Causes of Shortness of Breath Without Exertion
- Understanding Breathlessness at Rest
- Common Non-Exertional Triggers
- Symptoms That Require Immediate Attention
- When It’s Not the Lungs: Other Systems Involved
- The Role of Anxiety and the Nervous System
- Hormonal Imbalances and Breath Control
- Nutritional Deficiencies and Oxygen Transport
- Medical Conditions That May Cause Silent Breathlessness
- How Digestive Issues Affect Breathing Patterns
- Understanding the Diaphragm’s Role in Silent Dyspnea
- Time-Based Patterns and What They Reveal
- Long-Term Risks of Ignoring Silent Breathlessness
- How Cardiovascular Factors Influence Breathing
- Autoimmune and Inflammatory Triggers
- When Breathlessness Signals Neurological Issues
- Knowing When to Seek Medical Help
- FAQ

Understanding Breathlessness at Rest
Shortness of breath that appears without any physical strain—what’s often described as “air hunger” or unexplained breathlessness—can be unsettling. Unlike post-exercise fatigue, this type of dyspnea arises unexpectedly and without warning. You may notice it while watching TV, lying in bed, or even during quiet moments at your desk.
From what I’ve observed, this kind of breathing discomfort often catches people off guard. It can start with a tight chest or a sudden need to take a deep breath. Unlike normal exertional breathlessness, this isn’t always about being out of shape—it’s frequently tied to your lungs, heart, blood, or even your nervous system. It’s a signal that something deeper might be happening, and it’s important not to brush it off.
Common Non-Exertional Triggers
There are multiple causes of breathlessness at rest, and not all of them are related to the lungs. Some of the most common triggers include heart conditions like arrhythmias or heart failure, silent asthma, anxiety disorders, anemia, and even acid reflux.
From my work with clients, I can say that iron deficiency is a common and overlooked cause. When your body doesn’t have enough oxygen-carrying red blood cells, breathing can feel labored—even at rest. Similarly, anxiety-triggered hyperventilation mimics the sensation of suffocation, although there’s no physical exertion.
One woman I worked with experienced recurring breathlessness after meals. After ruling out heart issues, we discovered her diaphragm was reacting to bloating—a connection we only uncovered after addressing her digestion. That case reminded me how often respiratory symptoms originate outside the lungs.
Symptoms That Require Immediate Attention
Not all breathlessness is a cause for panic, but certain signs demand medical evaluation. If your shortness of breath is accompanied by chest pain, fainting, blue lips or fingertips, or sudden swelling in your legs, don’t wait—get checked immediately.
I’ve seen clients ignore breathlessness for months, attributing it to weight or stress, only to later discover underlying issues like pulmonary embolism or early-stage heart failure. The body whispers before it shouts. Take seriously any persistent changes in your breathing, even if they seem mild.
These red-flag symptoms may also coincide with hidden conditions such as PCOS or thyroid imbalance, which can influence fluid retention and cardiovascular strain. In cases like these, addressing the root disorder can relieve the respiratory symptom.
When It’s Not the Lungs: Other Systems Involved
A common misconception is that breathing issues must mean lung disease. But in reality, many cases I’ve seen are linked to cardiovascular or hematological causes. The heart, blood vessels, and red blood cells all play crucial roles in how oxygen moves through the body.
Heart rhythm irregularities, low hemoglobin, or even hormonal disruptions can trigger breathlessness without any physical trigger. One client had no lung issues but experienced breathlessness linked to pelvic floor tension—a connection that often goes unnoticed. This is where I sometimes refer to resources on how to strengthen pelvic floor muscles, as structural stability in the lower torso can surprisingly influence respiratory ease.
Internal swelling, poor posture, or vascular compression can subtly affect how your diaphragm functions. This shows how interconnected the systems are, and why a full-body evaluation is often more revealing than a chest X-ray alone.
