Prostate Biopsy: Procedure, Risks, and Patient Guide
“In my 12 years of medical practice, I have often met patients who felt anxious when told they needed a prostate biopsy. While the word ‘biopsy’ can sound frightening, it is an essential test that helps doctors confirm whether prostate changes are cancerous or harmless. In this guide, I will explain when a prostate biopsy is recommended, how the procedure is performed, and what patients can expect before and after the test.”
A prostate biopsy is one of the most important steps in diagnosing prostate conditions, especially when PSA levels are elevated or doctors notice changes on imaging. For many men, the word “biopsy” sounds alarming, but in reality this test is safe, quick, and provides doctors with the information they need to decide on the right treatment. In this article, I will explain what a prostate biopsy is, why it’s done, how the procedure works, and what to expect before and after.
What Is a Prostate Biopsy and Why Is It Done?
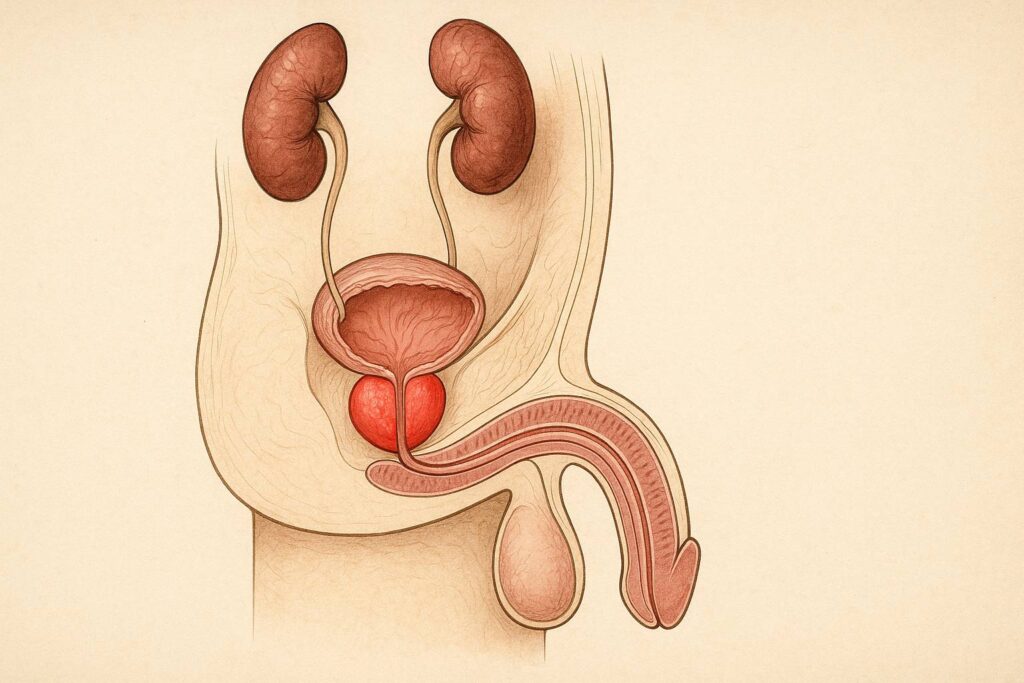
A prostate biopsy is a diagnostic procedure in which doctors take tiny samples of tissue from the prostate gland. These samples are then examined under a microscope to detect cancerous or abnormal cells. The test is usually suggested when PSA (prostate-specific antigen) levels rise, or when scans and physical exams show changes that cannot be explained otherwise. The main purpose is clarity: to know whether the prostate is healthy or showing early disease.
Why doctors recommend this test
Doctors recommend a prostate biopsy when other findings suggest something unusual in the prostate. Elevated PSA levels are one of the most common reasons. PSA is a protein produced by the prostate, and when its value goes above the normal range, it may signal inflammation, benign enlargement, or sometimes prostate cancer. Since PSA alone cannot give a final answer, a biopsy becomes the next step.
Another common reason is an abnormal digital rectal exam. When a physician feels a hard nodule or asymmetry in the gland, a biopsy helps clarify what exactly is happening inside. In my own practice, I have often seen men panic after hearing that “something feels different.” A biopsy allows us to move from fear and uncertainty to evidence and clarity.
