Understanding Penile Cancer
Understanding Penile Cancer: A Comprehensive Guide for Patients and Families
- What Is Penile Cancer and Why It Matters
- Recognizing the Early Signs and Symptoms of Penile Cancer
- Key Causes and Risk Factors: Who Is Most at Risk?
- How Penile Cancer Is Diagnosed: Tests and Clinical Approach
- Understanding the Stages of Penile Cancer and What They Mean
- Treatment Options: From Surgery to Chemotherapy
- How Penile Cancer Affects Fertility and Sexual Function
- Long-Term Outlook: Recurrence and Follow-Up Needs
- Causes and Risk Factors of Penile Cancer
- Recognizing the Symptoms Early
- Diagnostic Methods for Penile Cancer
- Staging the Disease: Understanding Progression
- Treatment Options for Penile Cancer
- Prognosis and Survival Rates
- Preventing Penile Cancer: What You Can Do
- Penile Cancer vs. Other Male Genital Cancers
- Emotional and Psychological Impact of Penile Cancer
- Reconstructive Surgery and Rehabilitation
- Advances in Penile Cancer Research
- Summary Table: Stages and Survival
- 15+ FAQ
What Is Penile Cancer and Why It Matters
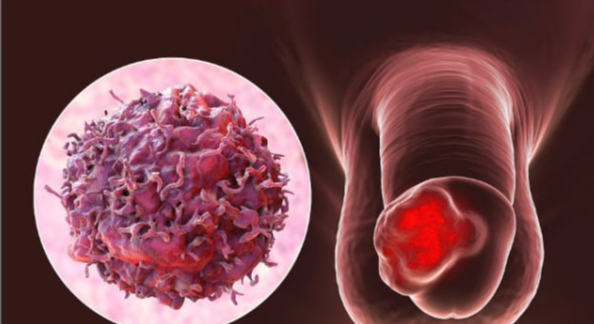
Penile cancer is a rare but serious type of cancer that begins in the skin or tissues of the penis. It usually starts in the squamous cells, the flat cells that make up most of the penile skin. Because the penis is part of both the urinary and reproductive systems, cancer in this area can have profound implications on both physical health and psychological well-being.
Early detection dramatically improves outcomes. Unfortunately, many cases go unnoticed until symptoms become severe. That’s why understanding how penile cancer presents itself, what increases the risk, and how it is treated is essential—especially for men over 50 or those with chronic infections like HPV.
Though uncommon in developed countries, penile cancer is more prevalent in regions with limited access to healthcare or poor hygiene practices. The disease can progress rapidly if untreated, making awareness and early medical consultation critical.
Recognizing the Early Signs and Symptoms of Penile Cancer
The most noticeable early signs often appear on the glans (tip of the penis) or the foreskin. Symptoms can be easily mistaken for other conditions like infections or inflammation, so timely evaluation by a urologist is key.
Common initial symptoms include:
- A sore or lump on the penis that doesn’t heal
- Foul-smelling discharge under the foreskin
- Skin thickening or color change
- Bleeding or ulceration
These signs may seem mild at first, but if persistent for more than two weeks, they should be examined. Pain is not always present in early stages, which contributes to delays in diagnosis.
Below is an overview of typical symptoms by stage:
| Stage | Common Symptoms |
| Early (in situ) | Red patch, minor irritation, slight skin change |
| Localized (Stage I) | Small growth, thickened skin, no lymph node changes |
| Advanced (Stage II+) | Larger mass, bleeding, discharge, lymph node swelling |
Key Causes and Risk Factors: Who Is Most at Risk?
Penile cancer is closely linked to lifestyle, infections, and hygiene. The strongest risk factor is infection with high-risk strains of human papillomavirus (HPV), particularly HPV-16 and HPV-18. Other significant contributors include smoking, poor penile hygiene, and having a foreskin that’s not regularly cleaned.
Circumcision in infancy has been shown to significantly reduce the risk of penile cancer, likely due to easier hygiene and reduced rates of HPV infection. However, adult circumcision does not offer the same level of protection once exposure has occurred.