The Role of Anxiety and the Nervous System
From my work with health-conscious clients, one of the most common non-cardiac causes of unexplained breathlessness is anxiety. What many don’t realize is that the nervous system controls breathing patterns—even at rest. A sudden imbalance in the sympathetic (fight-or-flight) and parasympathetic (rest-and-digest) systems can result in hyperventilation or the feeling of “air hunger.”
Anxiety-induced dyspnea doesn’t always feel like a panic attack. Sometimes it appears as a tight throat, shallow breathing, or even yawning fits. I’ve had clients who believed they had asthma, only to find their symptoms resolved through breathwork, grounding techniques, and nervous system regulation.
This is where stress management, vagal tone stimulation, and even bodywork targeting tension in the abdomen or pelvic floor how to strengthen pelvic floor muscles become part of the respiratory healing process.

Hormonal Imbalances and Breath Control
When hormones fluctuate—especially in women—breath regulation can be impacted. I’ve worked with several women experiencing dyspnea tied to thyroid dysfunction, adrenal fatigue, and perimenopause. In some of these cases, hormone shifts caused both chest tightness and erratic heart rhythms, leading to shortness of breath with no exertion involved.
PCOS is another condition that has cropped up more than once in my practice. Women with polycystic ovarian syndrome often face fluid retention, weight gain, and increased cardiovascular load, all of which can subtly affect breathing. One client found that her breathlessness subsided only after improving insulin sensitivity and lowering systemic inflammation. This ties directly into resources like the one I often recommend on natural treatment for PCOS symptoms.
Hormonal regulation doesn’t just impact reproductive health—it’s deeply tied to vascular tone, stress hormones, and even red blood cell production, all of which influence how efficiently the body breathes at rest.
Nutritional Deficiencies and Oxygen Transport
A less obvious but crucial cause of breathlessness is iron deficiency. I can’t count how many clients came to me breathless, tired, and dizzy—only to discover they were significantly low in ferritin or hemoglobin. Iron is vital for carrying oxygen in the blood. When levels drop, the body compensates by trying to breathe more often or more deeply, even when you’re at rest.
This isn’t always full-blown anemia. Sometimes it’s what I call “functional low iron”—where levels are in the lower range, but symptoms are very real. I always look for signs like pale skin, cold extremities, or lightheadedness after meals. In those cases, we work to rebuild iron stores naturally through diet—organ meats, molasses, leafy greens—and through strategic supplementation.
This ties closely to what I’ve discussed before in my article on best supplements for joint pain relief — as nutritional gaps often have ripple effects beyond their primary symptom category.
Medical Conditions That May Cause Silent Breathlessness
Let’s talk about deeper medical issues that may not produce dramatic symptoms at first. Conditions like pulmonary fibrosis, interstitial lung disease, or chronic obstructive pulmonary disease (COPD) can sometimes begin quietly, especially in non-smokers or those with autoimmune tendencies.
I remember a case where a client, an active woman in her 40s, complained of breathlessness only while lying flat. It turned out to be early pulmonary hypertension, which was detected only after a cardiopulmonary stress test. Other conditions that can behave like this include sarcoidosis and lupus.
This is why I urge anyone with consistent, unexplained breathlessness to advocate for thorough testing—not just a spirometry test, but echocardiograms, blood gases, and even sleep studies if needed. The sooner you catch it, the better the outcome.
How Digestive Issues Affect Breathing Patterns
It might sound surprising, but your gut can play a huge role in how you breathe—even when you’re just sitting still. Over the years, I’ve worked with clients who experienced breathlessness due to bloating, acid reflux, or even abdominal adhesions. When the digestive system is inflamed or distended, it can put physical pressure on the diaphragm, restricting normal lung expansion.
One client had persistent breathlessness at night. Eventually, we discovered that her bloating from poorly digested foods was creating upward pressure on her diaphragm. After we adjusted her meal timing and included carminative herbs, the breathlessness disappeared within a week.
For those struggling with digestive tension or gas buildup, I often recommend my piece on natural remedies for bloating and gas — since digestive support can offer direct relief from subtle respiratory symptoms.
