the tumor’s behavior, the patient’s age, and health profile before recommending surgery, radiation, hormone therapy, or careful monitoring.
Active surveillance and watchful waiting
Active surveillance means closely tracking prostate cancer without starting immediate treatment. Doctors schedule regular PSA tests, imaging, and occasional biopsies to make sure the disease remains stable. This option works best for men with slow-growing, early-stage tumors.
Watchful waiting differs slightly: it focuses less on frequent testing and more on managing symptoms if they appear. This path often suits older men or those with other health conditions where aggressive treatment could cause more harm than benefit. Both strategies help patients avoid side effects until treatment truly becomes necessary.
Surgery (radical and robotic approaches)
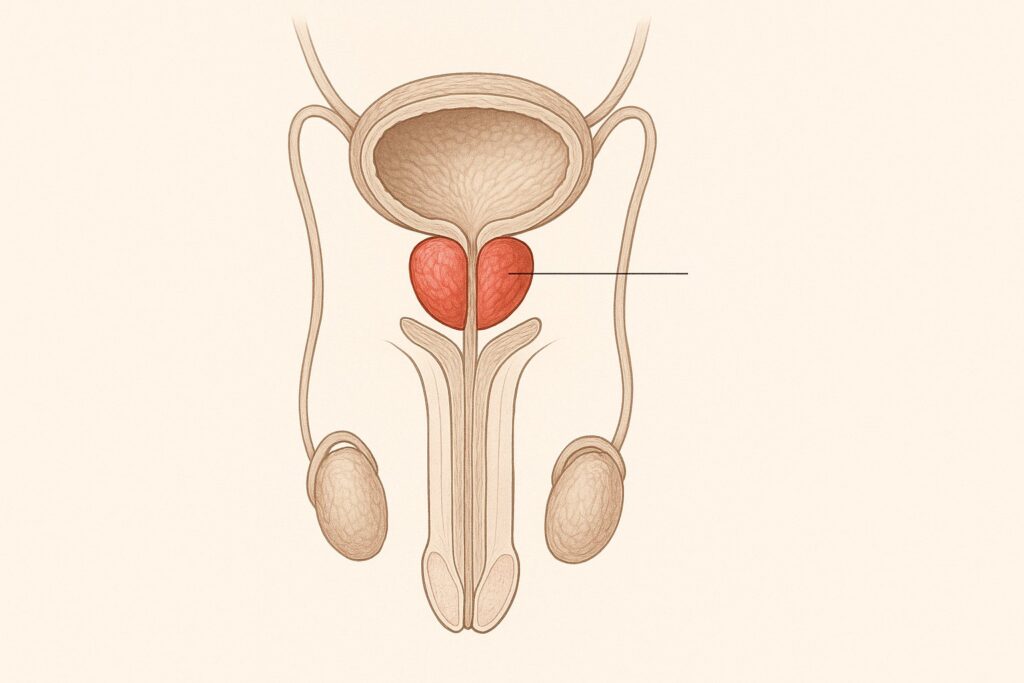
Radical prostatectomy removes the entire prostate gland and sometimes nearby lymph nodes. This option suits men with cancer limited to the prostate and good overall health. It offers the chance of complete removal of the disease when performed early.
Robotic-assisted surgery has become common in the USA. It allows greater precision, smaller incisions, and faster recovery compared with traditional open surgery. Patients often experience less blood loss and shorter hospital stays, though side effects such as urinary leakage or erectile dysfunction can still occur.
Radiation — one of the main options
Radiation therapy remains one of the most widely used treatments for prostate cancer. It targets cancer cells with high-energy beams, aiming to destroy them while sparing surrounding tissues. Doctors often recommend it for men who want a non-surgical option or are not candidates for surgery.
Modern techniques such as image-guided radiation make the treatment more accurate and reduce complications. Radiation can cure localized cancer and also control disease that has spread beyond the prostate. Side effects exist, but advances in 2025 continue to make therapy safer and more effective.
Radiation in Detail
Radiation therapy plays a central role in prostate cancer treatment. Advances in technology have improved accuracy, reduced side effects, and expanded choices for patients in 2025.