Several risk elements are outlined in the table below:
| Risk Factor | Impact Level | Explanation |
| HPV Infection | High | Directly alters cellular DNA, increasing cancer risk |
| Smoking | High | Contains carcinogens that affect genital tissues |
| Phimosis (tight foreskin) | Moderate to High | Traps bacteria and irritants under foreskin |
| Poor Hygiene | Moderate | Encourages chronic infections and inflammation |
| Age Over 50 | Moderate | Risk increases with age |
Understanding these risks allows men to take preventive measures early, especially regarding HPV vaccination and smoking cessation.
How Penile Cancer Is Diagnosed: Tests and Clinical Approach
When penile cancer is suspected, doctors begin with a physical exam and thorough history. If a suspicious lesion is found, a biopsy is the gold standard for confirmation. This involves removing a small tissue sample for microscopic examination.
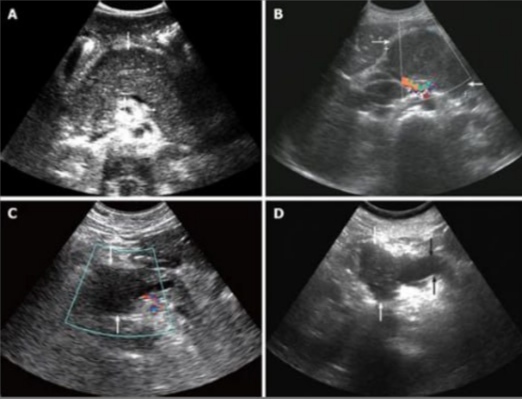
Once cancer is confirmed, staging tests are used to determine how far it has spread. These may include:
- Imaging (MRI, CT, or PET scans)
- Ultrasound of the groin to detect enlarged lymph nodes
- Blood tests to assess organ function and rule out metastasis
In cases where symptoms involve deeper tissue, a scan may be crucial. Interestingly, some patients undergo testing similar to what’s used in diagnosing prostate cancer, particularly in assessing lymph node involvement and pelvic spread.
Proper staging is vital to forming an effective treatment plan and predicting outcomes. Doctors typically use the TNM system, which classifies tumors by size (T), lymph node involvement (N), and distant spread (M).
Understanding the Stages of Penile Cancer and What They Mean
Penile cancer is staged using the internationally accepted TNM system—Tumor (T), Node (N), and Metastasis (M). These categories help determine how far the cancer has spread and inform treatment choices.
- Stage 0: Also called carcinoma in situ. Cancer cells are only in the top layer of skin.
- Stage I: The cancer has invaded the connective tissue but not yet spread to blood vessels or lymph nodes.
- Stage II: The tumor has invaded deeper tissues, possibly including the urethra or blood vessels.
- Stage III: Lymph nodes in the groin area are involved.
- Stage IV: Cancer has spread to distant parts of the body or deeply invaded nearby structures.
Here’s a simplified version of the staging in tabular format:
| Stage | Extent of Spread | Survival Outlook |
| Stage 0 | Localized to skin surface | Excellent with treatment |
| Stage I | Invades connective tissue | Very good |
| Stage II | Reaches deeper tissues or urethra | Fair to good |
| Stage III | Lymph nodes in groin involved | Depends on node involvement |
| Stage IV | Distant organs or extensive invasion | Poor |
Early stages often have curative outcomes, especially with surgery or localized therapy. In contrast, later stages may require systemic treatment and have a guarded prognosis.
Treatment Options: From Surgery to Chemotherapy

Treatment for penile cancer depends on the tumor’s size, location, and stage. The goal is always to remove or destroy the cancer while preserving as much function as possible.
Common treatments include:
- Surgical excision: The most frequent approach. In early-stage cancer, this may be a simple lesion removal. In more advanced cases, partial or total penectomy (removal of part or all of the penis) may be necessary.
- Laser therapy or topical chemotherapy: For carcinoma in situ or small superficial lesions.
- Lymphadenectomy: Removal of nearby lymph nodes when cancer has spread.
