How to Strengthen Pelvic Floor Muscles Naturally and Effectively
- Understanding the Role of Pelvic Floor Muscles
- Early Symptoms of Pelvic Floor Dysfunction
- Main Causes of Weak Pelvic Floor Muscles
- Different Stages of Pelvic Floor Weakness
- How Nutrition Supports Pelvic Floor Strength
- Breathing and Posture: The Unsung Tools
- Daily Habits That Weaken the Pelvic Floor
- Comparison of Key Supportive Elements
- Movement Practices That Activate the Pelvic Floor
- Pelvic Floor and Hormonal Health
- Postpartum Recovery and the Pelvic Floor
- When to Seek Professional Help
- Aging and the Pelvic Floor: What to Expect
- Integrating Supportive Practices into Your Lifestyle
- Mental and Emotional Dimensions of Pelvic Health
- Long-Term Maintenance and Prevention
- FAQ: Pelvic Floor Strengthening
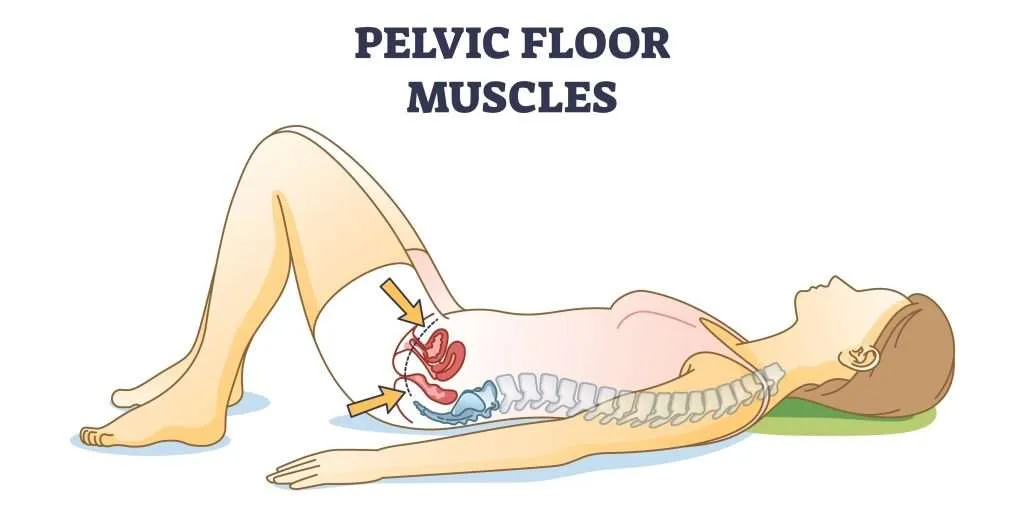
Understanding the Role of Pelvic Floor Muscles
The pelvic floor isn’t just one muscle—it’s a complex group forming a supportive sling beneath your pelvis. These muscles help control bladder and bowel movements, stabilize the spine, and support organs like the uterus and bladder. When they weaken, symptoms can appear slowly and subtly: a slight leak when you sneeze, a dragging sensation in the pelvis, or trouble holding in gas.
Many of my clients don’t realize these signs are related to muscle health. When we correct posture, add breathwork, and train the core safely, the pelvic floor begins to re-engage. A strong pelvic floor isn’t just about avoiding leaks—it enhances confidence, sexual wellness, and even posture.
Early Symptoms of Pelvic Floor Dysfunction
Pelvic floor issues often start with signs so minor they’re easy to brush off. I’ve had women tell me they just thought it was “part of getting older” when they noticed slight incontinence or pressure in the pelvic area. Others describe difficulty starting urination, urgency, or discomfort after standing for too long.
Interestingly, several clients also reported sensations like unsteadiness or feeling faint when rising quickly. After we improved core activation and breath support, many of those symptoms eased—showing how this overlaps with what causes dizziness when standing up. The pelvic floor affects so much more than just bladder control.
Main Causes of Weak Pelvic Floor Muscles
From my experience, childbirth and aging aren’t the only culprits. Prolonged sitting, chronic coughing, heavy lifting with poor technique, and even poor nutrition can slowly undermine pelvic floor strength. Emotional stress can play a role too—clenching through trauma or anxiety often tightens and eventually exhausts these muscles.