How a tissue sample helps confirm diagnosis
The tissue taken during a biopsy is carefully studied by a pathologist, a doctor who specializes in identifying diseases under the microscope. This direct look at the cells is what makes biopsy the most reliable way to confirm or rule out prostate cancer. No blood test or imaging scan can replace the accuracy of seeing how prostate cells behave and whether they look normal or malignant.
Each tiny core of tissue gives a snapshot of the prostate’s health. When cells are organized and uniform, results are usually benign. When the architecture looks disrupted or aggressive, the report indicates cancer and its grade. By analyzing these patterns, doctors can explain the situation clearly to patients and decide on the best course of action. Without this tissue sample, both patient and doctor would remain uncertain, and treatment decisions would be based on guesses rather than facts.
Main Types of Prostate Biopsy
There are several ways to collect tissue from the prostate, and the choice of method depends on the patient’s health, available technology, and the doctor’s preference. Each approach has its own advantages and potential drawbacks. The two most common techniques are transrectal and transperineal biopsies. Let’s look at how each one works in practice.
Transrectal biopsy (TRUS-guided)
The transrectal ultrasound-guided biopsy, often called TRUS biopsy, is the most widely used technique worldwide. In this method, the doctor inserts a small ultrasound probe into the rectum. The probe produces real-time images, which help guide a thin needle into the prostate. Through this pathway, the doctor collects several tiny cores of prostate tissue, usually between 10 and 12 samples.
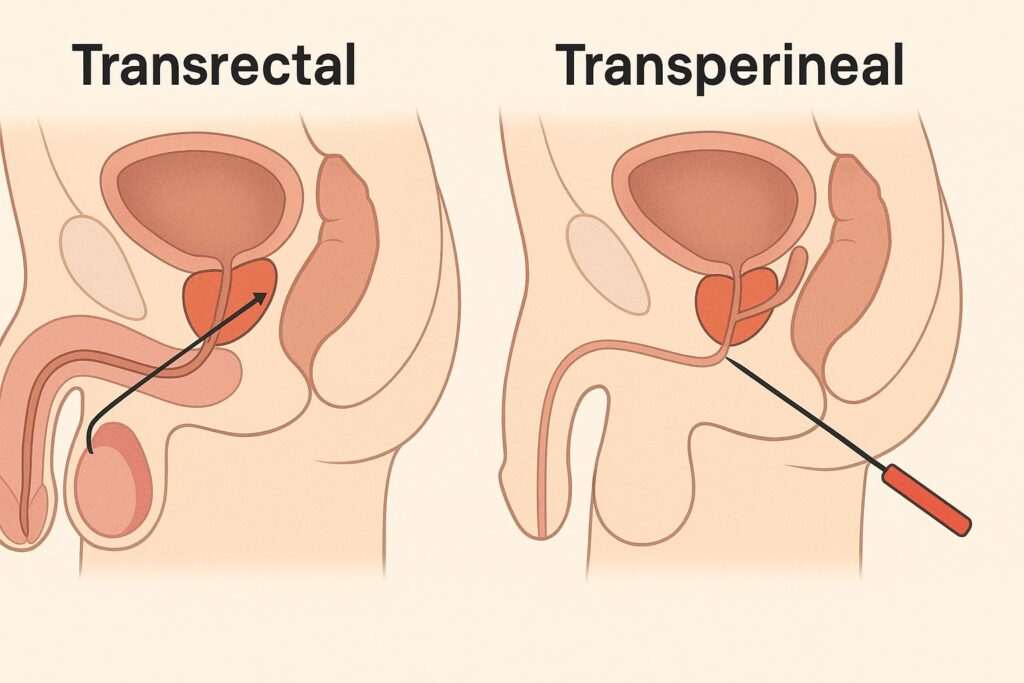
This approach has remained popular because it is relatively quick, does not require complex equipment, and can often be performed in an outpatient clinic. Many of my patients are surprised by how short the procedure is — typically less than 20 minutes. Local anesthesia is used to minimize discomfort, and most men tolerate it well.
However, the transrectal route also carries some specific risks. Because the needle passes through the rectum, there is a chance of introducing bacteria into the prostate or bloodstream, which may lead to infection. To reduce this risk, doctors routinely prescribe antibiotics before and after the test. While complications are uncommon, patients should always be informed about both the benefits and the possible downsides of this technique.
