Difficulty Swallowing in Esophageal Cancer
Difficulty Swallowing in Esophageal Cancer: Causes, Diagnosis, and Relief
- Why Difficulty Swallowing Happens in Esophageal Cancer
- How Tumors and Treatments Affect Swallowing Function
- How Common Is This Symptom in Esophageal Cancer?
- Clinical Trends and Stage-Linked Severity
- Underlying Causes Behind Swallowing Difficulty in Cancer Patients
- When to Be Concerned: Red Flags in Dysphagia
- Diagnostic Techniques to Identify the Problem
- Therapeutic Options and Symptom Management
- Preventing Swallowing Problems During Cancer Care
- Does It Go Away? Recovery and Prognosis
- What Doctors Emphasize to Patients
- 15+ Questions to Discuss with Your Doctor (FAQ)
Why Difficulty Swallowing Happens in Esophageal Cancer

Dysphagia, or difficulty swallowing, is one of the hallmark symptoms of esophageal cancer. Patients often describe the sensation as food getting “stuck” behind the breastbone, or a growing discomfort when trying to eat solid foods. This symptom typically begins subtly and worsens progressively, often becoming one of the reasons patients seek medical attention.
The sensation is more than a mechanical issue—it often causes anxiety, nutritional deficiencies, and social isolation during meals. For many, it signifies a deeper underlying pathology in the esophagus that requires immediate investigation and care.
How Tumors and Treatments Affect Swallowing Function
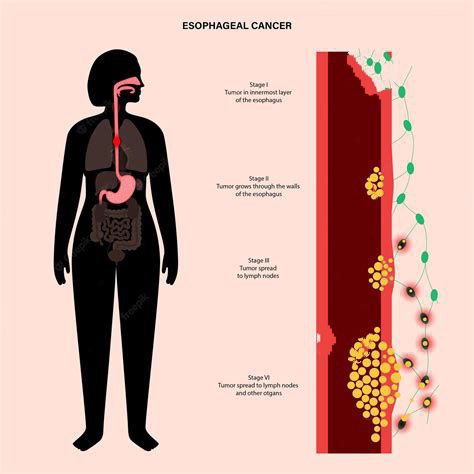
The main mechanism behind dysphagia in esophageal cancer lies in tumor growth. As malignant cells form within the lining of the esophagus, they may thicken and invade deeper tissues. Over time, this can constrict the esophageal passage and impede the natural flow of food from the mouth to the stomach.
In some cases, treatment itself—such as radiation therapy—can cause esophageal inflammation (esophagitis) or scarring, further complicating the swallowing process. Even chemotherapy, though systemic, may trigger mucosal changes that intensify the issue.
This interference can be visualized through barium swallow tests or endoscopy, where narrowing or tumor mass becomes evident.
How Common Is This Symptom in Esophageal Cancer?
Dysphagia is reported in over 70% of patients diagnosed with esophageal cancer at the time of presentation. In many cases, it is the first and most persistent symptom. Its presence often correlates with tumor size, location, and stage of disease progression.
Clinical observations reveal that lower third esophageal tumors tend to affect swallowing more rapidly, especially for solids. In early-stage cases, the symptom may be minimal or absent, but as the tumor grows, patients progressively move from trouble swallowing solids to even difficulty with liquids and saliva.
Severity is generally categorized using a clinical grading scale—from occasional discomfort to complete obstruction.
Clinical Trends and Stage-Linked Severity
| Stage of Esophageal Cancer | Prevalence of Dysphagia | Description |
| Stage I | Rare (~10%) | Often asymptomatic or mild discomfort |
| Stage II | Moderate (~40–50%) | Discomfort with solids begins |
| Stage III | High (~70–80%) | Solid and some liquid difficulty |
| Stage IV | Very High (>90%) | Severe dysphagia or complete blockage |
This direct relationship between disease stage and symptom severity helps guide diagnostic urgency and treatment intensity. Swallowing issues also strongly affect nutritional status, which is a key predictor of patient outcomes.
Underlying Causes Behind Swallowing Difficulty in Cancer Patients

The primary cause of dysphagia in esophageal cancer is tumor obstruction. As the malignant mass expands inward, it reduces the lumen of the esophagus, making it increasingly hard for food or liquids to pass. But several additional layers compound the problem.
Oncological factors include the exact location of the tumor, whether it’s squamous cell carcinoma (typically upper or mid-esophagus) or adenocarcinoma (often at the lower esophageal junction). Tumor invasion into surrounding nerves or the trachea can also disrupt the natural swallowing reflex.