Clients who have a history of hormonal imbalances, like those I see when discussing natural treatment for PCOS symptoms, may also face pelvic tension or laxity. The hormonal landscape affects tissue elasticity and muscle tone. That’s why treatment should include a whole-body approach: nutrition, relaxation, and functional movement—not just kegels.

Different Stages of Pelvic Floor Weakness
Pelvic floor dysfunction tends to evolve gradually, which is why early intervention matters. I classify it across three general stages, based on what I’ve observed:
- Mild: Occasional urine leaks during sneezing or laughing, mild pelvic heaviness after standing all day, or needing to go “just in case.”
- Moderate: Noticeable pressure in the pelvic area, frequent urgency, discomfort during intimacy, or difficulty fully emptying the bladder.
- Severe: Prolapse symptoms like tissue bulging, chronic discomfort or pain, consistent incontinence, or severe bowel issues.
Even in more advanced stages, I’ve seen clients regain tone and control—especially when we combine breath-based exercises with lifestyle changes. It’s not about perfection. It’s about awareness, support, and reclaiming stability from the inside out.
How Nutrition Supports Pelvic Floor Strength
In my work with clients, I often remind them that muscles need more than movement—they need nourishment. Protein, magnesium, and essential fatty acids are critical for muscle repair and tissue elasticity. I’ve had women see real change in pelvic stability simply by improving their daily intake of whole foods and reducing inflammatory ingredients like refined sugar and seed oils.
One client I worked with had both pelvic laxity and thinning hair. As we focused on mineral-rich, iron-supportive meals and collagen-building nutrients, her hair improved—and so did her pelvic tone. That’s no surprise, as tissue health is deeply interconnected. In such cases, it’s helpful to explore how to stop hair thinning in females to understand how nutrient deficiencies show up throughout the body.
Breathing and Posture: The Unsung Tools
Most people don’t associate breathing patterns with pelvic floor health—but they absolutely should. I always assess how a client breathes when they walk in. Chest breathing creates tension in the upper body, while proper diaphragmatic breathing helps the pelvic floor relax and engage in harmony with your core.
The diaphragm and pelvic floor are like dance partners—they rise and fall together. Slouching, shallow breathing, or “sucking in” the belly (a habit many women pick up unconsciously) disrupts this balance. When we correct posture, practice breath-led movement, and release tension in the jaw and abdomen, pelvic floor engagement becomes more natural.

Daily Habits That Weaken the Pelvic Floor
From my kitchen days to wellness coaching, I’ve noticed how repetitive patterns influence the body. Crossing your legs too often, wearing high heels daily, holding your breath while lifting, or sitting with a tucked pelvis for hours—all these subtly weaken pelvic engagement.
Habits like rushing to the bathroom “just in case” or avoiding bowel urges also disrupt natural coordination. In one case, a client’s habit of holding in gas while working long hours at a desk contributed to long-term pelvic floor strain. By restoring awareness and timing, her symptoms resolved. It’s small things repeated daily that make or break this system.
Comparison of Key Supportive Elements
| Supportive Element | Role in Pelvic Floor Health | Notes from My Practice |
| Diaphragmatic Breathing | Synchronizes core and pelvic floor engagement | Improved urgency control and stability in many clients |
| Hydration | Prevents constipation and urinary urgency | Dehydrated tissues fatigue faster |
| Magnesium-Rich Foods | Supports muscle relaxation and nerve signaling | Often helps with both cramps and pelvic tension |
| Protein (esp. collagen) | Builds connective tissue and muscle tone | Boosted recovery in postpartum and menopausal clients |
| Posture Awareness | Maintains alignment for optimal pelvic positioning | Reduced heaviness and pressure symptoms |
| Mindful Toileting | Preserves coordination of pelvic muscles | Avoids “just in case” habits that disrupt neuromuscular flow |
Movement Practices That Activate the Pelvic Floor
Over the years, I’ve guided many women through rebuilding pelvic awareness, and I’ve found that the best results come from movement that combines breath, control, and awareness—not intensity. Simple bridges, wall sits, and deep squats done slowly with exhalation on exertion are more effective than a hundred rushed kegels.
Yoga practices that include mula bandha (a gentle pelvic floor lift) have been particularly transformative for clients, especially when paired with breath retention and core control. I recommend starting with small, daily sessions focused on feeling—not forcing—the lift. When practiced consistently, it changes how you move and carry yourself throughout the day.
