Pancreatic Cancer Ultrasound
Pancreatic Cancer Ultrasound: A Complete Guide
- What Is Pancreatic Cancer Ultrasound and How Is It Done?
- Why Ultrasound Is Often the First Imaging Choice
- Transabdominal Ultrasound: Strengths and Limitations
- Endoscopic Ultrasound (EUS): A More Advanced Tool
- How Pancreatic Tumors Appear on Ultrasound Scans
- What Happens If Ultrasound Detects a Suspicious Mass?
- Ultrasound’s Role in Staging Pancreatic Cancer
- When Ultrasound Alone Isn’t Enough
- Comparison: Ultrasound vs CT, MRI, and PET in Pancreatic Cancer
- Using Ultrasound to Monitor Treatment Response
- Risks and Misinterpretations with Pancreatic Ultrasound
- Patient Example: From Abdominal Pain to Early Diagnosis via Ultrasound
- Advancements in Ultrasound Technology for Pancreatic Imaging
- Challenges in Rural and Low-Resource Settings
- How Ultrasound Fits into Overall Pancreatic Cancer Care
- Key Takeaways: What Patients Should Know
- 15+ Frequently Asked Questions
What Is Pancreatic Cancer Ultrasound and How Is It Done?
A pancreatic cancer ultrasound uses sound waves to create images of your pancreas and surrounding structures. It is a non-invasive, safe, and affordable diagnostic tool commonly used as the first imaging test when pancreatic symptoms arise. Two main approaches exist: transabdominal ultrasound and endoscopic ultrasound (EUS). Transabdominal scans are performed through the abdomen, while EUS involves inserting a thin probe through the stomach or small intestine for high-resolution imaging of the pancreas.
Both methods help detect abnormalities such as masses, cysts, or duct dilations. EUS also allows guided biopsy of suspicious lesions, which is invaluable for definitive diagnosis.
Why Ultrasound Is Often the First Imaging Choice
Ultrasound is frequently chosen early in the diagnostic process due to its many benefits:
- Accessibility and Cost
Widely available in clinics and hospitals, ultrasound is less expensive than CT or MRI scanning. - Safety Profile
No radiation exposure makes it suitable for frequent monitoring or use in sensitive populations. - Real-Time Imaging
Physicians can assess blood flow using Doppler ultrasound and visualize dynamic organ function such as dilation of bile ducts.
While not as detailed as CT scans or MRIs, ultrasound often reveals signs warranting further investigation, such as a solid mass or dilated pancreatic duct, both red flags for pancreatic cancer detection.
Transabdominal Ultrasound: Strengths and Limitations
Transabdominal ultrasound is the most common type, but it has pros and cons:
Pros:
- Quick and painless
- Readily available
- No radiation exposure
Cons:
- Limited sensitivity for small tumors (<2 cm)
- Challenged by patient attributes (e.g., obesity, gas in intestines)
- Cannot perform biopsies
Because pancreatic cancers are often small and deep-seated, abnormalities may be missed. However, obvious masses and duct abnormalities are readily visualized, making ultrasound a valuable starting point—though often followed by CT, MRI, or NanoKnife pancreatic cancer treatment evaluations.
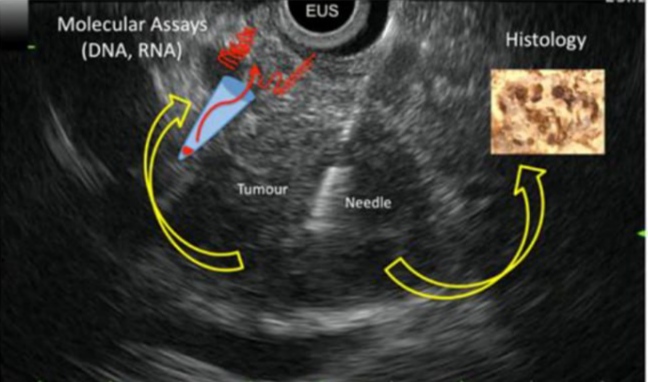
Endoscopic Ultrasound (EUS): A More Advanced Tool
Endoscopic ultrasound delivers high-resolution images and enables biopsy:
- A thin, flexible tube with an ultrasound probe is inserted via mouth
- The probe directly contacts stomach or duodenum wall, providing clear pancreaticobiliary images
- Allows fine‑needle aspiration (FNA) to collect tissue for cancer diagnosis
EUS is more invasive, requiring sedation, but it delivers better tumor characterization and staging. It’s crucial when transabdominal scans are inconclusive but symptoms continue, such as persistent abdominal pain, unexplained weight loss, or onset of diabetes.