Treatment-related causes such as radiation-induced strictures or chemotherapy-related mucositis can damage the epithelial lining and contribute to pain or discomfort when swallowing. Radiation fibrosis is a known long-term consequence, especially when high doses are delivered to localized regions of the thorax.
Metabolic and nutritional factors—patients with poor nutrition often develop esophageal muscle weakness, making the problem worse. Reflux disease, which is common in these patients, may also inflame the esophagus and cause additional symptoms.
Secondary infections, especially fungal or viral esophagitis (e.g., candida or herpes simplex), can also worsen swallowing in immunocompromised cancer patients.
When to Be Concerned: Red Flags in Dysphagia
While some swallowing difficulty is expected in esophageal cancer, certain warning signs signal urgent medical attention is needed. These include:
- Inability to swallow liquids
- Frequent choking or coughing during meals
- Weight loss exceeding 5% in a month
- Blood in saliva or regurgitated food
- Chest pain unrelated to eating
- Hoarseness or changes in voice
- Signs of aspiration pneumonia (fever, cough, shortness of breath)
Such symptoms may indicate rapid tumor progression, infection, or even tracheoesophageal fistula—a severe and potentially life-threatening complication.
Patients already diagnosed with cancer should inform their oncologist immediately if any of the above emerge or worsen. These changes may also suggest that the cancer has spread or that treatment is causing new structural issues.
Diagnostic Techniques to Identify the Problem
Diagnosing the cause and extent of dysphagia involves a combination of imaging, endoscopic, and sometimes histological tools.
| Diagnostic Tool | Purpose |
| Barium Swallow X-ray | Visualizes blockages, strictures, and delayed passage |
| Upper Endoscopy (EGD) | Direct view of the esophagus, allows biopsy |
| CT or PET Scans | Assesses tumor spread, lymph node involvement |
| Esophageal Manometry | Measures muscle function and coordination |
| pH Monitoring | Checks acid reflux contributing to inflammation |
Endoscopy remains the gold standard, not just for diagnosis, but also for staging, as it allows real-time visualization and tissue collection.
In some patients, especially those with complete obstruction, endoscopic ultrasound (EUS) may be attempted to assess the depth of invasion and guide treatment plans.
Therapeutic Options and Symptom Management
Relieving swallowing difficulty requires a combination of direct tumor treatment and symptomatic support. The overall strategy depends on the patient’s stage, health status, and treatment goals (curative vs palliative).
Medical approaches:
- Proton pump inhibitors (PPIs) to reduce inflammation if reflux is involved
- Topical anesthetics to reduce pain during swallowing
- Antifungals or antivirals in case of secondary infections
- Chemoradiotherapy to shrink the tumor and widen the esophageal opening
Procedural interventions:
- Esophageal stent placement for rapid palliation in advanced cases
- Balloon dilation for strictures, though this carries a risk of perforation
- Laser or photodynamic therapy to debulk tumors
- Surgical resection (esophagectomy) in operable cases
Nutritional support is essential—many patients require temporary feeding tubes (e.g., PEG tubes) to maintain weight and energy for ongoing treatment.
In complex cases, multidisciplinary care involving oncologists, gastroenterologists, nutritionists, and palliative specialists ensures comprehensive symptom relief and improved quality of life.
Preventing Swallowing Problems During Cancer Care
While dysphagia is often inevitable in esophageal cancer, several preventive strategies can reduce its severity or delay its onset. Prevention focuses on both tumor control and esophageal care during and after treatment.
Early-stage detection through screening in high-risk patients—particularly those with chronic GERD or Barrett’s esophagus—allows for earlier intervention, which is less likely to impair swallowing. Timely removal of precancerous lesions or treatment with radiofrequency ablation can prevent progression to obstruction.
For those undergoing radiation or chemoradiation, prophylactic use of mucosal protectants and careful dose planning can minimize damage to healthy tissue. Some centers also advocate for swallowing therapy before dysphagia develops—this “prehabilitation” can strengthen muscles and prepare patients for recovery.
Maintaining hydration, avoiding smoking and alcohol, and sticking to a soft diet during active treatment may prevent ulcerations or strictures. Patients should be closely monitored for early signs of candidiasis, reflux, or malnutrition, all of which can worsen esophageal function.
Finally, avoiding rapid weight loss and working with a dietitian can help maintain muscle tone and swallowing reflexes.
