Natural Treatment for PCOS Symptoms: A Comprehensive Guide by a Chef-Turned-Healing Coach
- Understanding the Symptoms of PCOS
- The Stages of PCOS and How They Progress
- How Diet Directly Impacts PCOS Symptoms
- Daily Routine to Naturally Support Hormonal Balance
- Why Blood Sugar Stability Is Critical in PCOS
- Targeted Supplements for PCOS Support
- How Sleep and Light Exposure Influence PCOS Hormones
- Hair Loss, Acne, and Skin Changes in PCOS
- Movement That Supports, Not Stresses, the Body
- Emotional and Mental Health in PCOS Management
- Natural Herbs That Can Ease PCOS Symptoms
- Environmental Toxins That Disrupt Hormones
- PCOS and Gut Health: The Overlooked Link
- How PCOS Affects Fertility and What Can Help
- Short-Term and Long-Term Risks of Ignoring PCOS
- Comparison of Natural PCOS Treatments and Their Focus Areas
- FAQ
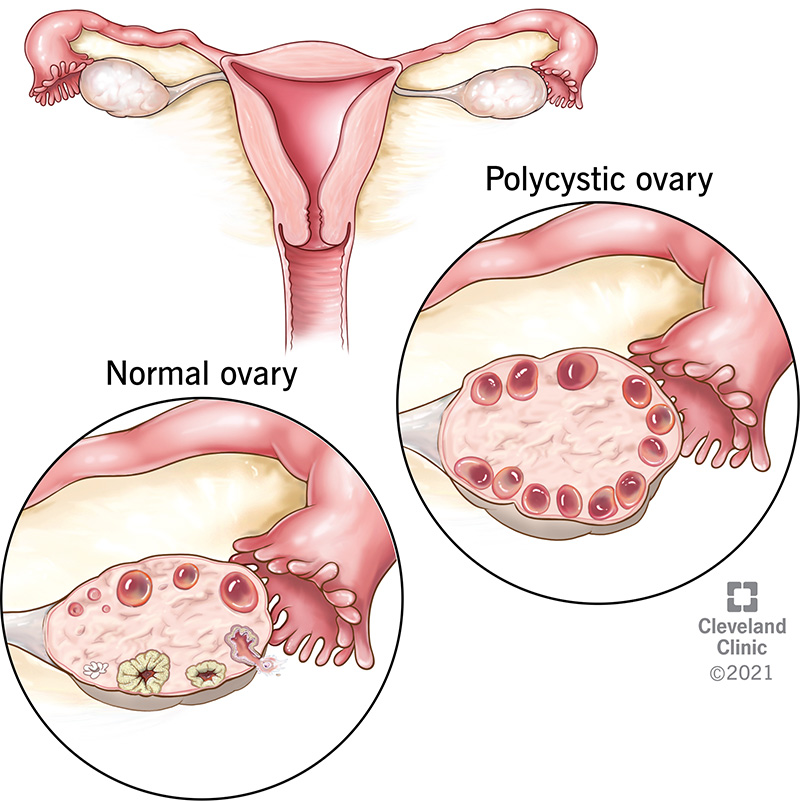
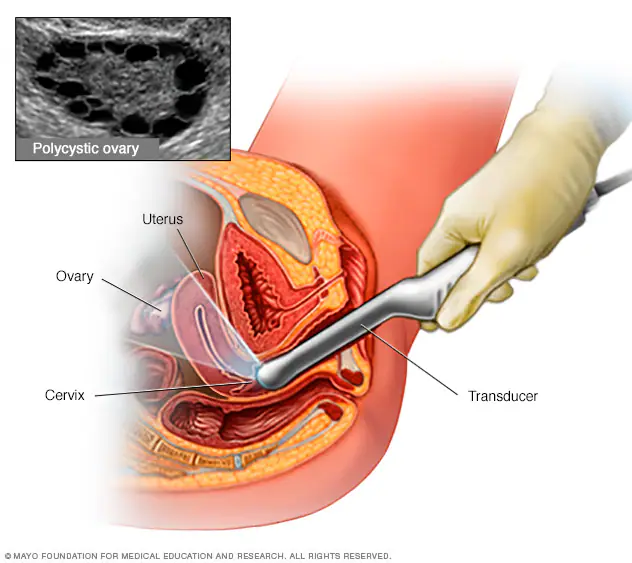
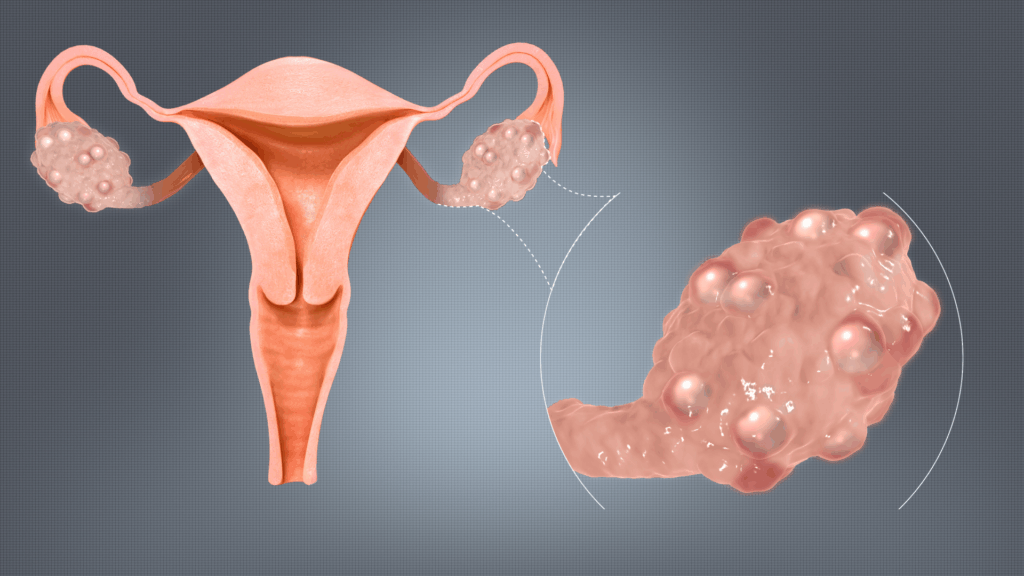
Understanding the Symptoms of PCOS
Polycystic Ovary Syndrome (PCOS) presents in diverse ways, but the most common symptoms include irregular or missed periods, unwanted facial hair, cystic acne, and unexpected weight gain. I’ve had clients come in complaining of anxiety, poor sleep, and mood swings—only to discover later that PCOS was the root cause. These symptoms often overlap with other issues, making diagnosis tricky unless you take a step back and look at the bigger picture.
What’s often overlooked is that symptoms change over time. For example, in early stages, acne and oily skin might be more dominant, but as insulin resistance develops, the person might experience chronic fatigue or find themselves lightheaded when standing — a good time to explore what causes dizziness when standing up. Recognizing patterns is the first step to finding relief.
The Stages of PCOS and How They Progress
In my work with women, I’ve observed three main stages of PCOS manifestation. Early on, it can feel like an occasional nuisance—missed cycles here and there, minor bloating, or weight fluctuation. The middle stage brings more hormonal chaos: androgens rise, insulin resistance worsens, and anxiety becomes more pronounced. Advanced stages often show signs of chronic inflammation, skin discoloration, and even fertility challenges.
These stages aren’t fixed, and with proper care, I’ve seen women reverse progression. One of my clients, for example, moved from an advanced state with severe hair thinning (we tied it to how to stop hair thinning in females) to a stable, ovulating cycle again within a year. The body, if supported correctly, can rebalance.
