Vomiting Blood in Stomach Cancer
Vomiting Blood in Stomach Cancer: Causes, Urgency, and Medical Respons
- Why Vomiting Blood Happens in Stomach Cancer Patients
- How Bleeding Starts: The Pathophysiological Link
- How Common Is Vomiting Blood in People with Stomach Cancer?
- What Can Trigger Vomiting Blood in These Patients?
- When to Seek Emergency Medical Help
- How Doctors Diagnose Bleeding in Stomach Cancer
- How Vomiting Blood Is Treated in Stomach Cancer Patients
- Can This Life-Threatening Symptom Be Prevented?
- Does Vomiting Blood Resolve After Treatment?
- What Oncologists and Gastroenterologists Say
- Questions to Ask Your Doctor
- 15+ FAQ: Vomiting Blood in Stomach Cancer
Why Vomiting Blood Happens in Stomach Cancer Patients
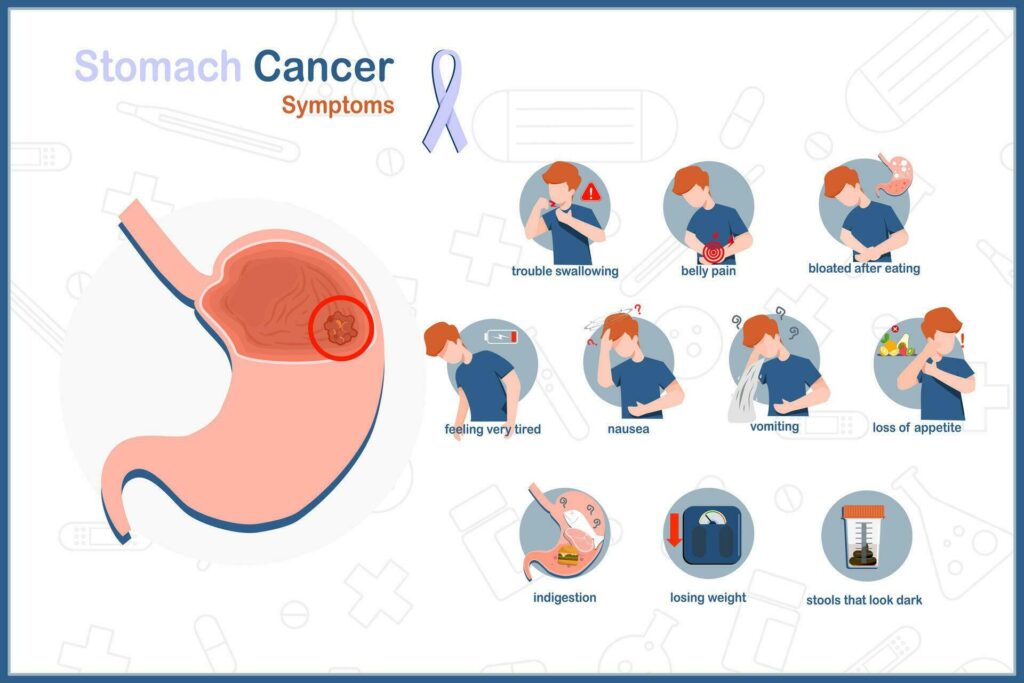
Vomiting blood—medically known as hematemesis—is one of the most alarming symptoms associated with stomach cancer. It often reflects active bleeding in the upper gastrointestinal tract, particularly from ulcerated tumors or damaged stomach vessels.
In the context of stomach cancer, vomiting blood can occur due to tumor erosion into blood vessels, necrosis of cancerous tissue, or pressure on nearby structures. Patients may notice dark red or coffee-ground colored vomit, sometimes accompanied by dizziness, fatigue, or shock.
This symptom is not always sudden. In many cases, patients experience subtle signs first—such as worsening abdominal discomfort, nausea, black stools, or frequent stomach noises from slowed digestion and blood pooling in the gut.
