Early Signs of Ovarian Cancer: What American Women Shouldn’t Ignore
Many women notice bloating, pelvic discomfort, or changes in appetite and assume these issues are related to diet, hormones, or everyday stress. The difficulty with ovarian cancer is that its earliest signs often resemble common, non-serious conditions. Because of this, many women delay seeking care until the disease has progressed. Understanding which symptoms deserve closer attention — and knowing when to see a doctor — can make all the difference in catching ovarian cancer early, when treatment is most effective.

Why early detection of ovarian cancer is so important
Early detection can mean the difference between a highly treatable condition and one that is discovered too late. Ovarian cancer is often called a “silent disease” because its early warning signs blend in with everyday complaints like bloating, fatigue, or changes in appetite. Recognizing these signals early and seeking timely medical care can significantly improve survival rates and quality of life.
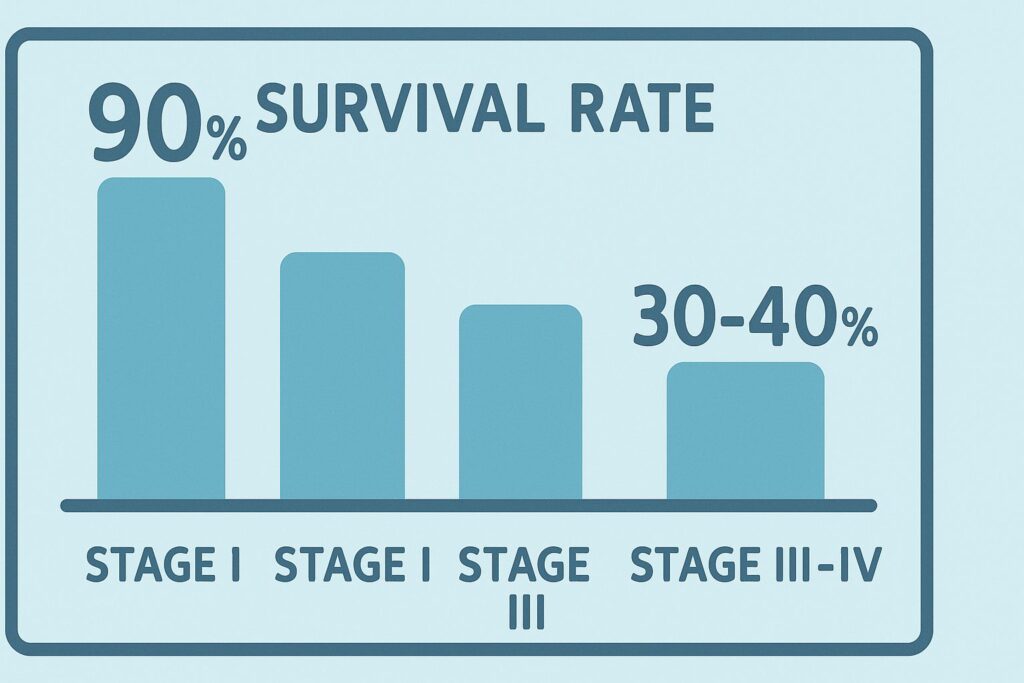
Survival rates by stage — why timing matters
Doctors measure progress in ovarian cancer using stages, from I to IV. Stage I means the tumor is limited to one or both ovaries, while stage IV indicates that the cancer has spread to distant organs. When diagnosed early, treatment is far more effective. Women with stage I ovarian cancer have a five-year survival rate of around 90%, meaning most live long, healthy lives after treatment.
Unfortunately, fewer than 20% of cases are diagnosed at this early stage. By the time symptoms become more obvious and the disease is discovered at stage III or IV, the survival rate drops sharply — often to 30–40%. These numbers underline a harsh truth: it is not the aggressiveness of ovarian cancer alone that makes it so dangerous, but how late it is usually found.
In clinical practice, I’ve seen how this plays out. Patients who insisted on a check-up after weeks of persistent bloating or pain often received life-saving early diagnoses. Those who waited months, hoping their discomfort would resolve, sometimes faced much more advanced disease. The earlier ovarian cancer is detected, the more treatment options are available — including surgery and targeted therapies that are less effective in late stages.