External beam radiation vs brachytherapy
External beam radiation delivers high-energy rays from outside the body directly to the prostate. Doctors plan each session with detailed imaging, making sure the beams strike only the tumor. This approach suits men with localized or locally advanced cancer and often requires multiple sessions over several weeks.
Brachytherapy works differently. Doctors place tiny radioactive seeds inside the prostate, where they release radiation over time. This method targets the cancer internally with less exposure to surrounding organs. Brachytherapy is often chosen for men with low- to intermediate-risk cancer who prefer a shorter treatment course.
How many sessions are usually required
External beam radiation for prostate cancer typically involves 20 to 45 sessions, spread over four to nine weeks. Each visit lasts only a few minutes, but consistency matters because smaller daily doses protect healthy tissue while effectively targeting the tumor.
Some clinics now offer hypofractionated schedules, where higher doses are delivered in fewer sessions. These shorter courses can finish in about four to six weeks and have shown similar success rates. The choice depends on cancer risk, patient health, and the technology available at the treatment center.
Side effects patients should be aware of
Radiation can cause urinary urgency, frequent trips to the bathroom, and mild burning during urination. Some men notice temporary changes in bowel habits, such as looser stools or rectal irritation. These effects usually appear gradually during treatment and improve after therapy ends.
Long-term side effects may include erectile dysfunction or persistent urinary leakage, though modern techniques in 2025 have lowered these risks. Talking openly with the care team helps men prepare for potential changes and learn strategies to manage them effectively.
Hormonal Treatment and Its Role
Hormone therapy, also called androgen deprivation therapy (ADT), remains a cornerstone of prostate cancer treatment in 2025. Doctors often use it when the cancer has spread, returned after local treatment, or needs to be combined with radiation for stronger results.
How androgen deprivation therapy works
Prostate cancer cells grow in response to male hormones, mainly testosterone. ADT lowers testosterone levels or blocks its effect on cancer cells, slowing or stopping tumor growth. Doctors achieve this either with medications that suppress hormone production or with drugs that block receptors on cancer cells.
In practice, ADT does not cure the disease but keeps it under control, sometimes for many years. Patients often notice improvements in symptoms like bone pain or urinary blockage. Understanding how the therapy works helps men see why it is used alongside other treatments rather than as a stand-alone cure.
Common drugs used in the US
Doctors in the United States often prescribe LHRH agonists or antagonists to reduce testosterone production. Popular options include leuprolide, goserelin, degarelix, and relugolix. These drugs are given as injections or tablets and form the backbone of androgen deprivation therapy.

Anti-androgens such as bicalutamide, enzalutamide, and apalutamide block the effect of testosterone on cancer cells. Sometimes doctors combine these with LHRH drugs to maximize control. The choice depends on the cancer stage, previous treatments, and the patient’s health profile.
Managing long-term side effects
Long-term hormone therapy can cause hot flashes, weight gain, bone thinning, fatigue, and decreased sexual function. These changes affect both physical health and emotional well-being, so proactive management is important.
Doctors often recommend exercise, healthy diet, and medications to protect bone strength. Counseling and support groups also help men cope with emotional effects. By addressing side effects early, patients can stay on treatment longer and maintain a good quality of life.
Choosing the Best Option for Early-Stage Cancer
When prostate cancer is detected early, men often face several safe and effective treatment paths. The decision should balance cancer control with preservation of quality of life.
Comparing surgery, radiation, and surveillance
Surgery offers the possibility of removing all cancer at once. It suits men with good overall health who want a direct solution, though risks include urinary leakage and erectile problems.
Radiation therapy provides a non-surgical option with excellent success rates. It is less invasive and often chosen by men who prefer to avoid surgery, though it may require weeks of sessions and can also affect sexual and urinary function. Active surveillance avoids immediate side effects altogether by delaying treatment until it becomes necessary, but it requires regular testing and close follow-up.