Recognizing vomiting blood as a potential complication of stomach malignancy is vital, as it typically signals advanced disease or a high-risk emergency.
How Bleeding Starts: The Pathophysiological Link
Stomach cancer, particularly adenocarcinoma, grows within the lining of the stomach and may ulcerate as it enlarges. As the tumor invades deeper layers, including the muscularis and submucosa, it may erode arteries or capillaries, resulting in internal bleeding.
In some cases, chemotherapeutic agents, radiation, or NSAIDs used during cancer treatment can weaken mucosal defenses, accelerating erosion. Tumors may also produce fragile blood vessels (neovascularization), which bleed easily under mechanical or digestive stress.
Common Mechanisms of Hematemesis in Stomach Cancer
| Mechanism | How It Leads to Vomiting Blood |
| Tumor ulceration | Exposes blood vessels to stomach acid and injury |
| Direct vessel invasion | Causes arterial or venous bleeding |
| Necrosis of tumor tissue | Leads to rupture and hemorrhage |
| Post-treatment mucosal damage | Weakens stomach lining, leading to bleeding |
| Pressure from tumor mass | Stretches and tears surrounding tissue |
When stomach wall metastasis occurs, the risk of bleeding may increase further, especially if the tumor spreads to vascular-rich layers or nearby organs like the pancreas or liver.
How Common Is Vomiting Blood in People with Stomach Cancer?
Vomiting blood is not always present in early stomach cancer, but it becomes more likely as the tumor progresses. It is more prevalent in patients with advanced, ulcerating, or poorly differentiated tumors. It’s also more frequent in those undergoing aggressive therapy or with co-existing gastrointestinal conditions like gastritis or varices.
Clinical Observations by Tumor Stage
| Stage of Stomach Cancer | Likelihood of Vomiting Blood |
| Early-stage, superficial tumors | Rare (~5–10%) |
| Locally advanced ulcerated tumors | Moderate (~20–40%) |
| Advanced stage with vessel invasion | High (~60–75%) |
| Recurrent or metastatic disease | Up to 80% in high-risk patients |
Retrospective studies show that hematemesis in stomach cancer is often a presenting symptom in resource-limited settings, where diagnosis is delayed. In developed countries, it typically occurs during progression or recurrence, often prompting emergency endoscopy.
What Can Trigger Vomiting Blood in These Patients?
Multiple triggers—both direct and indirect—can precipitate hematemesis in stomach cancer. Understanding these helps guide both prevention and emergency response.
Factors That Precipitate GI Bleeding
| Type of Trigger | Examples and Effects |
| Tumor-Related | Tumor erosion, growth into vessels, mechanical trauma from food |
| Treatment-Induced | Radiation, chemotherapy, corticosteroid-induced ulcers |
| Medication-Related | NSAIDs, anticoagulants, targeted therapies |
| Infection/Inflammation | H. pylori or secondary gastritis causing mucosal fragility |
| Mechanical Stress | Vomiting, retching, or gastric distension increasing pressure on tumor tissue |
Vomiting blood may also occur unexpectedly, especially in patients who were previously stable. This makes regular monitoring, especially in patients with symptoms like persistent nausea, anemia, or visible stomach noises, an essential part of care.
When to Seek Emergency Medical Help
Vomiting blood in the context of stomach cancer is always a red flag, but some cases require immediate hospitalization. Severe hematemesis can lead to hypovolemic shock, a life-threatening condition where blood loss results in dangerously low blood pressure and organ failure.