Why symptoms are often missed or misdiagnosed
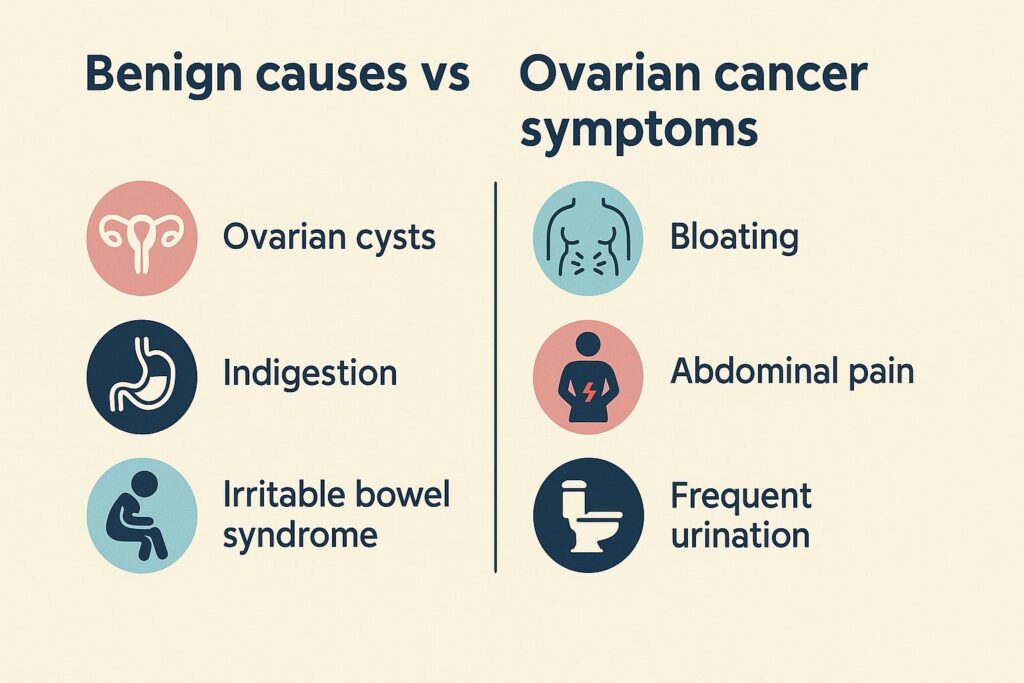
The earliest warning signs of ovarian cancer — bloating, pelvic pain, frequent urination, or loss of appetite — are subtle and often overlap with common, benign conditions. For example, irritable bowel syndrome can cause abdominal swelling, urinary tract infections can trigger urinary urgency, and hormonal changes can alter menstrual cycles. Because these problems are so widespread, women may not suspect anything serious, and doctors may first treat the more common explanation.

Another challenge is the intermittent nature of the symptoms. A woman might feel fine for several days, then notice bloating again after certain meals or during stressful periods. This on-and-off pattern can give a false sense of reassurance, delaying medical evaluation. Unlike acute conditions, ovarian cancer tends to cause vague but persistent discomfort, which slowly increases over time.
In my own practice, I often remind patients to pay attention to patterns. Occasional bloating after a heavy dinner is normal, but daily swelling that lasts for weeks is not. Similarly, needing to urinate once more than usual isn’t concerning, but waking up multiple times every night without a clear reason deserves attention. Misdiagnosis happens because these symptoms are so ordinary — yet persistence and progression are the red flags that set ovarian cancer apart.
What are the earliest symptoms of ovarian cancer?
Ovarian cancer rarely produces sudden or dramatic changes in the beginning. Instead, its earliest signs tend to be subtle and easily mistaken for routine digestive or musculoskeletal issues. Among the most common early indicators are persistent bloating, abdominal swelling, and ongoing pelvic or lower back pain. Paying attention to these symptoms — especially when they last for weeks rather than days — can help women seek medical care sooner.
Persistent bloating and abdominal swelling
Bloating that does not resolve with dietary changes or over-the-counter remedies is one of the hallmark early warning signs of ovarian cancer. Unlike normal gas or indigestion, this swelling tends to be constant and can cause clothes to feel tighter around the waistline. Some women also describe a sense of fullness or heaviness in the lower abdomen, even when they haven’t eaten much.