Does It Go Away? Recovery and Prognosis
Whether swallowing improves or not depends heavily on the stage of cancer, type of treatment, and overall prognosis.
| Clinical Scenario | Expected Course of Dysphagia |
| Early-stage, post-surgical patients | Often resolves completely after healing |
| Chemoradiation-treated patients | May improve gradually but may have some lasting fibrosis |
| Stent placement for palliation | Rapid relief, but symptoms may return with tumor progression |
| Terminal-stage disease | Typically progressive, requiring feeding tube or palliative care |
In many cases, swallowing may never return to normal, but targeted therapy and symptom management can restore enough function for adequate nutrition and hydration. Some patients find long-term benefit from speech-language pathologists who specialize in swallowing rehab.
What Doctors Emphasize to Patients

Oncology teams often reassure patients that swallowing difficulty is common and manageable, especially when reported early. They encourage patients not to delay seeking help, even for mild symptoms, as early intervention can preserve quality of life and prevent complications like aspiration pneumonia.
Experts also note that patients who communicate openly about eating difficulties tend to stay better nourished and tolerate treatment longer. Gastroenterologists often work alongside oncologists to guide esophageal care, and palliative care teams are brought in earlier than before—not just for end-of-life care, but to enhance symptom control and dignity throughout the cancer journey.
Doctors also highlight the importance of integrated care, which includes dietary support, emotional well-being, and rehabilitation. They emphasize that the goal isn’t just to treat cancer, but to preserve the patient’s ability to enjoy meals, maintain strength, and live meaningfully.
As one oncologist summarized:
“We don’t just treat the tumor. We treat the whole person, including how they eat, how they feel, and how they function every day.”
15+ Questions to Discuss with Your Doctor (FAQ)
1. What causes my difficulty swallowing—tumor growth or treatment side effects?
This is the most important distinction. Tumor growth typically causes narrowing, while radiation or chemotherapy may lead to swelling, ulcers, or nerve damage. Knowing the cause helps guide your care.
2. Could this be the first sign that my cancer has returned or progressed?
Yes. If swallowing becomes harder after a period of improvement, it could indicate recurrence. Your care team may order imaging to check for tumor regrowth.
3. Should I get a swallowing evaluation by a specialist?
Yes, especially if you’re coughing when eating, choking on soft foods, or avoiding meals. A speech-language pathologist can assess your swallowing muscles and recommend safe strategies.
4. Will I need a feeding tube?
Only if you’re losing weight or dehydrated because of severe dysphagia. Feeding tubes are often temporary and can improve strength so you can resume eating by mouth.
5. Are there medications that can help me swallow better?
Yes. Acid reducers, antifungals, or pain-relieving mouthwashes may help if inflammation, reflux, or infection is contributing. Muscle relaxants might also be considered.
6. What foods are safe or recommended for me?
Soft, moist, and pureed foods are easiest. Avoid dry bread, tough meat, and sticky textures. A dietitian can create a plan that’s both safe and enjoyable.
7. Is this related to radiation fibrosis?
If you’ve had radiation, fibrosis can develop months later. It causes stiffness in swallowing muscles or scarring in the esophagus. Imaging and swallow studies help clarify.
8. What imaging or tests do I need to investigate this symptom?
You may need an endoscopy, barium swallow, or CT scan. These can show narrowing, ulceration, or compression by a mass.
9. Can esophageal dilation or stent placement help me?
If the narrowing is due to a tumor or stricture, these procedures can restore function. They are usually safe and provide quick relief.
10. Could an infection be the reason I’m struggling to swallow?
Yes. Patients with compromised immunity can develop fungal or viral infections that irritate the throat or esophagus
11. Is my swallowing issue reversible or permanent?
It depends. If caused by inflammation or treatable narrowing, it may improve. Permanent damage from radiation or nerve involvement may require long-term strategies.
12. Can this lead to aspiration or pneumonia?
Absolutely. Difficulty swallowing can cause food or fluid to enter the lungs. This risk makes early evaluation essential.
13. Should I avoid certain medications or pills?
Yes, some pills are too large or irritating. Your doctor may switch you to liquid forms or advise how to safely take medications.
14. Are there warning signs I should report right away?
Yes. Severe pain when swallowing, coughing blood, or sudden inability to eat are red flags. These may relate to Warning Signs of Cancer progression or complications.
15. How does this symptom fit into the overall picture of my cancer?
Swallowing difficulty is common in this diagnosis and is closely related to stages cancer. It does not necessarily mean a poor prognosis, but needs careful monitoring as part of your Cancer care plan.