How Diet Directly Impacts PCOS Symptoms
Food was my doorway into healing, and for many of my clients, it’s the most tangible way to begin. PCOS is deeply influenced by insulin and inflammation—two areas diet can dramatically affect. I’ve found that focusing on whole, unprocessed ingredients and reducing refined carbs makes an enormous difference. Not “no carbs”—but slow carbs, like lentils, quinoa, and sweet potatoes.
Anti-inflammatory herbs like turmeric, cinnamon, and ginger have helped dozens of my clients manage blood sugar and pain. Interestingly, some who struggled with persistent bloating and gas found relief when we integrated natural remedies for bloating and gas, which also lowered internal stress and improved cycle regularity. Food choices ripple far beyond the plate.
Daily Routine to Naturally Support Hormonal Balance
Here is a sample structure I often recommend as a foundation for healing PCOS symptoms. I’ve personally tested and refined this through years of guiding clients.
| Time | Action |
| 7:00 AM | Wake up, sunlight exposure, warm lemon water with a pinch of sea salt |
| 8:00 AM | Protein-rich breakfast (e.g., egg, lentils, or tofu scramble) |
| 10:30 AM | Gentle movement — walk or yoga |
| 1:00 PM | Balanced lunch with healthy fats and fiber-rich carbs |
| 3:00 PM | Herbal tea with spearmint or dandelion, screen break |
| 5:30 PM | Evening walk or resistance band exercises |
| 7:00 PM | Light dinner, avoid sugars or heavy carbs |
| 9:30 PM | Magnesium-rich snack (pumpkin seeds or banana), dim lighting |
| 10:30 PM | Sleep in total darkness, away from screens |
This rhythm helps sync circadian hormones, support digestion, and gradually recalibrate the body’s stress and insulin response.
Why Blood Sugar Stability Is Critical in PCOS
One of the most underestimated pieces of the PCOS puzzle is blood sugar regulation. You don’t need to be diabetic to suffer from the effects of insulin resistance, which is present in the majority of PCOS cases I’ve seen. When blood sugar spikes and crashes repeatedly, it sends hormonal signals into chaos. Cortisol rises, ovulation halts, and symptoms like fatigue, mood swings, and stubborn belly weight intensify.
I’ve guided women through gradual dietary shifts—starting with balancing each meal with protein, healthy fats, and fiber. Those with morning dizziness, for instance, usually improved after stabilizing their glucose intake and learning more about what causes dizziness when standing up. It’s a foundational piece for long-term hormone repair.

Targeted Supplements for PCOS Support
Supplements aren’t magic pills, but when used mindfully, they can accelerate recovery. I typically recommend starting with magnesium, zinc, omega-3s, and inositol—especially myo-inositol combined with D-chiro-inositol. These help improve insulin sensitivity, reduce androgens, and regulate cycles.
I had one client who was plagued by mood crashes and sugar cravings despite eating well. Once we added magnesium glycinate and chromium picolinate, her energy improved within a week. Always pair supplements with testing, but when used intentionally, they can bridge key nutritional gaps.
How Sleep and Light Exposure Influence PCOS Hormones
Many women I’ve worked with overlook the role of circadian rhythm in hormone health. Poor sleep quality, late nights, or constant screen exposure disrupt the brain’s communication with ovaries and adrenal glands. Melatonin and cortisol are tightly linked to reproductive hormones.
I recommend rising with natural light and winding down with darkness. One of my clients made no dietary changes but simply began dimming lights by 9 p.m. and waking with sunrise—and her periods resumed after four months of being absent. It’s a reminder that light is as medicinal as food in the PCOS journey.
Hair Loss, Acne, and Skin Changes in PCOS
From my experience, one of the most emotionally difficult aspects of PCOS is how it shows on the outside. Hair thinning, oily skin, and painful cystic acne are often the first visible signs. Androgen excess fuels these changes, but it’s not unfixable. I often focus on internal anti-inflammatory support, liver detoxification, and zinc intake.