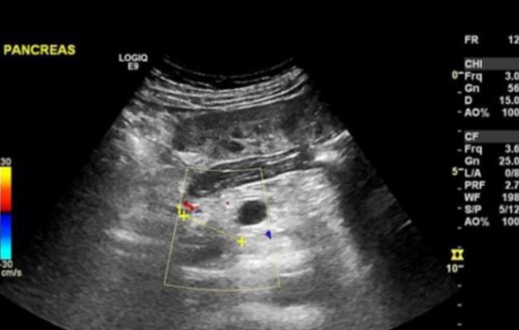
How Pancreatic Tumors Appear on Ultrasound Scans
Pancreatic tumors can show up in several ways on an ultrasound, depending on their size, type, and location. Solid tumors typically appear as hypoechoic (darker) areas compared to the surrounding tissue. In some cases, they may also disrupt the smooth architecture of the pancreas or cause indirect signs like a blocked bile duct or dilated pancreatic duct.
Common ultrasound features of pancreatic tumors include:
| Feature | Description |
| Hypoechoic mass | Darker, irregular area on the pancreas |
| Pancreatic duct dilation | Often greater than 3 mm—may indicate tumor blockage |
| Double duct sign | Both bile and pancreatic ducts appear dilated |
| Loss of normal pancreatic shape | Blurred or deformed margins of the pancreas |
Endoscopic ultrasound enhances the visibility of these findings. Smaller or early-stage tumors may be completely missed on transabdominal ultrasound but are more reliably detected via EUS.
What Happens If Ultrasound Detects a Suspicious Mass?
If your ultrasound reveals a potential mass or abnormal duct changes, further investigation is essential. You may be referred for:
- CT or MRI Scans: These provide more detail and help confirm the findings.
- EUS-Guided Biopsy: A sample of the mass is collected for histopathology.
- Blood Tests: CA 19-9 and liver function tests are commonly ordered.
Ultrasound can raise suspicion but cannot definitively diagnose cancer alone. That’s why combining imaging techniques is often necessary, especially for determining cancer stage and operability.
It’s worth noting that some patients first undergo colonoscopy for unrelated gastrointestinal symptoms, and suspicious findings there may lead to abdominal ultrasound or CT.
Ultrasound’s Role in Staging Pancreatic Cancer
Staging determines how far the cancer has spread and influences treatment decisions. While ultrasound is not the gold standard for staging, endoscopic ultrasound is particularly useful in assessing:
- Tumor size and local invasion
- Involvement of nearby lymph nodes
- Relationship to blood vessels (e.g., portal vein, superior mesenteric artery)
These details help determine whether the tumor is resectable (surgically removable) or needs neoadjuvant therapy first. In certain settings, EUS can be as effective as CT scans in local staging—especially for early tumors not yet visible via external imaging.
When Ultrasound Alone Isn’t Enough
There are many cases where ultrasound is not sufficient:
- Obese patients or those with excess bowel gas
- Tumors smaller than 2 cm
- Tumors located in the tail of the pancreas
- Patients with anatomical distortions or previous surgeries
In these situations, CT, MRI, or PET scans are essential to complete the evaluation. Endoscopic ultrasound, while superior for close-range imaging, also requires specialized equipment and expertise, making it less accessible in smaller hospitals.
Moreover, patients being monitored for recurrence or undergoing evaluation for pancreatic cancer treatments like surgery, chemotherapy, or NanoKnife ablation often rely more heavily on CT/MRI than ultrasound.