Transperineal biopsy
In a transperineal biopsy, the needle reaches the prostate through the skin between the scrotum and the anus — a region called the perineum. Instead of passing through the rectum, the doctor makes tiny punctures in this area, guided by ultrasound images. Several samples are taken, often with a grid system that helps cover different zones of the prostate more evenly.
One of the main benefits of the transperineal approach is the reduced risk of infection. Because the needle does not go through the rectum, it avoids contact with bacteria that can cause complications. This technique also gives better access to areas of the prostate that are sometimes difficult to reach with the transrectal route, especially the anterior part of the gland.
Patients sometimes worry that punctures through the skin may hurt more, but local or general anesthesia is usually applied. In my practice, men who undergo transperineal biopsy often report similar or even less discomfort compared with the transrectal method. The main downside is that it usually requires a more specialized setup, which means it is not available in every clinic.
Which approach is safer and more accurate?
Both transrectal and transperineal biopsies aim to achieve the same goal — collecting reliable tissue samples for diagnosis. The difference lies in safety and accuracy. Transrectal biopsy remains more common because it is simpler and quicker, but it carries a higher chance of infection. Transperineal biopsy, on the other hand, is increasingly preferred for its lower infection risk and better coverage of the whole prostate.
From an accuracy perspective, studies show that the transperineal route may detect cancers that the transrectal approach misses, especially in the front and side zones of the prostate. For patients with repeatedly elevated PSA but negative transrectal biopsies, switching to a transperineal method often provides answers.
When I discuss options with patients, I explain that neither method is “perfect.” The choice depends on medical history, available resources, and the experience of the urologist. In clinics with the right equipment, transperineal biopsy is becoming the safer and more accurate option. Still, for many men, the transrectal technique remains a reasonable and effective first step.
Step-by-Step: How Doctors Perform a Biopsy
Understanding the steps of a prostate biopsy helps reduce fear and makes the whole process easier to handle. Men often arrive nervous because they don’t know what will happen. By breaking the procedure down into preparation, the test itself, and the recovery phase, patients can walk in more confident and leave with fewer surprises.
Preparing for the procedure
Before the biopsy, doctors usually order blood and urine tests to check overall health and rule out infection. If the patient takes blood thinners such as warfarin or aspirin, the urologist will discuss stopping or adjusting these medications to lower the risk of bleeding. Antibiotics are prescribed to reduce the chance of infection, especially for the transrectal approach.
On the day of the biopsy, patients are asked to come with an empty rectum, sometimes after using a mild enema. In my practice, I always explain these details clearly — following the instructions carefully makes the procedure smoother and safer. Some clinics also offer light sedation for anxious patients, while others rely on local anesthesia alone.
What happens during the test

Once the patient is ready, the doctor applies local anesthesia to numb the area. If the biopsy is transrectal, an ultrasound probe is gently placed into the rectum to guide the needle. For a transperineal biopsy, the probe is positioned on the skin near the perineum. Using ultrasound images, the doctor advances a fine needle into specific areas of the prostate and collects tissue cores.
Typically, 10 to 12 samples are taken, but in some cases more are needed, especially if MRI has shown suspicious zones. The entire process usually lasts 15 to 30 minutes. Most patients are surprised by how quickly it is over. During the biopsy, a clicking sound is heard as the spring-loaded needle captures each tissue sample — this is normal and expected.
What patients usually feel
With anesthesia, most men describe the procedure as uncomfortable rather than painful. The initial pressure of the ultrasound probe or the skin puncture can feel odd, but the needle itself is usually felt only as a brief pinch. Anxiety often causes more distress than the physical sensations. That is why I always talk patients through each step; hearing what comes next reduces fear significantly.
After the biopsy, mild soreness or a dull ache in the pelvic area is common for a few days. Some men notice a small amount of blood in urine, semen, or stool — this is normal and usually fades on its own. The majority return to normal activities within 24 to 48 hours, though heavy exercise or sexual activity is best avoided until the doctor gives the all clear.