Factors that help decide the best path
Doctors consider age, tumor aggressiveness, PSA level, and other health conditions when advising patients. Younger men often lean toward surgery or radiation for long-term control, while older men may choose surveillance if the tumor grows slowly.
Lifestyle and personal goals matter as well. Some men prioritize avoiding treatment side effects, while others prefer the certainty of immediate therapy. Talking through these factors with a trusted doctor helps find the balance between effective cancer control and maintaining daily life.
Latest Advances and New Approaches in 2025
In recent years, prostate cancer therapy has moved beyond surgery, radiation, and hormone therapy. In 2025, patients benefit from targeted drugs, immunotherapy, and precision treatments guided by new imaging and biomarkers.
Targeted drugs and immunotherapy
Targeted drugs focus on specific weaknesses inside cancer cells. PARP inhibitors, for example, block DNA repair in tumors with BRCA mutations, making it harder for cancer to survive. These medicines are taken orally and often work well for men whose cancer resists standard hormone therapy.
Immunotherapy trains the body’s own defense system to recognize and attack prostate cancer. Checkpoint inhibitors and experimental vaccines are now available through clinical trials in the USA. While not every patient responds, these treatments represent a powerful new option for men with advanced or treatment-resistant disease.
PSMA-directed treatments
PSMA-directed therapy targets a protein found on the surface of most prostate cancer cells. Doctors attach radioactive particles to molecules that bind to PSMA, delivering radiation directly to the tumor while sparing healthy tissue. This method has shown strong results for men with advanced cancer who no longer respond to hormone therapy.
In 2025, PSMA PET scans also help doctors locate even tiny spots of cancer. By combining advanced imaging with PSMA-targeted drugs, physicians can both detect and treat disease with greater precision than before.
Clinical trials to watch in the US
Across the United States, clinical trials are testing new drug combinations, advanced immunotherapies, and improved radiation schedules. These studies give patients access to cutting-edge treatments while contributing to future standards of care.
Some trials explore shorter radiation courses with equal effectiveness, while others test next-generation hormone blockers or novel vaccines. For men who qualify, participation offers the chance to benefit from tomorrow’s therapies today.
Life After Treatment
Completing prostate cancer therapy marks the beginning of a new stage. Recovery involves not only follow-up medical care but also attention to physical function, emotional well-being, and long-term health.
Sexual health and urinary recovery
Many men notice changes in sexual function after surgery, radiation, or hormone therapy. Erections may take time to return, and some men need medications, devices, or counseling. Open conversations with doctors and partners reduce stress and support gradual recovery.
Urinary control also improves slowly. Pelvic floor exercises, physical therapy, and, in some cases, medications help men regain strength. While setbacks happen, most patients see steady progress when they stay consistent with recovery strategies.
Lifestyle changes that support healing
Healthy habits make recovery smoother and lower the risk of cancer returning. Regular exercise improves energy, strengthens bones, and helps control weight. A balanced diet rich in fruits, vegetables, lean protein, and whole grains supports the immune system and overall health.

Avoiding smoking and limiting alcohol also improve outcomes. Men who adopt these changes often report faster recovery, better mood, and more confidence in managing long-term health after prostate cancer treatment.
Emotional and psychological support
Living through cancer affects more than the body. Anxiety, fear of recurrence, and changes in identity can weigh heavily on patients. Talking openly with mental health professionals or joining support groups helps men process these feelings.
Family involvement also matters. When partners and relatives understand the challenges of recovery, men feel less isolated and more motivated to follow medical advice. Emotional support strengthens resilience and improves quality of life after treatment.
Insights From Practice
Years of working with men facing prostate cancer have shown me that clear communication matters as much as medical treatment. Patients want straightforward answers and reassurance that their concerns are heard.
Common concerns men share with doctors
The most frequent question is about survival: “Will I live to see my family milestones?” Men also worry about sexual health, urinary control, and how quickly they can return to work or normal routines. These questions reflect the fear of losing independence and quality of life.
Another common concern is treatment side effects. Patients want to know how severe they will be and whether the effects are permanent. By addressing these concerns directly, doctors can reduce anxiety and help men focus on realistic outcomes instead of worst-case scenarios.