- Radiation therapy: Often used if surgery is not an option or to preserve appearance/function.
- Chemotherapy: Used when cancer is advanced or has spread. Drugs like cisplatin and 5-FU are common.
Multimodal treatment plans—such as combining surgery with radiation—may improve outcomes in later stages.
It’s important to note that systemic treatment strategies used in intermediate-risk prostate cancer have parallels here, especially regarding hormone suppression in advanced cases.
How Penile Cancer Affects Fertility and Sexual Function
One of the most difficult topics for patients is how penile cancer and its treatment will affect their sexual health. While treatments aim to preserve function whenever possible, some outcomes—especially in advanced stages—may involve surgical changes.
Key aspects impacted:
- Erectile function: May remain intact in early treatments but can be impaired by extensive surgery or radiation.
- Fertility: Often preserved unless chemotherapy or systemic radiation is involved.
- Body image and intimacy: Psychological effects are significant and require support from both clinicians and counselors.
Penile reconstruction surgeries exist and are continually improving. They use grafts or flaps to recreate a functional and aesthetic structure. Patients should ask about sexual rehabilitation resources early in the treatment process.
Long-Term Outlook: Recurrence and Follow-Up Needs
Follow-up care is essential, particularly because recurrence is most likely within the first two years after treatment. The nature of follow-up depends on the cancer’s stage and whether lymph nodes were involved.
Routine follow-up includes:
- Visual and physical exams of the penile area
- Groin lymph node assessments
- Imaging if recurrence is suspected
- Psychological support and counseling
Patients who have undergone lymph node removal or chemotherapy may also require long-term surveillance for side effects like lymphedema or cardiovascular toxicity.
Interestingly, recent studies show that patients who maintain good general wellness—including men’s health markers such as testosterone balance and metabolic control—have better post-treatment recovery.
Causes and Risk Factors of Penile Cancer
Penile cancer typically arises from a combination of environmental, behavioral, and biological factors. The leading cause is persistent infection with human papillomavirus (HPV), particularly HPV-16 and HPV-18 strains. These oncogenic viruses can integrate into penile epithelial cells and disrupt normal cell cycle regulation, increasing the risk of malignancy. Other infectious contributors include HIV, which further weakens immune surveillance.
Uncircumcised men face a higher risk due to the potential for smegma buildup under the foreskin, which may lead to chronic irritation and inflammation. Additionally, phimosis (inability to retract the foreskin) and poor genital hygiene have been associated with higher cancer incidence. Tobacco use, whether through smoking or chewing, introduces carcinogens that affect penile tissues and significantly raise risk.
In rare cases, men with a history of lichen sclerosus — a chronic inflammatory condition of the skin — may also have an elevated susceptibility. There’s ongoing research into genetic predisposition, though most cases are linked to acquired rather than inherited traits. Factors such as low socioeconomic status and reduced access to healthcare may delay diagnosis and indirectly contribute to poorer outcomes.
Recognizing the Symptoms Early
Early detection of penile cancer improves survival and minimizes the need for aggressive treatment. Most early signs manifest on the glans or foreskin. Common symptoms include a lump, ulcer, or sore that does not heal. These lesions might bleed, produce discharge, or become tender over time. A wart-like growth or a persistent area of thickened skin may also raise concern.
Changes in skin coloration, such as redness or bluish discoloration, are occasionally overlooked but can be early warning indicators. Some men report foul-smelling discharge, especially if secondary infection sets in. Swelling of the foreskin or painful urination could also suggest disease progression.
Swollen lymph nodes in the groin, while more often associated with infection, should be carefully evaluated, especially when persistent or firm. The importance of recognizing subtle or atypical signs is crucial, as patients may delay seeking help due to embarrassment or lack of awareness — especially regarding male-specific cancers. Educational campaigns in men’s health aim to improve awareness and encourage timely evaluation.