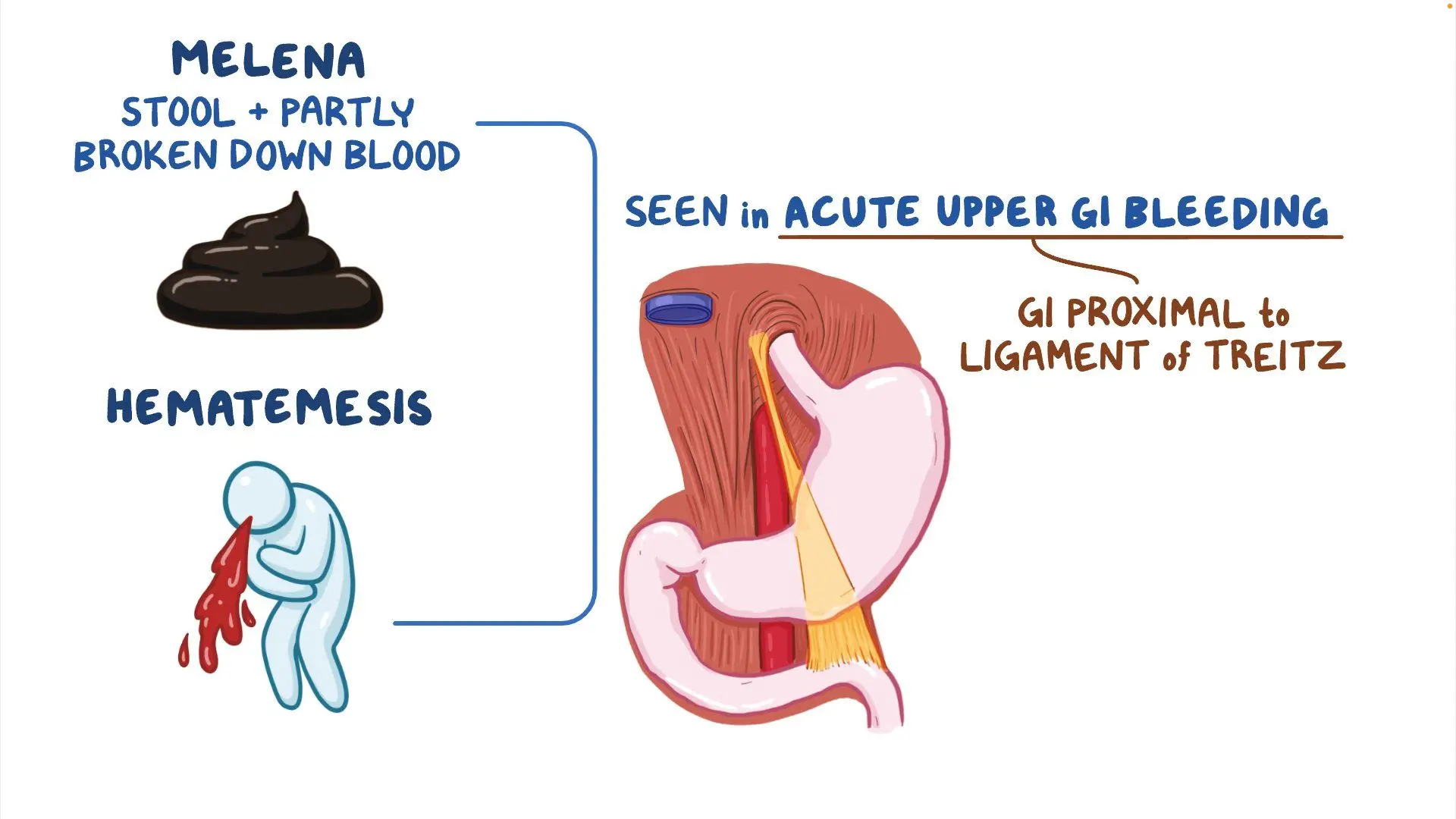
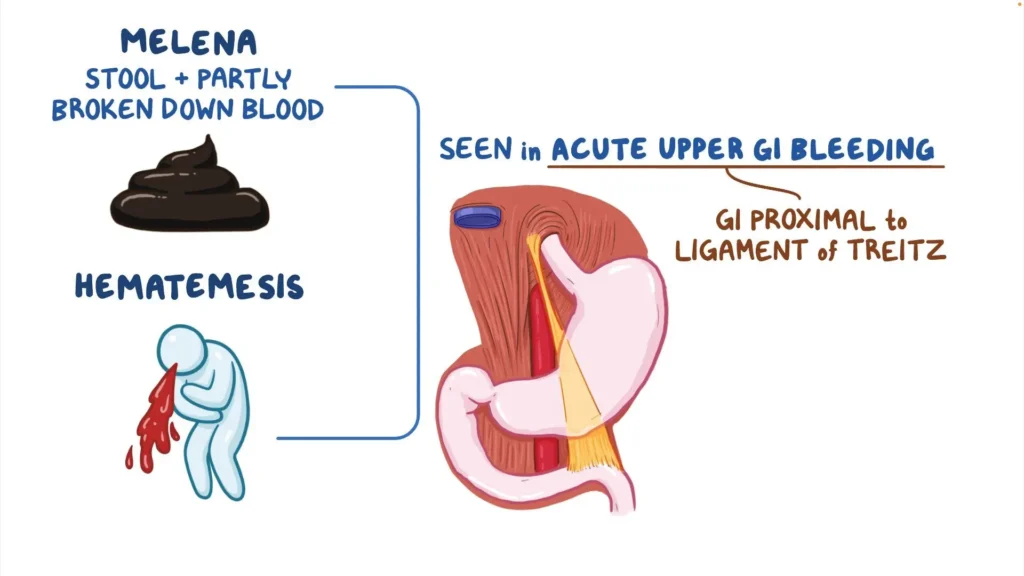
Key warning signs include vomiting large volumes of bright red blood, signs of shock (cold extremities, low pulse, confusion), chest pain, or black tarry stools (melena), which indicate prolonged internal bleeding. Patients already known to have gastric tumors are especially vulnerable if they’re undergoing treatment that weakens the stomach lining.
It’s critical for caregivers and patients to recognize the difference between manageable bleeding and acute hemorrhage, especially if recurrent vomiting or gastrointestinal pain was present beforehand.
Emergency Symptoms and Clinical Interpretation
| Symptom or Sign | Clinical Concern |
| Vomiting bright red blood | Active upper GI hemorrhage |
| Coffee-ground emesis | Slow gastric bleeding (oxidized blood) |
| Pale, clammy skin + fast heartbeat | Hypovolemia or shock |
| Sudden collapse after vomiting | Severe intragastric bleeding |
| Black tarry stools (melena) | Ongoing upper GI blood loss |
Immediate evaluation in an emergency department is warranted if any of the above signs occur, especially in combination.
How Doctors Diagnose Bleeding in Stomach Cancer