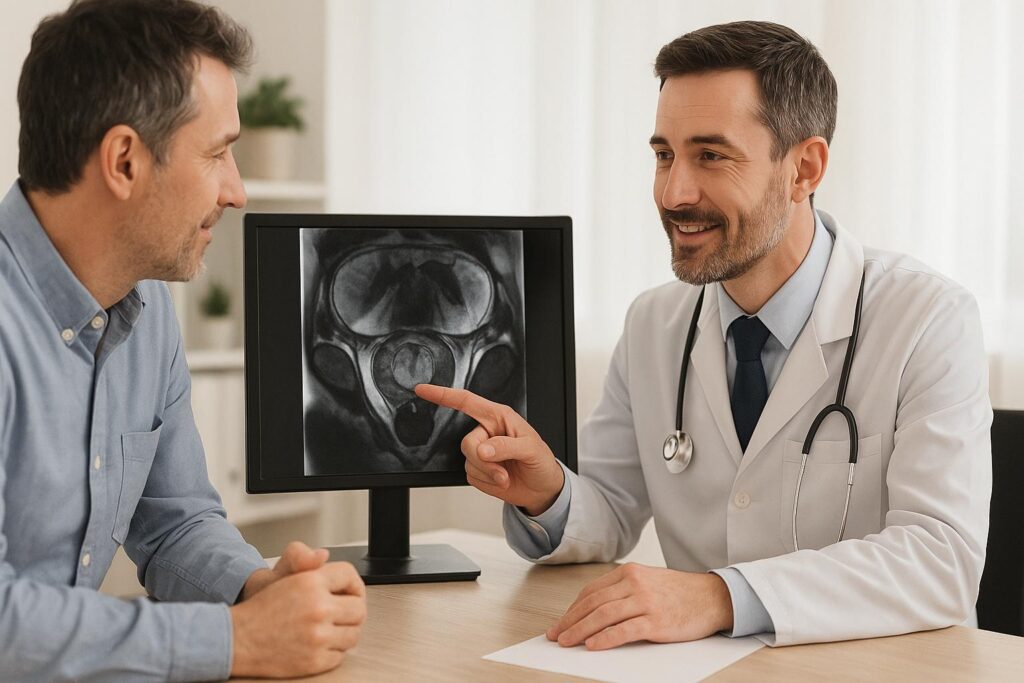
How I explain options to my patients
When I sit with a patient, I explain every treatment path in plain language. I describe how surgery, radiation, or hormone therapy works, what benefits each brings, and what risks to expect. I make sure the patient understands not only the medical facts but also how each choice may affect daily life.
I often use examples from other men who faced similar situations. This helps patients see that recovery is possible and that side effects can be managed. My goal is always to replace fear with clarity so the decision feels informed, not rushed.
Key questions to ask your doctor
Men benefit most when they prepare questions before appointments. Good ones include: “Which treatments fit my stage of cancer?”, “What side effects should I expect in the short and long term?”, and “How will this affect my sexual and urinary health?”
Other important questions cover recovery time, the need for follow-up tests, and how new therapies in 2025 might apply. By asking directly, patients take an active role in their care and build trust with their medical team.
FAQ on Prostate Cancer Treatment (2025 Update)
When to Consult a Doctor
| Situation | Why It Matters |
|---|---|
| New diagnosis of prostate cancer | A specialist explains all treatment paths and tailors care to your stage and health. |
| Rising PSA after treatment | An early sign that cancer may have returned or progressed. |
| Severe side effects | Hot flashes, urinary problems, or pain need timely management. |
| Questions about new therapies | Doctors can explain if you qualify for the latest treatments or trials in 2025. |
Expert’s Closing Note
“As a physician, I know how difficult it feels to face choices about prostate cancer treatment. In 2025, men have more effective and safer options than ever before, including surgery, radiation, hormone therapy, and new targeted drugs. My advice is simple: talk openly with your doctor, ask every question, and choose the plan that protects both your health and your quality of life. Early, informed decisions lead to the best possible outcomes.”