Understanding the Diaphragm’s Role in Silent Dyspnea
The diaphragm is the unsung hero of every breath you take. It sits just under your lungs and moves downward to create space during inhalation. When its movement is restricted—due to poor posture, scar tissue, abdominal bloating, or musculoskeletal tension—your breath can become shallow and unsatisfying, even if your lungs are technically healthy.
In my bodywork collaborations, I’ve seen how pelvic and spinal imbalances affect the diaphragm. For example, a woman recovering from a C-section had chronic shortness of breath that improved drastically once we addressed fascial tension along her abdominal wall and lower ribs.
Simple practices like diaphragmatic breathing, gentle thoracic mobility, and even massage can restore function here. If breathlessness feels worse when lying down or after meals, the diaphragm is a suspect worth investigating.
Time-Based Patterns and What They Reveal
Tracking when shortness of breath occurs can offer powerful diagnostic clues. Some people feel breathless at night, others only upon waking, and some when sitting still in the afternoon. Each pattern can point toward a different underlying issue.
To help clients (and now you) identify patterns, I’ve laid out this table based on timing and likely causes:
| Time of Day | Possible Triggers | What to Watch For |
| Morning | Sleep apnea, fluid redistribution, reflux | Dry mouth, fatigue, restless sleep |
| Midday (resting) | Anxiety, blood sugar dips, iron deficiency | Dizziness, jitteriness, weak legs |
| Evening | Digestive pressure, circadian inflammation | Bloating, gassy abdomen, shallow breathing |
| Lying down at night | Orthopnea (heart), diaphragm compression, acid reflux | Need to prop up pillows, coughing, tight chest |
This kind of tracking helped one of my clients pinpoint that her breathlessness was linked to post-meal bloating and reflux—which we solved with a blend of dietary shifts and postural changes.
Long-Term Risks of Ignoring Silent Breathlessness
Ignoring persistent, unexplained breathlessness can have serious long-term consequences. Even when it doesn’t seem urgent, breathlessness can be the earliest symptom of something evolving—something like pulmonary hypertension, left-sided heart failure, or progressive anemia.
In my experience, the most overlooked risk is cardiac strain. If your heart is constantly compensating for poor oxygenation—due to low red blood cell count, fluid overload, or high pressure in the lungs—it will eventually wear out. The person may not feel chest pain, but may notice more fatigue, swelling, or lightheadedness.
Another risk is desensitization. The body adapts to chronic shallow breathing by downregulating sensation. You may not even realize how bad your breathing has become until a stressor (like an infection or travel) tips the balance, triggering a crisis.