Diagnostic Methods for Penile Cancer
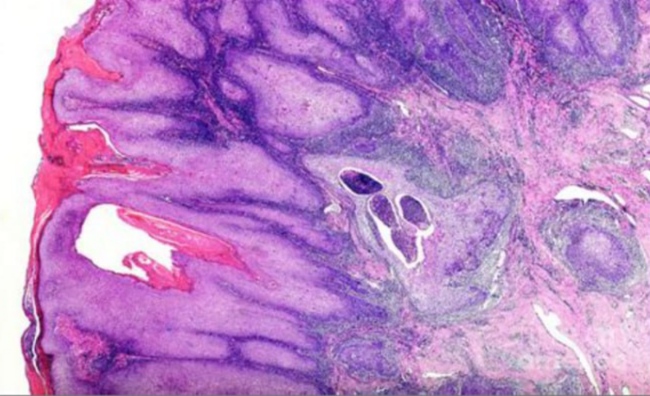
The diagnostic process begins with a thorough clinical examination, including inspection and palpation of the penis and inguinal lymph nodes. If a suspicious lesion is present, a biopsy is essential. Incisional or punch biopsy is commonly used for small lesions, while excisional biopsy may be considered for localized growths.
Histopathological evaluation determines the presence of squamous cell carcinoma — the most prevalent subtype — and assesses factors such as depth of invasion, grade, and lymphovascular involvement. Imaging plays a vital role in staging. Ultrasound with Doppler is often used to assess tumor infiltration, especially in corpora cavernosa. MRI offers more detailed soft tissue evaluation and is preferred for complex cases.
To detect possible spread, a CT scan or PET-CT may be conducted to assess lymph node involvement or distant metastasis. In select cases, a sentinel lymph node biopsy is recommended to detect micrometastases even in clinically normal groin nodes.
Laboratory workup typically includes complete blood count, renal function, and possibly HPV genotyping. Importantly, penile cancer diagnosis may overlap with other genitourinary cancers. Coordination with urologic oncologists ensures accurate staging and treatment planning.
Staging the Disease: Understanding Progression
Staging of penile cancer follows the TNM system, which classifies tumors based on:
| Stage | Tumor (T) Description | Nodal Status (N) | Metastasis (M) |
| Stage 0 | Carcinoma in situ | N0 | M0 |
| Stage I | Tumor invades subepithelial tissue | N0 | M0 |
| Stage II | Tumor invades corpus spongiosum/cavernosum | N0 or N1 | M0 |
| Stage III | Any T + N2 or fixed lymph nodes | N2 | M0 |
| Stage IV | Any T + N3 or distant spread | Any N | M1 |
This framework is crucial for both prognosis and treatment selection. Early-stage penile cancer (Stage 0 or I) may be amenable to organ-sparing treatments. As the disease progresses, lymph node involvement becomes a dominant prognostic factor. Bilateral inguinal metastasis (N2/N3) significantly reduces long-term survival.
Advanced stages may include spread to pelvic lymph nodes or distant sites such as lungs, liver, or bones. Metastatic disease is rare but carries a grim prognosis. Staging must be reassessed after initial therapy to determine treatment response and inform further interventions.
Penile cancer staging also shares principles with other urological cancers like Prostate Cancer — particularly when evaluating nodal and distant spread. Recognizing patterns of progression across male-specific malignancies enhances interdisciplinary care.
Treatment Options for Penile Cancer
Treatment for penile cancer depends heavily on the stage, grade, and exact location of the tumor. For early-stage cancers (such as carcinoma in situ or Stage I), organ-sparing techniques are often prioritized. Topical chemotherapy (e.g., 5-fluorouracil or imiquimod) can be effective in situ cases. Laser ablation or Mohs micrographic surgery is sometimes used for superficial lesions with minimal invasion.
For more advanced cases, partial or total penectomy may be necessary. While psychologically and functionally significant, penectomy provides the highest chance of long-term survival in locally advanced tumors. Surgeons aim to preserve as much of the penis as possible while ensuring complete tumor removal.
Inguinal lymph node dissection is typically required if nodes are involved. Minimally invasive laparoscopic techniques are emerging in this area, reducing complications. Radiation therapy may be employed postoperatively or as primary treatment when surgery isn’t feasible.
