Stage 3 Bowel Cancer
Stage 3 Bowel Cancer: Survival Rate
- What Is Stage 3 Bowel Cancer?
- How Is Stage 3 Bowel Cancer Diagnosed?
- Survival Rates for Stage 3 Bowel Cancer
- The Role of Surgery and Chemotherapy
- Common Symptoms and How They Progress
- Prognostic Factors Influencing Survival
- Living With Stage 3 Bowel Cancer: Physical and Emotional Impact
- Detecting Recurrence and Monitoring After Treatment
- Role of Chemotherapy and Adjuvant Therapies
- Importance of Nutrition During and After Treatment
- Impact on Daily Function and Return to Work
- Risk of Secondary Cancers and Long-Term Complications
- The Role of Genetics and Family History
- Comparing Stage 3 to Other Bowel Cancer Stages
- Early Warning Signs and Missed Diagnoses
- Monitoring Survivors: Follow-Up and Recurrence Prevention
- FAQ: Common Questions About Stage 3 Bowel Cancer Survival Rate
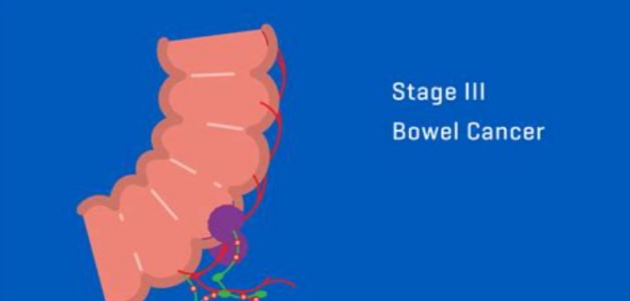
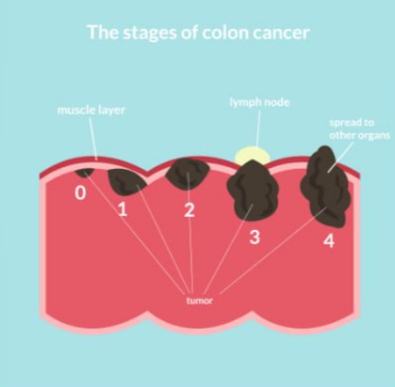
What Is Stage 3 Bowel Cancer?
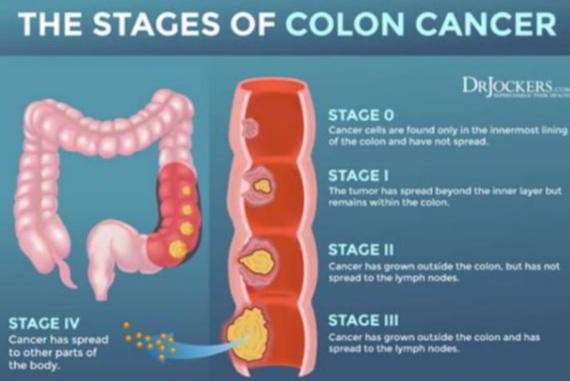
Stage 3 bowel cancer means the disease has spread beyond the inner layers of the bowel wall and into nearby lymph nodes, but not yet to distant organs. This is considered an advanced but potentially curable stage. The cancer is often subdivided into stage 3A, 3B, and 3C, depending on how many lymph nodes are involved and how far the tumor has grown into the bowel wall.
At this stage, timely treatment is essential. The prognosis is still hopeful with aggressive treatment, including surgery and chemotherapy. However, the presence of lymph node involvement indicates a higher chance of recurrence, which is why long-term follow-up and staging accuracy are critical.
How Is Stage 3 Bowel Cancer Diagnosed?
Diagnosis is typically confirmed through a combination of imaging studies, endoscopic procedures, and biopsy. Common diagnostic tools include:
- Colonoscopy with tissue biopsy to confirm malignancy.
- CT scans or MRIs to assess local spread and lymph node involvement.
- PET scans when there’s uncertainty about distant metastasis.
- CEA blood test to monitor cancer activity pre- and post-treatment.