Pelvic Floor and Hormonal Health
Hormones deeply influence tissue tone, elasticity, and fluid balance—all critical for pelvic floor function. I’ve worked with women experiencing irregular cycles, bloating, and pelvic discomfort who also had weakened support muscles. When we addressed their hormonal balance through food, sleep, and targeted supplementation, the pelvic symptoms often resolved alongside.
This is why I often reference natural treatment for PCOS symptoms when discussing pelvic care with clients who also have irregular menstruation or ovulation issues. Estrogen, insulin, and cortisol fluctuations all affect how muscles and fascia respond. Pelvic floor healing isn’t separate from endocrine balance—it’s a reflection of it.
Postpartum Recovery and the Pelvic Floor
One of the most overlooked periods for pelvic floor support is the months after childbirth. Even in the absence of tearing or complications, the sheer stretching of tissue requires intentional recovery. I’ve seen women struggle with core control, back pain, and incontinence for years simply because they were told to “wait it out.”
When we begin gentle core reintegration—like breathwork, supported pelvic tilts, and glute activation—the results can be surprisingly fast. The key is avoiding overload: no crunches, planks, or jumps early on. Instead, we rebuild the foundation slowly and deliberately, honoring the body’s healing pace.

When to Seek Professional Help
Not all pelvic floor issues can be resolved at home. I always advise clients to consult a pelvic floor physical therapist if they experience persistent symptoms like vaginal bulging, pain during sex, or urinary retention. A trained therapist can assess internal muscle tone, provide manual release when needed, and design a personalized movement plan.
One of my clients assumed she just needed to do more kegels. But after an assessment, we learned her pelvic floor was actually overactive—tight and non-responsive. Only with manual therapy and breath-based relaxation did her symptoms ease. Don’t guess. If something feels off and isn’t improving, professional guidance is worth it.
Aging and the Pelvic Floor: What to Expect
With age, it’s natural for muscle mass and tissue elasticity to decline. But that doesn’t mean pelvic floor dysfunction is inevitable. I’ve worked with women in their 60s and even 70s who regained bladder control and postural strength through targeted routines.
What matters is consistency and care. Don’t rush. Breath, slow muscle recruitment, hydration, and magnesium all remain essential. I often remind older clients that the same principles that help with what causes dizziness when standing up—such as circulation, nervous system support, and muscle reactivation—also help the pelvic floor.
Integrating Supportive Practices into Your Lifestyle
Sustainable healing happens when support is part of your daily rhythm. I encourage clients to pair mindful movement with daily anchors: pelvic lifts while brushing teeth, breath holds while waiting for the kettle, posture checks in the mirror. These tiny practices create massive shifts over time.
Sleep, hydration, and even joy matter. Chronic tension—often held in the pelvis from stress or trauma—can undermine progress. Laughter, community, and relaxation let the nervous system downregulate and the pelvic floor release its chronic hold.
Mental and Emotional Dimensions of Pelvic Health
I’ve seen firsthand how emotional blocks can translate into muscular ones. Many women hold shame, fear, or trauma in the pelvic space. This tension, often unconscious, leads to both overactivity and numbness in the muscles. Emotional release and mental safety are just as important as the exercises.
That’s why practices like somatic therapy, body-based meditation, and mindful self-touch are part of many healing journeys I’ve witnessed. Reclaiming ownership over this space isn’t just physical—it’s an act of integration and self-trust.
Long-Term Maintenance and Prevention
Once you regain pelvic floor strength, keeping it becomes much easier. The body remembers. I tell clients to treat pelvic health like dental hygiene—daily, simple, and non-negotiable. A few minutes of focused breathing, supported squats, or posture correction can prevent regression.
Stay aware of new patterns—sedentary jobs, illness, hormonal shifts, or pregnancy. When life changes, return to your core practices. Even women I’ve helped through menopause maintained control and confidence by adapting—not abandoning—their routines. Just as with hair or gut health, consistency is key to lasting results.
FAQ: Pelvic Floor Strengthening
How long does it take to see results from pelvic floor exercises?
From my experience, many clients begin noticing subtle improvements like reduced urgency or better posture within two to three weeks, provided they’re practicing consistently and mindfully. That said, deeper and more lasting changes—especially in cases like postpartum weakness or overactive muscles—can take up to two or three months. I always tell clients that this is about building long-term resilience, not chasing fast fixes.