Once vomiting blood is reported, the first priority is to stabilize the patient, followed by pinpointing the source of bleeding. A combination of clinical examination, blood tests, and endoscopic imaging helps confirm the diagnosis and plan treatment.
Diagnostic Methods for Hematemesis in Stomach Cancer
| Diagnostic Tool | Purpose |
| Upper GI Endoscopy (EGD) | Direct visualization of bleeding site, tumor extent |
| CBC + Coagulation Profile | Assesses anemia, platelet count, and clotting status |
| Contrast-Enhanced CT Scan | Evaluates tumor invasion, vessel rupture, or metastasis |
| Crossmatch and Type | Prepares for possible blood transfusion |
| Gastric Biopsy (if safe) | Determines histology and ulceration if bleeding is controlled |
| Nasogastric Tube Aspiration | Confirms presence of blood in stomach (when endoscopy is delayed) |
Endoscopy is typically the gold standard for diagnosing upper GI bleeding and offers therapeutic options, such as cauterization or injection therapy, at the same time. If a tumor is bleeding and obscures the field, CT or angiography may be used to assess for stomach wall metastasis or arterial bleeding.
How Vomiting Blood Is Treated in Stomach Cancer Patients
Treatment strategies are focused on stabilizing the patient, stopping the bleeding, and addressing the underlying cancer. Depending on the severity, interventions may be endoscopic, pharmacologic, or surgical.