Accurate staging is essential not only for predicting outcomes but also for choosing the right combination of therapies. In many cases, bowel obstruction, bleeding, or fatigue prompt the initial clinical suspicion.
One must also consider that certain early symptoms like bowel discomfort, unexplained weight loss, or back pain may go unnoticed for months. These signs are often mistakenly attributed to benign issues, which delays diagnosis. A related concern to be aware of is bowel leakage, which can sometimes be an early indicator of cancer.
Survival Rates for Stage 3 Bowel Cancer
Survival statistics offer a general idea but should be interpreted cautiously. For stage 3 bowel cancer, the average 5-year survival rate is around 60–75%, depending on substage, patient health, and treatment response.
Here’s a breakdown by substage:
| Stage 3 Subtype | 5-Year Survival Rate |
| Stage 3A | 75–85% |
| Stage 3B | 60–70% |
| Stage 3C | 40–60% |
Factors influencing survival include:
- Number of affected lymph nodes
- Tumor size and location (colon vs. rectum)
- Response to chemotherapy
- Molecular markers like KRAS and BRAF mutations
- General health and age at diagnosis
It’s also important to recognize that lifestyle changes and follow-up strategies significantly impact long-term outcomes. Survivors who maintain a healthy diet and manage inflammation markers tend to do better over time.
The Role of Surgery and Chemotherapy
Treatment for stage 3 bowel cancer typically starts with surgical resection of the tumor and affected lymph nodes. In some cases, neoadjuvant chemotherapy (before surgery) is used to shrink the tumor, especially when the mass is large or close to vital structures.
Postoperative treatment almost always includes adjuvant chemotherapy, commonly the FOLFOX regimen (5-FU, leucovorin, and oxaliplatin), which targets remaining microscopic cancer cells.
Chemotherapy may last from 3 to 6 months, depending on the patient’s tolerance and risk of recurrence. Side effects like fatigue, neuropathy, and gastrointestinal upset are managed with supportive care.
Radiation is used more frequently in rectal cancer than in colon cancer, especially if there’s a risk of local recurrence. It’s usually applied before surgery to increase the chance of clear margins.
Patients experiencing lower back pain after treatment should not ignore it — this can be a red flag, especially in the context of Back Ache and Bowel Cancer. Ongoing monitoring and reporting of any new symptoms remain a key part of survivorship.
Common Symptoms and How They Progress
The symptoms of stage 3 bowel cancer often resemble earlier stages but tend to intensify as the disease advances. These can include:
- Persistent changes in bowel habits (diarrhea, constipation, or narrowing of stool)
- Rectal bleeding or blood in the stool
- Abdominal pain or cramping
- Fatigue and weakness due to anemia
- Unintended weight loss
- A feeling of incomplete bowel emptying
In some cases, patients may also report vague discomfort or bloating that doesn’t resolve. Importantly, these symptoms often develop gradually, making them easy to overlook or dismiss.
It’s crucial to pay attention to how symptoms evolve over time. For instance, subtle bleeding may eventually become visible in stools, and occasional cramping might develop into persistent pain. One symptom that deserves more awareness is back pain. Though commonly overlooked, chronic back discomfort can be associated with bowel cancer, especially when tumors press on nerves or organs. This relationship is discussed further in Back Ache and Bowel Cancer.
Prognostic Factors Influencing Survival
Several variables influence the long-term outlook for individuals with stage 3 bowel cancer. These prognostic factors include:
- Number of lymph nodes affected: More nodes generally indicate a higher risk of recurrence.
- Tumor grade: High-grade tumors grow and spread faster than low-grade ones.
- Margins of surgical resection: If cancer cells remain at the margins, the risk of recurrence rises.
- Molecular profile: Certain mutations such as KRAS or MSI (microsatellite instability) impact both prognosis and treatment options.
- Patient’s immune response: Strong immune activity may correlate with improved survival.
Doctors often use these factors, in conjunction with TNM staging, to determine whether additional therapies are needed after surgery. Personalized medicine plays an increasing role in predicting which patients benefit most from specific chemotherapy combinations.