Possible Risks and Complications
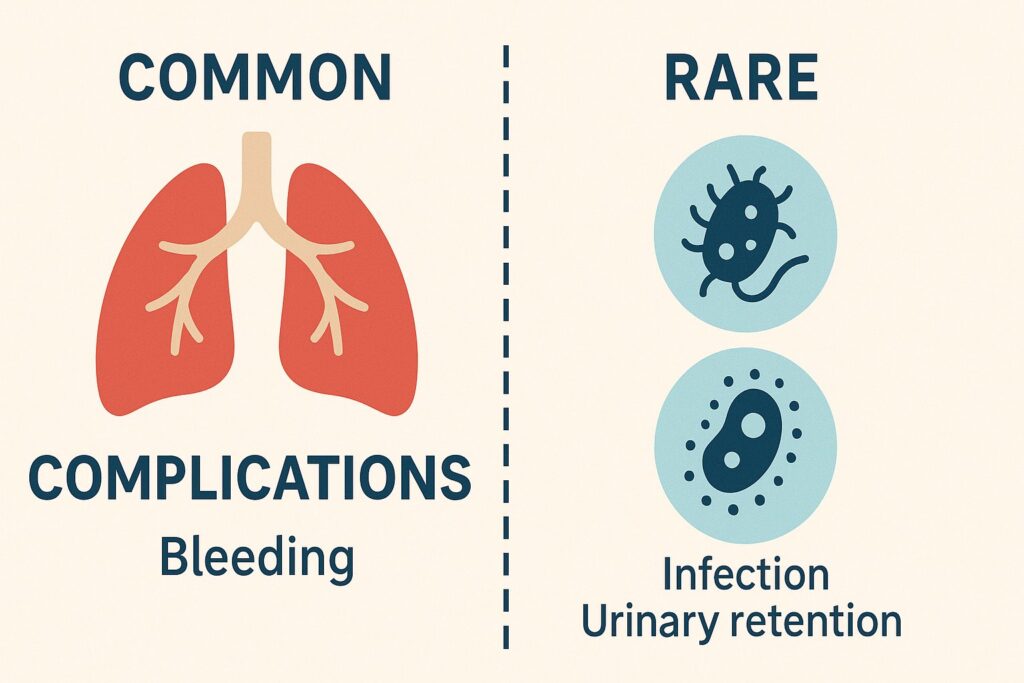
Every medical test carries some level of risk, and a prostate biopsy is no exception. Most men experience only mild and temporary side effects, but it is important to know what to expect so you don’t panic over normal reactions.
Common short-term effects
After a biopsy, many men notice a small amount of blood in the urine, semen, or stool. This effect looks alarming, but it usually fades within a few days. The biopsy needle passes through delicate tissue, so minor bleeding is almost inevitable. Doctors warn patients about this in advance so they understand it as part of the healing process.
Mild soreness or discomfort in the pelvic area is also common. Some men describe it as a dull ache that feels similar to a muscle bruise. Over-the-counter pain relievers and rest usually help. In my practice, I tell patients that they can return to light daily activities quickly, but they should avoid heavy exercise or cycling until the soreness disappears.
Rare but serious problems
Although most men recover quickly after a prostate biopsy, a few may face more serious issues. The most important one is infection. Because the needle can introduce bacteria, especially in the transrectal method, a small number of patients develop fever, chills, or painful urination. Doctors reduce this risk by prescribing antibiotics, but if symptoms of infection appear, immediate medical care is essential.
Another rare problem is significant bleeding. While minor blood traces are normal, heavy bleeding in urine or stool requires urgent attention. In very rare cases, men may have difficulty passing urine because of swelling or blood clots in the urethra. In my practice, I emphasize that these situations are unusual but possible, and knowing the warning signs helps patients react quickly if they occur.
“Don’t get a biopsy”: myths and facts explained
Some men read alarming stories online and decide that “you should never get a biopsy.” This statement is misleading. The truth about prostate biopsy is that while it does carry risks, it remains the only reliable way to confirm or rule out cancer. Without tissue samples, doctors cannot make an accurate diagnosis, and treatment decisions would be based on guesses.
A common myth is that biopsy always “spreads cancer.” Research shows no evidence that taking tissue samples makes cancer grow faster or spread. Another myth claims that “a high PSA always means cancer,” so biopsy is unnecessary. In reality, PSA can rise for many reasons, such as infection or benign enlargement. A biopsy clarifies the cause. In my experience, once patients understand these facts, their fear decreases and they see biopsy as a rational, necessary step.
Recovery and Aftercare Tips
The days after a prostate biopsy matter just as much as the procedure itself. Knowing what is normal and what requires attention helps patients recover with less stress and avoid unnecessary worry.
What to expect in the first days
During the first two or three days, most men notice mild soreness in the pelvic area and small amounts of blood in urine, semen, or stool. These effects are common and usually fade on their own. The body needs time to heal from the tiny punctures made during the biopsy. I always explain to patients that these signs are part of the natural recovery process, not a sign of something going wrong.