Chemotherapy regimens, such as cisplatin-based combinations, are usually reserved for node-positive or metastatic disease. Immunotherapy is currently being studied in clinical trials, especially in HPV-related penile cancers. Treatment is often multidisciplinary, involving urology, oncology, radiology, and sometimes plastic surgery for reconstruction.
Prognosis and Survival Rates
Penile cancer outcomes depend primarily on early detection and lymph node involvement. Patients diagnosed with localized disease have excellent five-year survival rates — often over 85%. However, survival drops significantly once the cancer spreads to regional nodes (about 50–60%) or distant organs (below 30%).
Prognostic factors include:
- Tumor size and depth of invasion
- Histologic grade (well vs poorly differentiated)
- Presence of lymphovascular invasion
- Lymph node involvement
- Perineural invasion
In recent years, earlier diagnosis and improved surgical techniques have helped improve overall survival. Awareness of male cancers through broader Men’s Health campaigns also plays a role in encouraging earlier check-ups.
Prognosis is also impacted by patient factors like age, comorbidities, and immune status (particularly in HIV-positive individuals). High-grade tumors with extensive invasion tend to progress rapidly, underscoring the importance of vigilant follow-up even after successful treatment.
Preventing Penile Cancer: What You Can Do
Although penile cancer is relatively rare, many of its causes are preventable. The most important protective measure is HPV vaccination, which significantly reduces the risk of high-risk HPV strains known to cause genital cancers. While traditionally offered to females, HPV vaccines are now recommended for males up to age 26 (and sometimes beyond).
Circumcision in infancy has been shown to lower risk, but adult circumcision is not widely adopted as a preventive measure. Good hygiene — especially for uncircumcised men — remains essential. Gently retracting and cleaning under the foreskin daily helps prevent smegma buildup and chronic inflammation.
Smoking cessation is another critical preventive step. Tobacco’s carcinogenic compounds directly affect the skin of the genitals and may impair immune defense against HPV infections.
Regular self-examination and prompt medical attention for any genital skin changes are also key. Public health efforts should focus on early education, especially in at-risk populations with limited healthcare access.
Penile Cancer vs. Other Male Genital Cancers
Penile cancer must be distinguished from other malignancies that affect male reproductive organs, particularly testicular and prostate cancer. Each has a unique origin, risk profile, and progression rate. However, symptoms may overlap — particularly in advanced stages.
Unlike testicular cancer, which affects younger men and often presents as painless swelling, penile cancer typically affects older males and begins with visible lesions on the glans or foreskin. In contrast, prostate cancer may develop silently and only present later with urinary or skeletal symptoms.
Penile cancer also carries unique psychological burdens due to its visible location and implications for sexual identity. It shares staging and nodal spread patterns with Biochemical Relapse in Prostate Cancer , particularly in how groin and pelvic nodes are evaluated and managed.
Multidisciplinary awareness helps ensure accurate diagnosis and avoids misclassification. Many men delay seeking care for genital symptoms, assuming they are benign — which underscores the need for clearer differentiation and routine male health screening.
Emotional and Psychological Impact of Penile Cancer
The diagnosis of penile cancer brings unique psychological challenges. Because the penis is not only a functional organ but also tied closely to identity, intimacy, and masculinity, many men experience anxiety, depression, shame, or even PTSD after diagnosis or surgery.
Those who undergo partial or total penectomy may face changes in sexual function and body image. These can affect relationships and quality of life, especially if patients feel stigmatized or isolated. Open communication with partners and access to counseling are vital. Peer support groups, often found through cancer centers or online, provide validation and coping strategies.
Psychosexual therapy may be beneficial for couples navigating intimacy changes. The emotional dimension of penile cancer is sometimes under-addressed in clinical care, yet it’s just as critical to recovery as physical treatment. Survivorship plans should include mental health evaluation and referral when appropriate.
Reconstructive Surgery and Rehabilitation
For patients requiring partial or total penectomy, reconstructive options may be available. Phalloplasty, though complex, can help restore genital form and function, including the possibility of urinary diversion and sexual sensation using nerve grafts.