Living With Stage 3 Bowel Cancer: Physical and Emotional Impact
A stage 3 cancer diagnosis is life-altering. Patients often go through cycles of hope, fear, and physical exhaustion. Post-surgical recovery may take weeks to months, especially if a colostomy or ileostomy is involved. These lifestyle changes demand emotional resilience and support systems.
Common challenges include:
- Dealing with the physical effects of chemotherapy
- Adjusting to dietary restrictions
- Navigating social isolation or work limitations
- Managing anxiety about recurrence
Access to survivorship programs, counseling, and cancer-specific dietitians can greatly improve quality of life. Some patients also explore alternative therapies (like acupuncture or meditation) as complementary tools to conventional care.
It’s vital not to dismiss early bodily changes as “normal aging.” For example, early-stage bowel cancer may show up only as mild symptoms, such as occasional bloating or changes in stool consistency. These subtle signs are explored further in Symptom of Bowel Cancer.
Detecting Recurrence and Monitoring After Treatment
After curative treatment, stage 3 bowel cancer survivors require long-term monitoring. The first 2–3 years post-treatment are critical, as this is when most recurrences happen.
Follow-up typically includes:
- Regular colonoscopies every 1 to 3 years
- CEA blood tests every 3–6 months for the first few years
- CT scans annually or as needed
- Physical exams and symptom tracking during each oncology visit
A major concern in this period is local recurrence or distant metastasis (especially to the liver or lungs). Early detection of recurrence improves the chances of successful secondary treatment.
Patients should promptly report symptoms such as new pain, bowel habit changes, or unexplained fatigue. Even seemingly minor concerns, like mild leakage or gas retention, could warrant evaluation. That’s why recognizing Is Bowel Leakage a Sign of Cancer is essential in the post-treatment landscape.
Role of Chemotherapy and Adjuvant Therapies
For most patients with stage 3 bowel cancer, chemotherapy is a standard part of treatment following surgery. The most commonly used regimen is FOLFOX, which includes 5-fluorouracil, leucovorin, and oxaliplatin. This combination targets residual cancer cells that surgery may have missed, aiming to reduce recurrence risk.
Duration usually spans 6 months, depending on the patient’s tolerance and tumor biology. While effective, chemotherapy can cause side effects such as neuropathy, fatigue, nausea, and lowered immunity. Patients with MSI-high tumors might not benefit as much from traditional chemotherapy but may respond better to immunotherapy in some clinical trials.
In addition to systemic treatments, some patients may be candidates for targeted therapies or clinical trials testing the next generation of precision drugs. These options are especially important when standard treatment is not fully effective or tolerated.
Importance of Nutrition During and After Treatment
Nutrition plays a vital role in recovery and survival after a stage 3 bowel cancer diagnosis. Malnutrition is common due to surgical changes, appetite loss, and the gastrointestinal effects of chemotherapy.
Dietary guidance usually focuses on:
- Easily digestible, high-protein meals
- Avoiding high-fiber foods immediately post-surgery
- Incorporating fermented foods and probiotics to rebuild gut flora
- Staying hydrated to support kidney function and bowel regularity
Registered dietitians who specialize in oncology are essential members of the care team. Over time, many patients transition to a Mediterranean-style diet, which has been shown to support gut health and lower inflammation. Maintaining a healthy weight post-treatment is also correlated with improved survival.
Impact on Daily Function and Return to Work
Reentering daily life after stage 3 bowel cancer treatment involves a balance between recovery and reintegration. Physical recovery from abdominal surgery may take weeks or months, especially if a stoma was created. Patients often report fatigue, brain fog, or lingering digestive problems that affect their work capacity.
Social reintegration can be just as challenging. People may feel isolated, misunderstood, or uncomfortable discussing their medical history. Support groups and survivorship clinics offer helpful resources to ease this transition.
Some employers offer phased returns or hybrid roles that accommodate the energy fluctuations common during recovery. It’s important for patients to advocate for themselves and communicate openly with care teams and workplaces.