Clinical Approaches to Managing Hematemesis
| Intervention Type | Example/Use Case |
| Fluid Resuscitation + Blood Transfusion | Replaces lost volume and hemoglobin |
| Proton Pump Inhibitors (IV) | Reduces gastric acidity to protect bleeding sites |
| Endoscopic Hemostasis | Thermal coagulation, clip placement, or injection therapy |
| Embolization (Interventional Radiology) | Occludes bleeding vessels when endoscopy fails |
| Emergency Surgery | Used for uncontrolled hemorrhage or tumor resection |
| Oncologic Therapy | Chemotherapy or radiation to shrink bleeding tumors |
Supportive care may also include oxygen therapy, NPO (nothing by mouth) status, and correction of coagulopathies. In terminal cases where bleeding is recurrent and treatment-resistant, palliative options and comfort-focused care may be discussed.
Can This Life-Threatening Symptom Be Prevented?

While hematemesis cannot always be prevented in stomach cancer, certain strategies can lower risk and prepare for rapid response. Preventive care focuses on reducing mucosal injury, identifying high-risk lesions early, and managing contributing factors such as drug toxicity or infection.
Preventive Measures in At-Risk Patients
| Strategy | Preventive Effect |
| Regular endoscopic surveillance | Detects ulcerated or bleeding-prone tumors early |
| Avoiding NSAIDs and anticoagulants | Reduces gastric mucosal risk and bleeding tendency |
| Helicobacter pylori eradication | Lowers inflammation and mucosal damage |
| Controlled use of steroids | Minimizes therapy-induced ulcers |
| Nutritional and hydration support | Supports mucosal repair and barrier function |
Patients with signs like weight loss, black stools, persistent indigestion, or audible stomach noises after eating should be evaluated promptly. Identifying pre-bleeding warning signs offers the best chance of proactive treatment before hematemesis occurs.
Does Vomiting Blood Resolve After Treatment?
Whether vomiting blood stops after treatment depends on the stage of the tumor, the bleeding site, and the treatment modality used. In many cases, especially when the bleeding is caused by localized ulceration, endoscopic interventions or tumor-targeted therapies can lead to full resolution of hematemesis.
Patients who undergo successful tumor resection or receive effective chemotherapy often experience a rapid decline in bleeding episodes. However, in advanced or metastatic cases—particularly those with vascular invasion or stomach wall metastasis—bleeding may recur despite treatment, sometimes requiring repeated procedures or palliative support.
In cases where vomiting blood is the result of treatment toxicity or mucosal damage, dose adjustments and mucosal protectants (e.g., proton pump inhibitors) often help control symptoms.
Likelihood of Hematemesis Resolution by Clinical Scenario
| Clinical Scenario | Likelihood of Resolution |
| Localized bleeding from ulcerated tumor | High with endoscopic/surgical treatment |
| Bleeding from metastatic lesion or necrosis | Moderate to low; often recurrent |
| Bleeding triggered by medication toxicity | Good with cessation and protective therapy |
| Ongoing bleeding despite therapy | Palliative focus likely |
Regular monitoring and follow-up endoscopy are essential to assess healing and the risk of rebleeding.
What Oncologists and Gastroenterologists Say
Specialists in gastrointestinal oncology and endoscopy agree that vomiting blood in stomach cancer is an urgent and manageable complication—but only with rapid diagnosis and interdisciplinary care.
Gastroenterologists emphasize early endoscopy for both diagnosis and immediate treatment of active bleeding. They also recommend avoiding medications like NSAIDs and certain anticoagulants unless absolutely necessary.
Oncologists advise that patients with bleeding tumors are at higher risk of treatment interruptions and may need individualized regimens that balance bleeding risk with cancer control. They often collaborate with radiologists to use embolization techniques when endoscopic treatment fails or isn’t feasible.
