How to Prevent Bone Cancer
How to Prevent Bone Cancer: The Ultimate Guide
- What It Is and Why Prevention Matters
- The Role of Genetics and Family History
- Environmental Factors and Radiation Exposure
- Diet and Nutritional Strategies to Support Bone Health
- Physical Activity and Bone Strength: The Connection
- Monitoring for Early Warning Signs
- Chemical and Occupational Exposure: Mitigating Workplace Risks
- The Link Between Bone Injury and Cancer Development
- Hormonal Influence and Bone Tumor Risk
- Immunity, Inflammation, and the Cancer Connection
- Diagnostic Imaging for Early Surveillance
- Preventive Screenings and Long-Term Monitoring Plans
- Understanding the Role of Genetics in Bone Cancer Risk
- Dietary Strategies to Support Bone Integrity
- Lifestyle Adjustments That Reduce Overall Cancer Risk
- Summary: A Holistic Blueprint for Bone Cancer Prevention
- 15+ Frequently Asked Questions (FAQ)
What It Is and Why Prevention Matters

Bone cancer is a rare but serious condition in which malignant cells grow uncontrollably within the bone tissue. It can originate directly in the bone (primary bone cancer), or it can result from metastasis, where cancer from another organ spreads to the bone. While not all causes are preventable—especially in inherited or pediatric forms—there are meaningful lifestyle and environmental factors that can reduce the overall risk.
The most common types of bone cancer include:
| Type of Bone Cancer | Common Sites | Typical Age Group |
| Osteosarcoma | Arms, legs, pelvis | Teens, young adults |
| Ewing Sarcoma | Spine, ribs, pelvis | Children, teens |
| Chondrosarcoma | Pelvis, shoulders | Adults over 40 |
| Secondary (Metastatic) | Spine, hips, long bones | Over 50, with other cancer history |
Prevention becomes especially important for those with a family history of cancer, past radiation exposure, or pre-existing bone conditions.
The Role of Genetics and Family History
Genetic mutations account for a portion of bone cancer cases, particularly in younger populations. Inherited conditions such as Li-Fraumeni syndrome, Rothmund-Thomson syndrome, or hereditary retinoblastoma increase susceptibility.
People with a family history of bone cancer should consider:
- Speaking to a genetic counselor
- Undergoing periodic imaging, such as X-rays or MRIs
- Proactive screening for known cancer-related mutations
While you cannot change your genes, you can take steps to monitor your risk and act quickly if early signs appear. In veterinary oncology, for example, recognizing patterns in breeds helps veterinarians understand Bone Cancer in Dogs and detect it early — and the same principle applies to humans.
Environmental Factors and Radiation Exposure
Radiation therapy, especially for other types of childhood cancer, is one of the most well-documented risk factors for bone malignancies later in life. The higher the dose and the younger the age during exposure, the greater the risk.
Ionizing radiation from environmental sources (e.g., nuclear accidents, occupational exposure) also contributes to risk. While less common today, patients who received radiation decades ago for acne, scoliosis, or tuberculosis should be monitored closely.
| Exposure Source | Risk Level | Recommendation |
| Past radiation therapy | High | Annual orthopedic follow-up |
| Occupational (nuclear) | Moderate | Wear dosimeter; regular scans |
| Diagnostic X-rays | Low | Use only when clinically necessary |
| CT scans (repeated) | Moderate | Use with caution; explore MRI if viable |
Protective protocols in hospitals today minimize exposure, but awareness remains key in long-term monitoring.
Diet and Nutritional Strategies to Support Bone Health
A nutrient-rich diet that supports bone density may not directly prevent bone cancer, but it helps maintain skeletal strength and resilience. This creates an environment less vulnerable to cell damage or abnormal growth. Crucial dietary elements include:
- Calcium: Strengthens bone matrix
- Vitamin D: Aids in calcium absorption
- Magnesium & Phosphorus: Essential for bone structure
- Antioxidants: Neutralize free radicals, reducing cellular damage
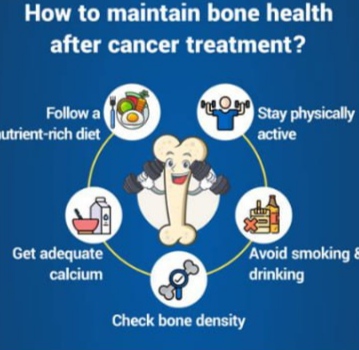
Infographic: Foods That Support Bone Integrity
(Include visual showing leafy greens, dairy, fortified cereals, oily fish, nuts, and eggs)
Moreover, ensuring a balanced intake of anti-inflammatory nutrients may reduce chronic irritation in bone tissue — a possible precursor to malignancy in some theories.
Physical Activity and Bone Strength: The Connection
Regular physical activity is essential for maintaining bone mass and reducing the risk of skeletal deterioration. While exercise doesn’t directly prevent cancerous mutations, it enhances structural resilience and improves the immune system’s efficiency in eliminating damaged cells.
Weight-bearing activities such as walking, resistance training, and yoga stimulate osteoblast activity (bone-building cells), preserving bone density — a factor critical for aging individuals.