Risk of Secondary Cancers and Long-Term Complications
After surviving stage 3 bowel cancer, patients remain at increased risk for secondary malignancies, especially in the gastrointestinal tract. These risks are influenced by genetic syndromes (like Lynch syndrome), radiation exposure, and chemotherapy history.
Common long-term complications include:
- Neuropathy from oxaliplatin
- Bowel dysfunction, such as urgency or incontinence
- Sexual dysfunction and changes in intimacy
- Mental health struggles like depression or PTSD
Routine follow-up is essential to catch these issues early. Genetic testing may also be recommended for those with strong family histories or early-onset cancer.
Awareness campaigns now encourage survivors to monitor for early signs of relapse or new cancers. Educational initiatives have made progress in clarifying which symptoms to report and which warrant investigation. Discussions around Symptom of Bowel Cancer are particularly valuable in ongoing survivorship planning.
The Role of Genetics and Family History
Genetics significantly influences the likelihood of developing stage 3 bowel cancer and impacts survival. Individuals with inherited conditions such as Lynch syndrome or familial adenomatous polyposis (FAP) have a markedly higher risk of both developing cancer and experiencing recurrence. Genetic counseling is often recommended for patients diagnosed under age 50 or with a strong family history of colorectal or related cancers.
Testing can reveal mutations in genes such as MLH1, MSH2, or APC, which not only guide screening for relatives but also inform treatment choices. For example, MSI-high or MMR-deficient tumors may respond better to immunotherapy rather than traditional chemotherapy.
This understanding aligns with new approaches to personalized medicine—where the treatment plan is tailored based on individual genetic markers. It also informs long-term screening strategies for family members.
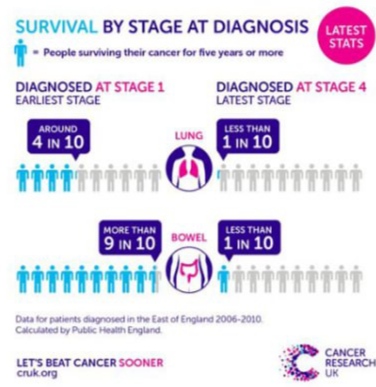
Comparing Stage 3 to Other Bowel Cancer Stages
The survival rate for stage 3 bowel cancer is notably lower than that of stage 1 or 2, but higher than stage 4. Understanding this contrast helps patients grasp the urgency of timely diagnosis and intervention.
| Stage | Description | 5-Year Survival Rate |
| Stage 1 | Tumor limited to bowel wall | ~90% |
| Stage 2 | Tumor has spread through bowel wall but not to nodes | ~70–85% |
| Stage 3 | Tumor has spread to regional lymph nodes | ~50–75% |
| Stage 4 | Tumor has metastasized to distant organs | ~10–15% |
The wide range for stage 3 reflects variations within the stage (e.g., number of nodes affected, tumor grade) and patient-specific factors such as age, health status, and response to treatment. Patients often ask how Back Ache and Bowel Cancer might be connected, since symptoms don’t always align neatly with cancer stage.
Early Warning Signs and Missed Diagnoses
Stage 3 bowel cancer is often diagnosed when symptoms worsen and interfere with daily life, but some signs are easily missed or dismissed. This includes:
- Rectal bleeding mistaken for hemorrhoids
- Abdominal discomfort attributed to IBS
- Fatigue and anemia assumed to be unrelated
Primary care physicians sometimes overlook these symptoms, particularly in younger patients. As awareness grows, campaigns are stressing the importance of reporting changes in bowel habits, even when they seem minor.
Certain symptoms—like Is Bowel Leakage a Sign of Cancer —are still under-discussed despite their relevance. Encouraging patients to track and report these issues may lead to earlier interventions and better outcomes.
Monitoring Survivors: Follow-Up and Recurrence Prevention
Once treatment is completed, survivors enter a structured follow-up phase. The first 2–3 years post-treatment are critical due to the higher chance of recurrence. Follow-up includes:
- CT scans every 6–12 months
- Colonoscopy within 1 year post-surgery, then at regular intervals
- Carcinoembryonic antigen (CEA) blood tests
- Clinical exams and symptom reviews
Lifestyle changes also play a major role. Patients are advised to reduce red and processed meat intake, increase fiber, exercise regularly, and limit alcohol. Maintaining a healthy BMI may also help prevent recurrence.