What makes this symptom concerning is its persistence. In clinical practice, I’ve seen patients who tried cutting out certain foods or adjusting their diet with no improvement. If abdominal swelling continues for more than two weeks and is not linked to obvious causes like large meals, constipation, or menstrual cycle changes, it deserves evaluation by a gynecologist.
Pelvic or lower back pain
Pain in the pelvic area or lower back can occur for many reasons, from muscle strain to menstrual cramps. However, when the discomfort is dull, persistent, and not tied to physical activity or the menstrual cycle, it may be an early sign of ovarian cancer. Unlike sharp pain that comes and goes, this type of ache often lingers and gradually becomes more noticeable over time.
In my medical experience, patients sometimes describe it as a deep pressure or dragging sensation in the pelvis or lower spine. While back pain is extremely common, the key red flag is persistence without clear explanation. If rest, stretching, or pain relievers don’t help, and the pain continues daily for weeks, it’s important not to dismiss it as “normal.” Early reporting of these symptoms allows doctors to rule out serious conditions and, if necessary, begin timely investigations for ovarian cancer.
Feeling full quickly and loss of appetite
Early satiety — the sensation of getting full after only a few bites — can appear when ovarian tumors or fluid buildup press against the stomach. This is not the same as skipping a meal or losing appetite during stress; it tends to happen repeatedly, with almost every meal.
Patients often notice they cannot finish their usual portions or that food becomes less appealing altogether. When this change persists for weeks and leads to gradual weight loss, it should be treated as a potential warning sign of ovarian cancer.
Frequent urination or urgent need to urinate
A common but overlooked symptom is the need to urinate more often than usual, sometimes with a sense of urgency. Unlike bladder infections, this usually occurs without burning, pain, or fever. The pressure comes from the ovaries or surrounding tissues pressing against the bladder.
If urinary frequency continues day and night for weeks and tests show no infection, it is important to consider ovarian cancer among the possible causes. Persistent bladder pressure without a clear explanation should never be ignored.
Menstrual changes or postmenopausal bleeding
Irregular cycles, heavier-than-usual periods, or spotting after menopause may indicate a gynecologic problem that deserves attention. While hormonal fluctuations or benign conditions can cause similar changes, ovarian cancer should be ruled out if symptoms repeat or worsen.
Doctors emphasize that any bleeding after menopause is abnormal and should prompt an immediate evaluation. Even in younger women, unexplained cycle changes that persist need investigation through ultrasound and blood tests.
Unexplained fatigue and weight loss
Constant tiredness and unintended weight loss are among the less specific but concerning early signs of ovarian cancer. They occur because cancer can alter metabolism, reduce appetite, and place strain on the body’s energy systems.
Unlike normal fatigue that improves with rest, this exhaustion lingers and often worsens. Women may notice looser clothing despite no dieting, or that everyday tasks feel harder. When combined with other early symptoms, these changes raise strong concern for ovarian cancer.
How do early ovarian cancer symptoms differ from common conditions?
One of the greatest challenges in detecting ovarian cancer early is that its symptoms overlap with many benign conditions. Women often assume their discomfort is related to digestion, hormones, or common gynecologic problems. Understanding the differences can help identify when ordinary issues become potential warning signs.
Ovarian cysts vs ovarian cancer symptoms
Ovarian cysts are fluid-filled sacs that commonly form during ovulation and usually resolve on their own. They can cause pelvic pain, bloating, or pressure, but these symptoms often fluctuate with the menstrual cycle and improve over time. Most cysts are benign and temporary.
By contrast, ovarian cancer symptoms tend to be persistent and progressive. Instead of pain that comes and goes, the discomfort lingers for weeks and may gradually worsen. While cysts may be identified during routine ultrasound and monitored, persistent bloating, pelvic pain, or unexplained appetite loss should raise suspicion for something more serious.
IBS, indigestion, or gas vs persistent bloating
Irritable bowel syndrome and simple indigestion are among the most common causes of abdominal discomfort. Symptoms may include bloating, cramping, and changes in bowel habits, but they typically improve with dietary adjustments, stress management, or medications. Gas-related bloating often resolves within hours or days.
Ovarian cancer–related bloating is different: it is consistent, does not improve with food changes, and often coexists with feelings of heaviness or abdominal swelling. Women may notice that clothes fit tighter even when weight has not increased. The key distinction is persistence — if bloating continues daily for more than two weeks, especially when paired with pelvic pain or urinary changes, it should not be dismissed as “just IBS.”