A woman I supported had been using topical treatments for years without results. When we addressed gut health, improved iron stores, and followed insights from how to stop hair thinning in females, her skin calmed and hair density improved. External symptoms are often internal signals.
Movement That Supports, Not Stresses, the Body
When I first began helping women with PCOS, many assumed high-intensity workouts were necessary for weight loss and hormone regulation. But what I noticed time and again is that over-exercising, especially with cardio, often worsens symptoms—triggering more cortisol and cycle disruption.
Instead, I encourage movement that supports the nervous system: walking outdoors, yoga, resistance training with bands, and dancing. One client swapped her daily HIIT with afternoon walks and noticed reduced bloating and calmer moods within two weeks. We even explored natural remedies for bloating and gas alongside these gentler workouts, and the synergy worked wonders.
Emotional and Mental Health in PCOS Management
PCOS is as much an emotional condition as a physical one. The irregular cycles, infertility fears, and body changes can trigger intense anxiety, frustration, and low self-worth. In my sessions, I’ve seen how emotional healing—through journaling, therapy, or simply voicing shame—can ease physical symptoms.
A woman I worked with finally acknowledged the stress she was holding around weight and perfectionism. As we shifted her mindset and she added breathing techniques and self-forgiveness to her daily routine, her cravings decreased and sleep deepened. The body often responds when the heart feels safe.
Natural Herbs That Can Ease PCOS Symptoms
Over time, I’ve come to respect the power of adaptogenic and hormone-balancing herbs. Spearmint tea is one of my go-tos—it’s been shown to reduce testosterone naturally. I’ve also used chasteberry (Vitex), maca root, and ashwagandha in protocols depending on a woman’s cycle and stress levels.
I remember a particularly anxious client who responded quickly to daily ashwagandha powder in her smoothie. Within weeks, her sleep and skin improved. Herbal care requires patience and personalization, but when aligned with your body’s needs, it can truly support hormonal recalibration.
Environmental Toxins That Disrupt Hormones
Many people don’t realize how much their environment affects hormone health. Endocrine-disrupting chemicals found in plastics, beauty products, nonstick cookware, and even receipts can mimic estrogen or interfere with progesterone. For my clients, reducing exposure often leads to surprising improvements.
I advise using glass containers, fragrance-free natural cosmetics, and switching to stainless steel or cast iron cookware. One client, after eliminating synthetic perfumes and plastics in the kitchen, reported clearer skin and lighter, more regular periods within three months. This layer of care can be subtle but powerful.
PCOS and Gut Health: The Overlooked Link
In my work with women who struggle with PCOS, I’ve consistently found that addressing gut health accelerates progress. The gut influences everything from nutrient absorption to estrogen detoxification. When it’s inflamed or leaky, hormones become harder to regulate, and symptoms like acne, mood instability, and sugar cravings intensify.
I guided one client through a simple protocol: eliminating processed dairy, incorporating fermented foods, and focusing on fiber from vegetables and lentils. Her bloating subsided, skin cleared, and PMS intensity dropped dramatically. This gut-hormone connection was also key in managing her occasional fatigue spells tied to what causes dizziness when standing up.
How PCOS Affects Fertility and What Can Help
Fertility concerns are one of the most emotionally charged aspects of PCOS. The irregular or absent ovulation often makes conception feel impossible. But I’ve seen many women restore their cycles and conceive naturally through targeted lifestyle changes. The body often just needs the right environment to trust again.
For example, we focused on blood sugar balance, anti-inflammatory foods, emotional healing, and nutrients like folate and omega-3s. One of my clients conceived after six months of cycle tracking and working through hormone repair with me. Patience is part of the process—but natural pregnancy with PCOS is entirely possible.
Short-Term and Long-Term Risks of Ignoring PCOS
Ignoring PCOS can result in more than just irregular periods. Over time, the condition can lead to type 2 diabetes, cardiovascular disease, metabolic syndrome, infertility, and endometrial hyperplasia. Short-term issues like fatigue and skin flare-ups may seem minor, but they often signal deeper imbalances.