New approaches include the use of circulating tumor DNA (ctDNA) to detect microscopic disease earlier than imaging or blood tests. These tools enhance early relapse detection and improve survival.
FAQ: Common Questions About Stage 3 Bowel Cancer Survival Rate
1. Can stress impact survival rates in stage 3 bowel cancer?
Chronic stress can indirectly affect survival by weakening the immune system, increasing inflammation, and decreasing adherence to treatment. While stress alone doesn’t cause cancer progression, it may compromise the body’s ability to cope with therapy and recovery. Supportive counseling and mind–body practices like meditation are often recommended.
2. Does age affect survival in stage 3 bowel cancer?
Yes, age plays a significant role. Younger patients typically have better overall survival due to better organ function and fewer co-morbidities. However, older adults can still respond well to treatment, particularly if they maintain good general health and tolerate chemotherapy well.
3. Can stage 3 bowel cancer go into remission?
Yes. Many patients with stage 3 bowel cancer achieve full remission following surgery and adjuvant therapy. Remission means no detectable signs of cancer at the time, but continuous monitoring is necessary since recurrence risk remains.
4. Is surgery always required for stage 3 bowel cancer?
Almost always, yes. Surgery to remove the tumor and nearby lymph nodes is standard for curative treatment. Chemotherapy follows to eliminate microscopic cancer cells and reduce recurrence risk.
5. What role does immunotherapy play in stage 3 treatment?
Immunotherapy isn’t currently the standard for all stage 3 cases but may be used when tumors show mismatch repair deficiency (dMMR) or high microsatellite instability (MSI-H). These patients are more likely to benefit from checkpoint inhibitors.
6. Can lifestyle changes improve survival chances?
Absolutely. Regular physical activity, plant-rich diets, weight control, and smoking cessation all contribute to improved outcomes. Lifestyle adjustments can also reduce treatment side effects and enhance overall well-being.
7. How soon after diagnosis should treatment begin?
Ideally within a few weeks. Delays beyond 8 weeks between diagnosis and surgery or the start of chemotherapy may negatively impact outcomes. Prompt action ensures better response rates.
8. Can stage 3 bowel cancer return after treatment?
Yes, recurrence is possible, particularly in the first 2–3 years after initial treatment. Regular follow-up is designed to catch recurrences early when they are still treatable.
9. How does tumor location (left vs. right colon) affect survival?
Left-sided tumors generally have a slightly better prognosis than right-sided ones. Right-sided cancers are sometimes detected later and may have different molecular characteristics affecting responsiveness to treatment.
10. Are certain races or ethnic groups at higher risk?
Yes. African American individuals tend to have higher incidence and mortality rates, partly due to disparities in access to screening and care. Tailored community outreach and early screening are essential.
11. Does gender affect survival rates?
Some studies suggest that women may have slightly better survival outcomes, potentially due to hormonal or genetic differences. However, the differences are modest and not a basis for altering treatment protocols.
12. What is the role of complementary therapies like acupuncture or herbal medicine?
These therapies may help manage side effects such as nausea or fatigue, but they should never replace medical treatment. Always consult your oncologist before starting any alternative therapy.
13. How long does chemotherapy last for stage 3 bowel cancer?
Adjuvant chemotherapy usually lasts around 3 to 6 months, depending on the regimen and patient tolerance. The most common drugs are FOLFOX or CAPOX.
14. Is bowel obstruction a sign of advanced cancer?
It can be. A bowel obstruction may indicate that the tumor has grown significantly or recurred. However, not all obstructions are cancer-related, so diagnostic imaging is required.
15. Can early screening prevent stage 3 diagnosis?
Yes. Routine colonoscopies can detect precancerous polyps or early-stage cancers before they progress to stage 3. Early detection remains the most effective tool for improving survival.