Men can usually return to light daily activities the same day or the next. However, doctors advise avoiding heavy lifting, cycling, or sexual activity until the discomfort disappears. Fatigue is also common, especially if sedation or anesthesia was used. In my practice, I recommend taking the first evening easy — rest, hydrate well, and allow the body to adjust.
Warning signs that need urgent care
Most men recover without problems, but a few may face warning signs that require immediate medical attention. If you develop a high fever, chills, or severe burning when urinating, call your doctor right away. These symptoms suggest an infection that needs quick treatment with stronger antibiotics or hospital care.
Heavy bleeding is another red flag. A few drops of blood are normal, but if urine turns bright red, if clots appear, or if you cannot pass urine at all, you must seek urgent help. In my practice, I tell patients to trust their instincts: if something feels worse than expected, it is safer to contact a doctor than to wait and hope it improves on its own.
How to support faster healing
You can support recovery by giving your body time to rest. Drink plenty of fluids to flush the urinary tract and help the healing process. Eat light, balanced meals and avoid alcohol for a few days, as it can irritate the bladder and increase bleeding risk. Gentle walking is fine, but save intense workouts or long bike rides for later.
Emotional recovery also matters. Anxiety after a biopsy is common, especially while waiting for results. I encourage patients to talk openly with their family or their doctor about concerns instead of holding them inside. Practicing relaxation techniques such as deep breathing or meditation can reduce stress and help the body heal more smoothly.
Understanding Biopsy Results
Once the biopsy samples reach the lab, the pathologist studies them under a microscope. The report that follows gives doctors and patients the information needed to decide on treatment or continued observation. Understanding these results can feel overwhelming, but clear explanations help men see what the numbers and terms really mean.
What a Gleason score means
The Gleason score describes how aggressive prostate cancer looks under the microscope. The pathologist grades the two most common patterns of cancer cells, each on a scale from 1 to 5, and then adds them together. For example, a score of 3+4=7 means the most common pattern is grade 3 and the second is grade 4. Higher numbers indicate that the cancer cells look more abnormal and may grow faster.

In practice, doctors use the Gleason score to guide treatment. A low score such as 6 usually suggests slow-growing cancer that may not need immediate intervention. Scores of 7 or higher indicate a higher risk and often lead to active treatment options like surgery or radiation. In my practice, I explain the Gleason score in plain language: it is a roadmap that shows both the patient and the doctor how urgent the situation is and what options make the most sense.
When results are inconclusive
Sometimes the pathologist cannot give a clear answer from the first biopsy. The report may say that the tissue shows atypical cells — changes that look suspicious but not clearly cancerous. This situation frustrates patients, but it does not mean the test failed. It means the prostate needs a closer look.
In such cases, doctors usually recommend repeating the biopsy, sometimes with MRI guidance to target suspicious areas more precisely. I tell my patients that an “inconclusive” result is not a dead end but a signal to gather more information. Clear answers often appear after a second or targeted biopsy, which helps avoid both under-treatment and unnecessary treatment.
Next steps if cancer is detected
When the biopsy confirms cancer, the doctor explains the stage, Gleason score, and treatment options. The next step depends on how aggressive the cancer looks and whether it has spread beyond the prostate. For many men with low-risk disease, active surveillance with regular checkups is enough. For higher-risk cases, surgery or radiation usually becomes part of the plan.
In my practice, I emphasize that a cancer diagnosis is not the same as an emergency. Patients often imagine the worst, but the majority of prostate cancers grow slowly. Taking time to review options with the medical team helps each man choose a treatment path that fits his health, age, and personal goals.
Alternatives and New Technologies
Biopsy techniques continue to evolve. Traditional approaches still work well, but newer technologies help doctors make the procedure safer and more precise. These advances reduce unnecessary samples, lower risks, and give patients clearer answers.
MRI-guided biopsies
MRI-guided biopsy combines magnetic resonance imaging with ultrasound to pinpoint suspicious areas in the prostate. The doctor first reviews an MRI scan to identify regions that look abnormal. During the procedure, software fuses MRI images with real-time ultrasound, guiding the needle directly into the targeted zone. This method allows doctors to sample fewer areas while still capturing the spots most likely to contain cancer.