That’s why I encourage early attention to any recurring breathlessness, no matter how subtle it seems.
How Cardiovascular Factors Influence Breathing
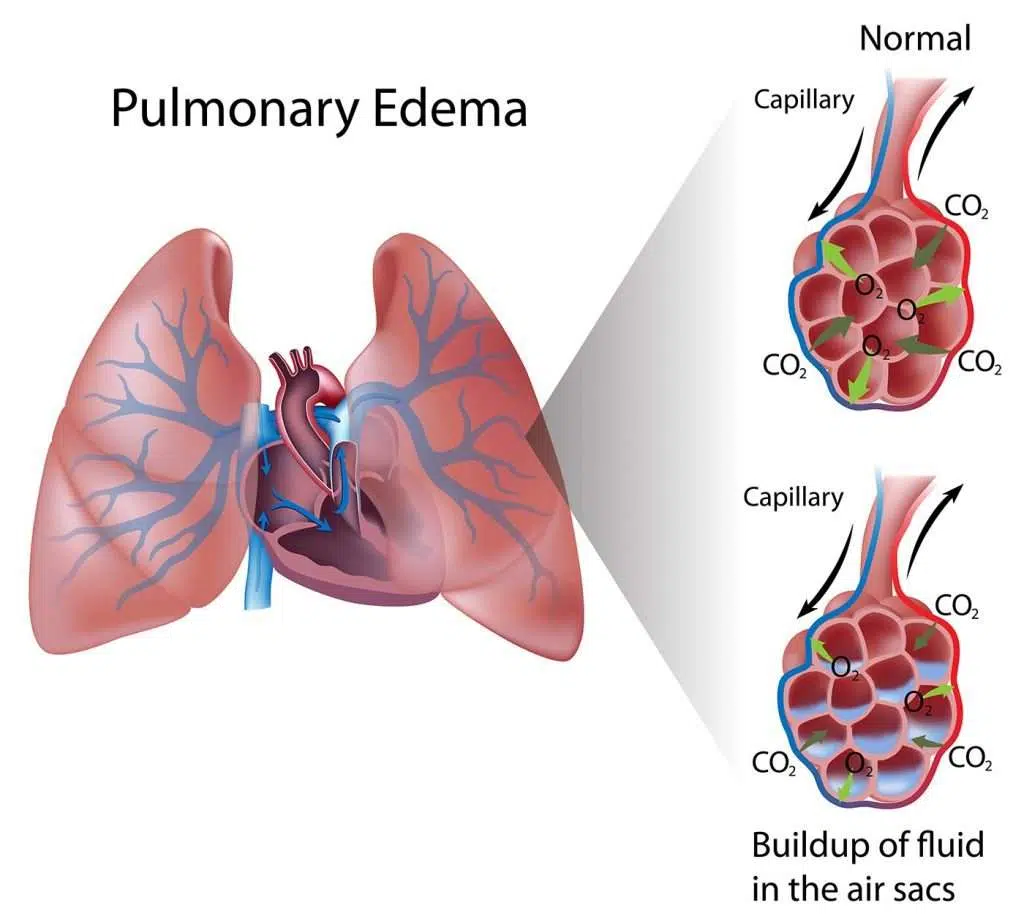
Breathlessness is one of the earliest signs the heart may be under strain. Even in people who don’t show classic symptoms like chest pain or palpitations, the cardiovascular system can still silently impact how efficiently oxygen moves through the body.
I’ve worked with clients whose shortness of breath was tied to mild but chronic left ventricular dysfunction. This means the heart’s left chamber doesn’t pump blood as strongly as it should, leading to subtle congestion in the lungs. These people often felt fine walking, but when lying down or reclining, the breathlessness kicked in.
It’s important not to overlook this connection—even if you’re young and otherwise healthy. Silent hypertension, valve disorders, or pericardial issues can all show up first as quiet changes in breath.
Autoimmune and Inflammatory Triggers
Some of the most puzzling cases I’ve seen involve autoimmune conditions like lupus, rheumatoid arthritis, or sarcoidosis. These diseases can subtly inflame lung tissue, affect blood vessel linings, or lead to low-grade fluid retention—all without obvious respiratory symptoms.
I remember one client who had breathlessness that came and went for months. It turned out to be a mild form of systemic sclerosis affecting the small blood vessels in her lungs. Once we caught it, treatment reduced her symptoms almost entirely.
Even in the absence of a formal diagnosis, I always consider inflammation a potential trigger—especially when breathlessness pairs with joint stiffness, fatigue, or rashes. These signs should never be dismissed.
When Breathlessness Signals Neurological Issues
In rare but important cases, the nervous system itself may be the source. Neurological disorders like multiple sclerosis, myasthenia gravis, or even Parkinson’s disease can impair the brain’s ability to coordinate breathing muscles.
From my time shadowing neurologists, I saw how weak phrenic nerve signaling could result in shallow breathing, particularly during sleep. Clients often didn’t know they were affected until they noticed morning fatigue or had a partner mention unusual breathing patterns at night.
Even more subtle are post-viral syndromes—something I’ve seen increasingly after flu, Epstein-Barr, and COVID infections. In these cases, the breathless feeling doesn’t reflect lung damage, but nerve fatigue and impaired muscle coordination.
Knowing When to Seek Medical Help
This is the most important takeaway I can share: breathlessness without exertion should never be shrugged off. While it often ties to manageable issues like stress or digestion, it can also signal serious systemic changes.