I once worked with a woman who brushed off her symptoms for years. By the time we connected, she had insulin resistance and anxiety that disrupted her daily life. Within six months of support—including addressing how to increase iron levels naturally—she began reversing those patterns. Acting early makes a lasting difference.
Comparison of Natural PCOS Treatments and Their Focus Areas
| Approach | Targeted Symptoms | Best For |
| Anti-inflammatory diet | Acne, bloating, mood swings | Early to moderate PCOS |
| Blood sugar balancing meals | Fatigue, cravings, irregular cycles | All stages |
| Adaptogenic herbs (e.g. maca) | Stress, sleep, hormone irregularities | Stress-driven PCOS |
| Myo-Inositol + D-chiro combo | Ovulation support, fertility | TTC (trying to conceive), cycle issues |
| Gut healing protocols | Bloating, acne, mental fog | Gut-disrupted or IBS-type PCOS |
| Emotional release practices | Anxiety, body shame, poor sleep | High-stress lifestyle |
| Toxin reduction (environment) | Hormonal acne, weight retention | Moderate to advanced PCOS cases |
This table summarizes what I’ve seen work in real-life applications. Tailoring the approach to your body’s unique patterns is the key to lasting relief.
FAQ
Can stress really worsen PCOS?
Absolutely. I’ve seen women’s symptoms flare during work deadlines or emotional upheaval. Cortisol impacts blood sugar, ovulation, and inflammation. Addressing emotional health is non-negotiable in healing PCOS naturally. Even simple practices like breathwork or walking without distractions can bring noticeable relief. On my experience, stress management often acts as the switch that turns improvements from temporary to lasting.
How important is sleep for PCOS?
It’s essential. From my experience, women who improve sleep quality often see better cycles, skin, and weight regulation. Melatonin and cortisol directly affect hormones like LH and FSH. I’ve worked with clients who made no dietary changes but simply fixed their circadian rhythm—and they saw restored ovulation within weeks. Sleep isn’t a luxury in PCOS care. It’s therapy.
Can I follow a vegetarian or vegan diet for PCOS?
Yes, but it requires planning. I’ve supported vegan clients who did well once they prioritized protein through legumes, tempeh, and seeds, and supplemented with B12, iron, and omega-3s. Low-protein vegan diets often worsen fatigue and hair thinning, but balanced plant-based meals can support hormonal health.
Is PCOS related to thyroid problems?
They often overlap. I’ve had several clients with undiagnosed hypothyroidism that masked as PCOS—or vice versa. Symptoms like fatigue, irregular periods, and cold intolerance can come from either condition. I always suggest testing TSH, Free T3, and Free T4 alongside reproductive hormones when symptoms are complex.
Do birth control pills fix PCOS?
They mask symptoms, but they don’t resolve the root causes. I’ve seen women experience relief from acne or bleeding on the pill, only for symptoms to return post-pill. In my practice, I help clients support their hormones naturally before and after stopping hormonal contraceptives.
Can I get pregnant naturally with PCOS?
Yes. I’ve helped many women conceive naturally, even after years of irregular periods. Restoring ovulation through blood sugar balance, nutrient support, stress reduction, and sometimes inositol or herbal aids can be enough. Fertility with PCOS takes patience, but it’s absolutely within reach.
What’s the difference between PCOS and endometriosis?
They’re different but can coexist. PCOS is rooted in ovulatory dysfunction and hormone imbalance, while endometriosis involves tissue growth outside the uterus. I’ve worked with clients who had both, and treatment for each needs a separate, tailored approach—though anti-inflammatory support benefits both.
Is it safe to treat PCOS naturally without medication?
In most cases, yes. From my clinical experience, natural treatment has not only been safe but more sustainable. However, I always advise working alongside a qualified professional to ensure that nothing serious is being missed. Lifestyle medicine is powerful when applied with clarity and care.