Comparison: Ultrasound vs CT, MRI, and PET in Pancreatic Cancer
When assessing pancreatic cancer, various imaging methods have specific strengths. Here’s how ultrasound compares with the most commonly used alternatives:
| Imaging Modality | Strengths | Limitations |
| Ultrasound | Quick, accessible, non-invasive, no radiation | Lower resolution, limited by anatomy, less accurate for small lesions |
| CT Scan | Excellent for staging, vascular involvement, and metastasis | Radiation exposure; may miss small or isoattenuating tumors |
| MRI | Superior for soft tissue contrast, helpful in surgical planning | Longer duration, expensive, less available in some settings |
| PET Scan | Functional imaging; detects metabolic activity, ideal for distant spread | Not used for initial diagnosis, expensive, low specificity sometimes |
Ultrasound is frequently the first step, but follow-up with more detailed imaging is almost always needed to complete diagnosis and treatment planning.
Using Ultrasound to Monitor Treatment Response
After diagnosis, ultrasound can serve a supportive role in monitoring how pancreatic tumors respond to treatment, particularly in the liver and peritoneum. While CT remains the standard for most follow-ups, ultrasound can be used to:
- Track reduction in size of liver metastases
- Evaluate resolution of obstructed bile ducts post-stenting
- Guide fluid drainage in case of ascites or infection
However, keep in mind that subtle changes in tumor biology—like changes in metabolic activity—require PET or MRI for accurate interpretation.
Risks and Misinterpretations with Pancreatic Ultrasound
While ultrasound is safe, there are risks of false positives and false negatives:
- False positives can occur with cysts, benign lesions, or pancreatitis that mimic cancer.
- False negatives happen especially with tumors in the tail, those under 2 cm, or in patients with excessive intestinal gas.
Misinterpretations may delay diagnosis, especially when subtle ductal dilation is dismissed. This is why a multidisciplinary approach combining radiology, oncology, and gastroenterology is essential.
Ultrasound findings must always be correlated with blood work and other imaging before moving forward with a treatment plan.
Patient Example: From Abdominal Pain to Early Diagnosis via Ultrasound
A 61-year-old man presents with vague upper abdominal pain and weight loss. His primary care provider orders a transabdominal ultrasound, which shows a hypoechoic lesion in the head of the pancreas and a dilated bile duct. He’s immediately referred to a gastroenterologist for endoscopic ultrasound and biopsy.
Histology confirms early-stage pancreatic adenocarcinoma. Because the tumor hasn’t encased major vessels and there are no metastases, the patient undergoes Whipple surgery with adjuvant chemotherapy.
In this case, timely ultrasound screening led to early intervention and better outcomes—a rare but critical success story in pancreatic cancer management.
Advancements in Ultrasound Technology for Pancreatic Imaging
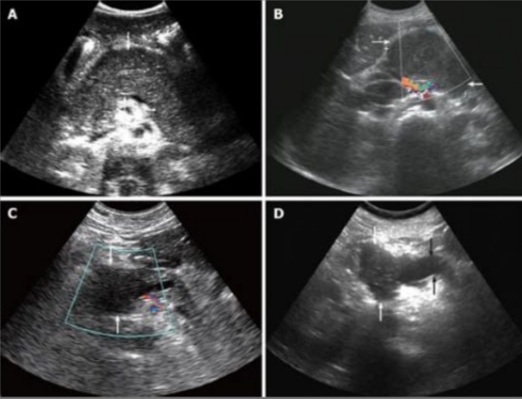
Modern ultrasound systems have significantly improved pancreatic cancer detection. Key advancements include:
- Contrast-Enhanced Ultrasound (CEUS): Helps differentiate between malignant and benign lesions by analyzing how microbubbles move through vessels in real time.
- Elastography: Measures tissue stiffness—cancerous tissue tends to be stiffer than normal pancreatic tissue.
- High-Frequency Probes: Provide better resolution for superficial pancreatic structures, especially in endoscopic use.
- 3D Ultrasound and AI-based Image Processing: Early research shows that combining 3D imaging with artificial intelligence may improve detection rates and reduce operator error.
These innovations are still being evaluated but represent a promising future for non-invasive cancer imaging.