Can I do kegels every day?
I’ve worked with women who believed more kegels would fix everything. In reality, daily kegels can be helpful, but only when done with awareness. Too many or too strong can actually lead to a tight, non-cooperative pelvic floor. I suggest starting small, listening to your body, and incorporating release work just as often as contraction.
What if kegels make my symptoms worse?
On several occasions, I’ve met clients whose incontinence or discomfort got worse after starting kegels. This usually meant their pelvic floor was already too tight and needed relaxation, not more tension. If you notice worsening symptoms, I recommend switching focus to breathing and softening exercises and seeking a professional pelvic floor therapist to guide your approach.
Is pelvic floor weakness common after childbirth?
Absolutely. From my work with new mothers, I can confidently say that even “easy” births can overstretch and fatigue the pelvic floor. Recovery isn’t automatic. Without intentional healing, symptoms can linger for years. Gentle reactivation—starting with breath, posture, and alignment—makes a huge difference in both strength and comfort.
Can aging alone cause pelvic issues?
Yes, but it’s not inevitable. On my own clients aged 60+, I’ve seen remarkable results just by reintroducing hydration, movement, and breath awareness. Aging reduces tissue elasticity, but the pelvic floor remains trainable for life. Regular attention is the best form of prevention.
What role does stress play in pelvic dysfunction?
In my experience, chronic stress often shows up as pelvic tightness or numbness. When the nervous system is constantly on alert, muscles tighten—including those we don’t think about. I recommend incorporating stress-reducing habits like walking, laughter, and quiet breathing. It helps the entire core, not just the pelvis.
How do I know if my pelvic floor is too tight or too weak?
This is tricky to self-assess. If you have symptoms like leaking when you sneeze, it could be either. If kegels make things worse or sex feels painful, the muscles may be too tight. I’ve seen clients misdiagnose themselves many times. The best route is to get a proper evaluation with a pelvic therapist.
Can pelvic floor dysfunction affect digestion?
Yes. In fact, I’ve had clients come to me thinking they had IBS, only to find their core and pelvic imbalance was the root. Weak or uncoordinated muscles can affect bowel movements, cause bloating, or create pressure that mimics GI distress. It’s all connected—especially with natural treatment for PCOS symptoms and hormonal regulation involved.
Should I avoid exercise during flare-ups of symptoms?
Not entirely, but I always advise scaling back. Focus on gentle movement, like lying pelvic tilts, breathing, or soft walking. Avoid jumping, running, or heavy lifting until your symptoms stabilize. One of my clients tried pushing through her discomfort, and it only prolonged her healing. Rest with purpose.
Is surgery ever necessary?
Sometimes, especially in severe cases of prolapse or unresolved trauma. But surgery is rarely the first solution. I’ve seen many avoid it by committing to rehab, breathwork, and proper alignment training. Even post-surgery, you’ll need to retrain the muscles or the same symptoms can return.
Can men benefit from pelvic floor work too?
Absolutely. Though I work mainly with women, I’ve also seen male clients with back pain or post-surgical issues improve dramatically with pelvic floor rehab. It supports the entire core and affects bladder control, sexual function, and spinal health in all genders.
What’s the link between hormones and pelvic health?
A strong one. In my experience, hormone fluctuations—especially estrogen and insulin—impact tissue quality, inflammation, and fluid retention. This directly affects how the pelvic floor feels and functions. I often recommend exploring hormonal support in tandem with physical work, especially for women with irregular cycles or menopause.
Are there warning signs I should never ignore?
Yes—things like sudden loss of bladder control, severe pelvic pain, or visible bulging should always be assessed by a professional. I once had a client ignore symptoms for a year assuming it was “just part of aging.” It turned out to be a minor prolapse that could’ve been corrected easily if caught earlier.
Can breathing alone really help?
Yes, and I’ve seen it happen. A client of mine resolved her stress incontinence simply by mastering diaphragmatic breathing and posture control. It doesn’t sound dramatic—but restoring the breath-pelvis connection is the single most powerful and overlooked technique in pelvic floor work.
Do supplements help?
They can. On my recommendation, some clients have used magnesium, collagen, and omega-3s with noticeable improvement—especially when combined with hydration and movement. I wouldn’t rely solely on pills, but they’re a solid part of the support system when used correctly.