In my practice, I see how MRI guidance improves accuracy, especially for men who had a negative standard biopsy but still show rising PSA levels. It reduces the chance of missing aggressive cancers hidden in hard-to-reach regions of the gland. While this approach requires advanced equipment and is not available in every clinic, patients who undergo MRI-guided biopsy often feel more confident that the test provided reliable information.
Liquid biopsy and genetic testing
Liquid biopsy offers a way to check for cancer without taking tissue directly from the prostate. Instead, doctors analyze a blood or urine sample to look for cancer-related DNA, proteins, or circulating tumor cells. These tests cannot fully replace a standard biopsy yet, but they provide useful clues about whether cancer may be present and how aggressive it might be.
Genetic testing also adds valuable insight. By examining the genes of prostate cells or inherited risk factors, doctors can predict how the cancer may behave and which treatments might work best. In my practice, I use genetic information to personalize care, especially for men with a strong family history of prostate cancer. These tools do not remove the need for biopsy, but they complement it and help guide smarter decisions.
Could biopsies become less invasive in the future?
Researchers continue to develop new techniques to make prostate diagnosis easier and safer. Advances in imaging, biomarkers, and computer-assisted targeting already reduce the need for random sampling. As these technologies improve, doctors may rely more on precision tools and less on taking multiple cores.
I believe the future will bring a shift toward fewer invasive procedures. A combination of imaging, liquid biopsy, and genetic testing could allow doctors to detect and monitor prostate cancer with minimal discomfort. While traditional biopsy will remain important for now, ongoing innovation points toward a future where men face less pain, fewer risks, and faster answers.
Patient Concerns and Expert Advice
Many men feel anxious when they hear they need a prostate biopsy. Worries about pain, risks, or what the results might show are natural. Addressing these concerns openly helps patients feel prepared and supported through the process.
Questions men often ask in my practice
The most common question I hear is, “Will it hurt?” I explain that local anesthesia blocks most of the pain. Men usually feel pressure from the ultrasound probe or a brief pinch when the needle takes a sample, but not sharp pain. Knowing what sensations to expect often reduces fear.
Another frequent question is, “What happens if cancer is found?” I tell patients that not all prostate cancers are aggressive. Some grow so slowly that we only monitor them, while others need active treatment. This reassurance helps men understand that a cancer diagnosis does not always mean surgery or radiation right away. In my practice, I encourage patients to ask every question on their mind — no concern is too small when it comes to their health.
Emotional preparation before the test
Anxiety often feels stronger than the biopsy itself. I see many men who imagine the procedure will be far worse than it actually is. I advise patients to prepare by learning what will happen step by step, because clear information removes fear of the unknown. Simple techniques such as deep breathing, guided meditation, or even listening to calm music on the way to the clinic can ease tension.
Support from family or friends also makes a difference. Bringing a trusted person to the appointment, even just to sit in the waiting room, helps men feel less alone. In my practice, I remind patients that feeling nervous is normal, and asking for support shows strength, not weakness. Preparing emotionally is just as important as preparing physically.
How to talk with your doctor about biopsy options
Good communication with the urologist builds trust and ensures the patient makes informed decisions. I encourage men to ask about the different biopsy methods — transrectal, transperineal, and MRI-guided — and the risks and benefits of each. Doctors can then explain which option fits the patient’s health, history, and local resources.
It also helps to discuss what will happen after the test. Patients should ask how long results will take, what side effects to expect, and what follow-up care includes. In my practice, I remind men that no question is “silly” when it comes to their health. Clear dialogue with the doctor reduces uncertainty and helps each patient feel in control of his care.
FAQ About Prostate Biopsy (2025 Update)
When to See a Doctor
Prostate symptoms often cause worry, but not every man needs an immediate biopsy. Knowing when to seek medical advice ensures that problems are caught early without unnecessary stress.
Signs such as difficulty urinating, blood in urine or semen, persistent pelvic pain, or a rising PSA level should not be ignored. Schedule a consultation with your doctor to determine whether a prostate biopsy is the right next step for you.
“As a physician, I understand how stressful it can feel to hear you may need a prostate biopsy. While most prostate changes turn out harmless, some require timely attention. My advice is simple: do not ignore symptoms or rising PSA levels. If you notice persistent changes, seek medical guidance promptly. Early evaluation not only protects your health but also brings peace of mind.”
Board-Certified Urologist