Challenges in Rural and Low-Resource Settings
In rural or underserved healthcare environments, ultrasound is often the only imaging modality available. This leads to specific issues:
- Limited access to trained sonographers and radiologists
- Lack of high-end ultrasound equipment
- Absence of complementary imaging like CT or MRI
- Delays in biopsy due to referral bottlenecks
Despite these challenges, ultrasound remains valuable in triaging suspected pancreatic cases, identifying obstructive jaundice, or guiding drainage procedures in patients who cannot travel for advanced imaging.
How Ultrasound Fits into Overall Pancreatic Cancer Care
Ultrasound plays a role across multiple stages:
- Detection: Often incidental, or first-line in jaundice cases
- Diagnosis: Helps guide more precise biopsies through endoscopic ultrasound
- Staging: Limited, but helpful with liver metastases or ascites
- Monitoring: Tracks changes post-intervention or palliative procedures
While it cannot replace CT or PET in staging or surgical planning, ultrasound is an essential, low-risk, repeatable tool in the full spectrum of pancreatic cancer care.
Key Takeaways: What Patients Should Know

- Ultrasound is useful but not definitive for diagnosing pancreatic cancer.
- If a pancreatic lesion is detected, expect follow-up imaging and biopsy.
- Endoscopic ultrasound (EUS) is superior to external ultrasound for small or deep tumors.
- Always ask whether additional tests are needed to confirm or rule out a diagnosis.
- Early detection with ultrasound can be life-saving—especially if followed by fast-track referrals.
For broader context, if you’re interested in high-precision techniques like NanoKnife ablation, or whether a colonoscopy can detect pancreatic cancer, explore those linked topics to understand the full range of diagnostic tools.
15+ Frequently Asked Questions
1. Can an ultrasound detect early-stage pancreatic cancer?
From my research, ultrasound can detect some early-stage tumors, but small or deeply located ones are often missed. That’s why EUS or CT is typically used to confirm findings.
2. How reliable is ultrasound compared to CT or MRI?
Ultrasound is less reliable overall. It’s a good starting point, especially for obvious abnormalities, but CT or MRI provide more detailed views.
3. What symptoms would lead a doctor to order an ultrasound?
Unexplained abdominal pain, jaundice, weight loss, or a family history of pancreatic issues often trigger an ultrasound request.
4. Can you use ultrasound if you already had abdominal surgery?
Yes, but scar tissue or altered anatomy might make the pancreas harder to visualize clearly.
5. Is a normal ultrasound enough to rule out pancreatic cancer?
No. A normal scan doesn’t eliminate the possibility—especially in high-risk patients. Further testing is usually recommended.
6. How fast should I act after an abnormal ultrasound?
Immediately. If the ultrasound shows a mass or duct dilation, quick referral for biopsy or advanced imaging is critical.
7. What’s the role of ultrasound in palliative care?
It helps guide procedures like fluid drainage or stent placement and monitors treatment response in comfort care plans.
8. Does ultrasound expose me to radiation?
Not at all. That’s one of its main advantages, particularly for repeated use.
9. Why can’t ultrasound always see the pancreas well?
The pancreas lies deep behind the stomach and intestines, which can obstruct sound waves—especially in obese patients or those with gas.
10. What’s the best test if ultrasound is inconclusive?
CT is usually the next step, followed by MRI or EUS depending on the situation.
11. Can ultrasound detect spread to the liver?
Yes, it can see metastases in the liver, especially if they’re large or numerous.
12. Is EUS painful?
Endoscopic ultrasound involves sedation and a thin scope—it’s well-tolerated and much more accurate for pancreas exams.
13. Can an ultrasound help detect other conditions besides cancer?
Yes—like pancreatitis, cysts, gallstones, or bile duct blockages. It’s a versatile diagnostic tool.
14. How often should high-risk patients get scanned?
It depends on personal risk factors, but many guidelines recommend yearly imaging—often with MRI or EUS rather than just ultrasound.
15. What’s the most important thing to remember about ultrasound and pancreatic cancer?
It’s a helpful first step, but never the only step. Follow-up with a specialist is always necessary if there’s any concern.