Menstrual irregularities vs cancer warning signs
Menstrual irregularities are common in adolescence, perimenopause, and times of stress. Hormonal imbalances, thyroid disorders, or benign gynecologic conditions can cause heavy bleeding, skipped cycles, or spotting. These patterns often change over months and may stabilize without treatment.
Ovarian cancer warning signs differ because abnormal bleeding often appears unexpectedly, worsens, or occurs after menopause when periods should no longer happen. Any postmenopausal bleeding is considered abnormal and warrants immediate evaluation. In younger women, cycle changes that remain unpredictable despite treatment also need careful assessment to rule out underlying cancer.
| Symptom | Common benign causes | Possible ovarian cancer warning |
|---|---|---|
| Persistent bloating / abdominal swelling | Indigestion, IBS, gas, constipation | Daily bloating lasting >2 weeks, not relieved by diet changes |
| Pelvic or lower back pain | Muscle strain, menstrual cramps, endometriosis | Dull, ongoing pain not linked to activity or cycle |
| Feeling full quickly / loss of appetite | Stress, stomach infection, reflux | Early satiety at nearly every meal, associated with weight loss |
| Frequent urination / urgency | Urinary tract infection, high fluid intake, overactive bladder | Persistent urgency without burning, fever, or infection |
| Menstrual changes or postmenopausal bleeding | Hormonal imbalance, thyroid disorders, perimenopause | Unexplained irregular cycles, any bleeding after menopause |
| Unexplained fatigue and weight loss | Stress, depression, thyroid disease | Constant tiredness with unintended weight loss, worsening over time |
When should you see a doctor about ovarian symptoms?
Because ovarian cancer symptoms often resemble everyday issues, many women hesitate to make an appointment. Yet timing is critical: the sooner you act, the better the chances for early detection. Knowing which changes count as red flags — and how long they should persist — can guide you in deciding when to see a gynecologist.
Red flag symptoms you should never ignore
Some symptoms require prompt medical attention regardless of age or background. These include persistent bloating or abdominal swelling that lasts more than two weeks, pelvic or lower back pain that does not improve with rest, unexplained weight loss, and any bleeding after menopause. Frequent urination without signs of infection also belongs to this list.
In my practice, I remind patients that while occasional discomfort is common, symptoms that keep recurring or intensifying are not. Ignoring them can delay diagnosis and reduce treatment options. If you notice two or more of these red flags together, it is especially important to schedule a medical evaluation.
How long symptoms should persist before seeking care
Temporary issues like indigestion, stress-related fatigue, or a single irregular period are rarely cause for alarm. The difference with ovarian cancer is persistence. If symptoms such as bloating, urinary urgency, or appetite loss continue daily for more than two weeks, you should not wait longer.
Doctors generally advise that any symptom lasting over 14 days without clear cause deserves evaluation. Women with a family history of ovarian or breast cancer should be even more proactive, as genetic risks make early attention more important.
What to expect during a gynecologic exam
Many women worry about what will happen at the doctor’s office, but the initial steps are straightforward. A gynecologist will begin with a detailed discussion of your symptoms and medical history, followed by a pelvic exam to feel for abnormalities.
Depending on the findings, the doctor may order a transvaginal ultrasound or blood tests such as CA-125. These tests do not confirm cancer on their own but provide valuable clues. If something suspicious is seen, further evaluation may include referral to a specialist or, in some cases, minor surgery for biopsy. Knowing what to expect often helps reduce anxiety and encourages women to seek care sooner.
How is ovarian cancer diagnosed in the US?
Because early ovarian cancer symptoms are vague, doctors rely on a combination of clinical exams and diagnostic tests to identify the disease. No single test can confirm ovarian cancer on its own, which is why evaluation often involves several steps.
Transvaginal ultrasound and pelvic exam
The first step usually includes a pelvic exam, where the gynecologist checks for abnormalities in the ovaries, uterus, and surrounding tissues. While this exam may not detect small tumors, it helps identify unusual swelling or tenderness.
A transvaginal ultrasound is often the next step. This imaging test uses sound waves to create detailed pictures of the ovaries and pelvis. It can reveal masses, cysts, or fluid buildup. However, ultrasound alone cannot determine whether a mass is cancerous or benign, so results are always interpreted alongside clinical history and other tests.