Both agree that coordinated care—especially in advanced cancer—is essential. In cases where curative treatment is not possible, the focus shifts to reducing distress, improving quality of life, and preparing families for potential complications.
Many also recommend educating patients and caregivers to recognize early signs of gastrointestinal bleeding, particularly if the patient has prior bleeding episodes, persistent stomach noises, or weight loss.
Questions to Ask Your Doctor
To manage the risks and treatment of vomiting blood in stomach cancer, it’s helpful to bring prepared questions to your medical team. These questions improve decision-making and reduce the stress of unexpected complications.
| Suggested Question | Why It’s Important |
| What caused the bleeding in my case? | Clarifies mechanism (tumor vs. treatment) |
| Is this a life-threatening episode? | Assesses urgency and level of risk |
| What treatment will stop the bleeding now? | Outlines immediate medical plan |
| Will this bleeding happen again? | Sets realistic expectations |
| Can this tumor be removed or treated to prevent bleeding? | Explores curative or control options |
| Should I change my medications or diet? | Reduces aggravating factors |
| Can I still receive chemotherapy? | Evaluates balance between cancer therapy and safety |
| How will you monitor me after this event? | Defines follow-up protocol |
| What warning signs should I watch for? | Empowers early detection of rebleeding |
| Will I need a transfusion or hospitalization? | Plans for future events |
| Are there preventive treatments for future episodes? | Considers long-term control |
| Is surgery or embolization an option? | Explores procedural interventions |
| How does this bleeding affect my prognosis? | Places symptoms in clinical context |
| Should I consult a palliative care team? | Supports planning and comfort if needed |
| What should caregivers do if this happens at home? | Guides emergency preparation |
15+ FAQ: Vomiting Blood in Stomach Cancer
1. Is vomiting blood always caused by cancer itself?
No. It can result from tumor ulceration, treatment side effects, or unrelated gastric conditions. However, in stomach cancer patients, it is often tumor-related.
2. What does it mean if the vomit looks like coffee grounds?
This typically indicates older or slower bleeding. Blood has been in the stomach long enough to be partially digested.
3. How much blood is considered dangerous?
Any amount can be serious, but vomiting large volumes or experiencing associated symptoms (like dizziness or fainting) is an emergency.
4. Will vomiting blood stop on its own?
Occasionally, but bleeding in stomach cancer often recurs and should always be evaluated and treated.
5. Can I continue chemotherapy after vomiting blood?
It depends on the cause and severity. Your doctor may pause or adjust treatment until bleeding is controlled.
6. Does vomiting blood mean the cancer has worsened?
Not always, but it can suggest tumor progression, especially if the bleeding is new or recurrent.
7. What are the treatment options if endoscopy doesn’t stop the bleeding?
Angiographic embolization or surgery may be used. In terminal cases, palliative care focuses on comfort.
8. Should I go to the ER every time I vomit blood?
Yes. All cases of hematemesis in stomach cancer warrant emergency evaluation.
9. Can acid-blocking medications help?
Yes. PPIs reduce stomach acid and protect ulcerated tissue, aiding clot formation.
10. What can I eat after a bleeding episode?
Only as advised by your doctor. Initially, patients may be NPO (nothing by mouth) to allow healing.
11. Can bleeding be predicted or prevented?
Sometimes. Regular monitoring, avoiding irritants, and addressing early warning signs help.
12. Is vomiting blood painful?
The vomiting itself may not be painful, but associated conditions like ulcers or cancer pain can cause discomfort.
13. Does vomiting blood shorten life expectancy?
It may in advanced cancer, particularly if bleeding is recurrent or uncontrolled, but not always.
14. Can younger patients with stomach cancer have this symptom?
Yes, especially with ulcerating tumors or aggressive forms of cancer.
15. How do doctors know where the bleeding is coming from?
Through endoscopy, imaging, and clinical history. These tools help pinpoint and treat the bleeding source.