I advise clients to get help if the breathlessness is persistent, worsens when lying down, or comes with chest tightness, swelling, or unexplained fatigue. Don’t wait for dramatic symptoms. Subtle patterns are your body’s early alerts.
Track your symptoms, note any patterns, and push for answers if your doctor dismisses it too quickly. You know your body best. Trust your instincts and seek a second opinion if needed.
FAQ
What vitamin deficiencies can cause shortness of breath?
In my experience, low levels of iron, vitamin B12, and sometimes vitamin D have been linked to shallow or labored breathing, especially at rest. I’ve had clients feel noticeably better after correcting deficiencies that were affecting red blood cell production or nerve function.
Can shortness of breath occur without lung problems?
Absolutely. I’ve seen many cases where the lungs are completely fine, but people still feel breathless due to heart strain, anemia, digestive pressure, or even muscle tension in the chest and diaphragm. It’s not always about the lungs.
Is anxiety the most common reason for breathlessness at rest?
From what I’ve observed, anxiety plays a role in many cases—but not all. The body’s nervous system can trigger fast, shallow breathing without physical exertion. I recommend ruling out other causes before settling on anxiety alone.
Can dehydration cause shortness of breath?
Yes, and I’ve seen it firsthand. When someone is dehydrated, blood volume drops slightly, making circulation less efficient. This can leave you feeling dizzy and short of breath, especially when standing or sitting still for long periods.
How do I know if my breathlessness is from low iron?
If you also feel tired, cold easily, have pale skin, or experience heart palpitations, it’s worth checking your ferritin and hemoglobin levels. I’ve written separately about how to increase iron levels naturally — which has helped many clients regain better breathing and energy.
Can bloating push on the lungs and cause shortness of breath?
Yes, and this is more common than most realize. I’ve worked with clients who feel breathless after large meals or during digestive flare-ups. Supporting gut health often relieves this pressure and restores deeper breathing.
Should I worry if I feel breathless only at night?
Breathlessness that worsens while lying flat is called orthopnea, and from my experience, it often points to heart or diaphragm-related issues. If propping up your head helps, that’s a sign to talk to a doctor.
Is breathlessness linked to blood sugar problems?
It can be. I’ve seen people with low or fluctuating blood sugar experience weak breathing, shakiness, and lightheadedness. Stabilizing meals and snacks helped reduce these symptoms dramatically in several cases.
Can posture affect breathing at rest?
Definitely. Poor posture compresses the diaphragm and chest cavity. I had one client who felt breathless during desk work but not while standing or walking—simply adjusting her seating and practicing breathing posture changed everything.
What if my doctor says it’s ‘just in my head’?
This happens too often, unfortunately. On my end, I always validate clients’ symptoms and dig deeper. Silent physical imbalances are real. Keep searching for answers and don’t hesitate to get a second opinion if you’re dismissed too quickly.
Can shortness of breath come from hormones?
Yes. Especially in women, shifts in progesterone, thyroid hormones, or adrenal function can influence breathing patterns. I’ve worked with clients who had subtle hormonal imbalances that caused breath changes, later confirmed via lab testing.
Is shortness of breath a sign of long COVID?
It can be. I’ve supported several clients with post-COVID symptoms who felt fine during activity but breathless at rest. Nervous system fatigue, subtle inflammation, or blood vessel sensitivity are all possible causes in such cases.
Does low blood pressure cause breathlessness too?
Yes, in some cases. Low blood pressure reduces blood flow and oxygen delivery to tissues, which can leave you feeling breathless even if your oxygen saturation is normal. Hydration and salt intake often helped my clients improve.
How long should I wait before seeing a doctor about it?
If it lasts more than a few days, or if it worsens, I suggest seeing someone right away. I always tell people: breath is life. Subtle changes deserve just as much attention as dramatic ones.
What natural therapies help with unexplained breathlessness?
In my work, I’ve used a mix of postural therapy, breathing retraining, iron-rich foods, gentle mobility, and digestive support to great effect. Every case is different, but gentle, supportive approaches can go a long way.