CA-125 blood test — limitations and role
CA-125 is a protein that can be elevated in women with ovarian cancer. A blood test measuring its levels is commonly used as part of the diagnostic process. However, CA-125 is not a definitive tool: levels may also rise due to benign conditions such as endometriosis, fibroids, or even normal menstruation.
Doctors use the CA-125 test more effectively in women who already have suspicious findings on ultrasound or a strong family history of ovarian cancer. In those cases, a high CA-125 level may increase concern and prompt further investigation. In monitoring women who have already been treated, the test is useful for tracking recurrence, but it is not reliable as a routine screening tool for the general population.
Genetic testing (BRCA1, BRCA2, family history)
Genetic testing plays an important role in identifying women at higher risk for ovarian cancer. Mutations in the BRCA1 and BRCA2 genes, as well as certain other inherited genetic syndromes, significantly increase lifetime risk. Women with a strong family history of ovarian or breast cancer are often referred for genetic counseling to decide whether testing is appropriate.
A simple blood or saliva test can detect these mutations. If a gene mutation is found, doctors may recommend closer monitoring, preventive strategies, or even risk-reducing surgery in some cases. For women without symptoms but with family risk, genetic testing provides valuable information that can guide future healthcare decisions.
When biopsy or surgery may be necessary
Unlike some cancers, ovarian cancer cannot usually be confirmed by a simple needle biopsy. If imaging tests or blood results strongly suggest malignancy, doctors may recommend surgery both to remove the mass and to obtain tissue for analysis.
During this procedure, a gynecologic oncologist examines the ovaries and surrounding tissues, removes suspicious areas, and sends samples to a pathologist. Only microscopic evaluation can confirm whether a growth is cancerous. Although surgery may sound intimidating, it provides the most accurate diagnosis and also serves as the first step in treatment if cancer is found.
Can lifestyle or screening help with early detection?
Unlike some cancers, ovarian cancer does not yet have a simple screening test that reliably detects the disease in its earliest stages. Still, awareness of family history, appropriate genetic counseling, and healthy lifestyle choices can all play a role in reducing risk and encouraging timely evaluation.

Is there a reliable screening test for ovarian cancer?
Currently, there is no standard screening test proven to catch ovarian cancer early in the general population. Pap smears, which many women receive regularly, do not detect ovarian cancer. Tests such as transvaginal ultrasound and the CA-125 blood test are useful in women with suspicious symptoms or high genetic risk, but they are not accurate enough to screen all women.
Researchers are actively studying new biomarkers and imaging strategies, but for now, the most effective approach is paying attention to persistent symptoms and seeking care quickly. This is why awareness remains the best defense until better screening tools become widely available.
The role of family history and genetic counseling
Family history is one of the strongest predictors of ovarian cancer risk. Women with close relatives — especially a mother, sister, or daughter — who have had ovarian or breast cancer should share this information with their doctor.
Genetic counseling helps women understand whether testing for BRCA1, BRCA2, or other gene mutations is appropriate. Counselors also discuss preventive strategies, which may include earlier screenings or, for high-risk women, preventive surgery. Understanding personal and family risk empowers women to make informed choices about their health.
Lifestyle factors (diet, exercise, hormonal health)
While lifestyle alone cannot prevent ovarian cancer, healthy habits contribute to lower overall risk and better resilience. Regular physical activity, a diet rich in fruits, vegetables, and whole grains, and maintaining a healthy weight all support hormonal balance and reduce inflammation.
Some studies suggest that long-term use of birth control pills may lower ovarian cancer risk by reducing the number of ovulations. Likewise, avoiding smoking and managing chronic conditions such as diabetes and obesity contribute to better gynecologic health overall. Though these steps cannot guarantee prevention, they form part of a proactive approach to reducing risk.
FAQs about Early Signs of Ovarian Cancer
Expert’s Closing Note
Sources / References
- American Cancer Society — Ovarian Cancer: Overview & Symptoms
- Mayo Clinic — Ovarian Cancer: Symptoms and Causes
- National Cancer Institute — Ovarian Cancer (PDQ®) — Patient Version
- Centers for Disease Control and Prevention (CDC) — Ovarian Cancer
- NHS — Ovarian Cysts & Ovarian Cancer (information for patients)