Tissue may be taken from the forearm, thigh, or abdomen to construct a neophallus. While these procedures are not available everywhere and can be expensive, they represent a lifeline for those seeking restoration of dignity and sexual identity.
Rehabilitation may also involve learning new ways of achieving sexual intimacy, using assistive devices, or psychological adaptation. Early involvement of a reconstructive urologist, physical therapist, and psychosexual counselor is ideal for those considering this path.
Advances in Penile Cancer Research
Ongoing studies are exploring molecular markers, targeted therapies, and HPV-related oncogenesis in penile cancer. Researchers are examining why certain HPV strains lead to malignancy in some men but not others, and whether immune-modulating drugs may offer benefit.
Clinical trials involving checkpoint inhibitors (used in other squamous cell cancers) are underway. Genetic studies are also being conducted to uncover familial risks and identify populations who may benefit from early surveillance.
Some data even draw parallels with prostate cancer — including the potential crossover relevance of studies on Prostate Cancer to better understand androgen-related pathways. As penile cancer research expands, outcomes may improve through personalized medicine.
Summary Table: Stages and Survival
Below is a simplified overview of penile cancer stages and estimated 5-year survival rates:
| Stage | Description | Estimated 5-Year Survival |
| Stage 0 (Carcinoma in situ) | Limited to surface skin cells | 90–95% |
| Stage I | Tumor invades connective tissue, no spread | 80–85% |
| Stage II | Invades deeper structures or blood vessels | 65–75% |
| Stage III | Spread to nearby lymph nodes | 40–60% |
| Stage IV | Distant spread (metastatic) | <30% |
Early detection clearly makes a critical difference in survival and quality of life.
15+ FAQ
1. What does penile cancer look like in early stages?
It often appears as a red patch, sore, wart-like growth, or ulcer on the glans, shaft, or foreskin. These changes can be mistaken for benign skin conditions but usually don’t heal.
2. Is penile cancer always caused by HPV?
Not always, but high-risk HPV types, especially HPV-16, are implicated in about half of cases. Other causes include poor hygiene and smoking.
3. Can circumcision prevent penile cancer?
Infant circumcision has been shown to reduce lifetime risk. However, adult circumcision as prevention isn’t universally recommended unless medically necessary.
4. Does penile cancer spread quickly?
It can, especially high-grade tumors. Lymph node involvement accelerates spread. Early detection is key to preventing metastasis.
5. Can penile cancer be cured?
Yes — especially when detected early. Organ-sparing treatments or surgery can often achieve a cure.
6. How painful is penile cancer treatment?
Discomfort varies. Topical treatments cause mild irritation. Surgery may involve recovery pain, but pain management is standard in care plans.
7. Are there non-surgical treatment options?
For superficial or early-stage cases, topical chemotherapy and laser therapy can be effective. Radiation is used in select cases.
8. Can it come back after treatment?
Recurrence is possible, especially if lymph nodes weren’t treated early. Regular follow-up is essential.
9. Can men still have sex after treatment?
Yes, though it may be different. Many men adapt with support. Counseling can help navigate emotional and physical changes.
10. Is it contagious?
No — cancer itself isn’t contagious. However, HPV, a contributing factor, is sexually transmissible.
11. How common is penile cancer?
It’s rare in the U.S., accounting for less than 1% of male cancers. However, incidence is higher in some countries with limited HPV vaccination or healthcare access.
12. Is there a genetic link to penile cancer?
There’s limited evidence of a strong hereditary component, but immune or skin disorders may raise risk.
13. Does HIV increase the risk?
Yes, because of immune suppression. HIV-positive men have higher rates of HPV infection and related cancers.
14. Can I request HPV vaccination as an adult?
Yes — men up to age 45 may request vaccination, especially if at higher risk. It’s most effective before sexual activity begins.
15. Should I be worried if I find a lump?
Any persistent genital lump should be evaluated by a doctor — it may be benign, but early examination prevents complications.