People with sedentary lifestyles tend to lose bone mass earlier, which may lead to complications like fractures and chronic inflammation. These, in turn, could increase cellular turnover in bones, creating an environment vulnerable to mutations over time.
For comparison, just like in Bone Cancer in Cats, where reduced activity can be an early warning sign, inactivity in humans may also mask underlying bone degeneration or cancer risk.
Monitoring for Early Warning Signs

Early detection is the single most effective method of improving outcomes in bone cancer cases. Many symptoms are initially subtle and can be mistaken for sports injuries or arthritis.
Common early indicators include:
- Persistent bone pain, especially at night
- Swelling or a noticeable lump
- Fractures from minimal trauma
- Reduced range of motion in joints
While these signs don’t automatically mean cancer, they warrant attention if they persist longer than a few weeks. Diagnostic tools such as bone scans and MRIs should be prioritized over standard X-rays when deeper lesions are suspected.
A Bone Density Test, typically used for osteoporosis, may not detect cancer directly. However, changes in bone mineral density could indicate structural abnormalities worth investigating. This is particularly important in understanding whether a Bone Density Test Can Detect Cancer indirectly by flagging red flags.
Chemical and Occupational Exposure: Mitigating Workplace Risks
Exposure to certain chemicals and toxins may increase the likelihood of cellular mutations in bones. Industrial workers, agricultural employees, and those in chemical processing may face higher risks.
| Chemical/Toxin | Linked Concern | Protective Measure |
| Benzene | Bone marrow toxicity | Ventilation, PPE, blood tests |
| Vinyl chloride | Sarcoma risk | Respirators, exposure limits |
| Chromium compounds | DNA damage potential | Protective gloves, periodic scans |
| Asbestos | Indirect inflammation | Avoidance, sealed environments |
Employers must enforce OSHA standards, but individuals can advocate for their own health by requesting regular blood panels and occupational health assessments.
The Link Between Bone Injury and Cancer Development
Though rare, there is ongoing debate about whether repeated trauma or fractures can contribute to bone cancer formation. While a direct link is not conclusively proven, chronic inflammation in a healing bone environment may increase mutation risk, especially in genetically predisposed individuals.
For example, if a fracture heals abnormally and new tissue growth is excessive or misdirected, it could — under specific conditions — trigger abnormal cell behavior.
Chondrosarcoma and osteosarcoma cases have been documented near long-healed injury sites, though causation remains speculative.
Infographic: Timeline of Injury to Tumor (Illustrative)
- Initial bone trauma → prolonged healing → persistent swelling → cellular instability → neoplastic change (in rare cases)
Hormonal Influence and Bone Tumor Risk
Hormonal balance plays a critical role in overall bone health, especially during puberty, pregnancy, menopause, or endocrine disorders. Estrogen and testosterone regulate bone remodeling, and their deficiency or excess can indirectly affect the cellular environment of bones.
In postmenopausal women, low estrogen levels contribute to decreased bone density, which increases the need for surveillance. Hormone therapy, especially when combined with prior radiation or chemotherapy, may also raise concerns about tumorigenesis.
Growth hormones used in childhood or puberty (either naturally or via treatment) have also been examined for links to bone overgrowth syndromes, some of which carry malignancy risks.
While research is ongoing, maintaining hormonal balance through nutrition, stress management, and endocrinological check-ups is a proactive strategy in long-term bone cancer prevention.
Immunity, Inflammation, and the Cancer Connection
The immune system plays a crucial role in identifying and eliminating early abnormal cells before they become malignant. Chronic inflammation, however, weakens this defense and may promote a microenvironment that fosters cancer development.
Inflammatory bone diseases like osteomyelitis or autoimmune conditions such as lupus and rheumatoid arthritis have been associated with higher cancer risks. This may be due to persistent immune activation and cell turnover.
| Factor | Impact on Bone Health | Recommendation |
| Autoimmune diseases | Chronic inflammation | Immunomodulatory therapy |
| Poor gut health (dysbiosis) | Reduced nutrient uptake | Probiotics, anti-inflammatory diet |
| Persistent infections | Delayed tissue recovery | Timely antibiotic use |
Individuals with a history of such conditions should work closely with rheumatologists and oncologists to maintain a balanced immune profile and reduce their cancer vulnerability.
Diagnostic Imaging for Early Surveillance
For those with high risk — due to family history, genetic conditions, or occupational exposure — periodic imaging is a key part of cancer prevention. Detecting subtle changes in bone structure can prompt early biopsies or interventions.
Diagnostic tools for bone health include:
| Imaging Type | Best Use Case | Radiation Exposure |
| X-ray | Structural changes and obvious fractures | Low |
| MRI | Soft tissue and marrow abnormalities | None |
| CT Scan | Deep bone and complex lesions | Moderate |
| PET Scan | Metabolic activity in suspected tumors | High |
MRI is especially valuable for its lack of radiation and clarity in detecting early bone marrow changes. PET scans, although more invasive, are often used when cancer is suspected to have spread.
Preventive Screenings and Long-Term Monitoring Plans
Preventive screening isn’t standard for bone cancer due to its rarity, but those at elevated risk can work with physicians to build personalized monitoring plans. These plans typically involve:
- Annual physical exams focused on musculoskeletal health
- Periodic imaging depending on age and risk profile
- Genetic screening if inherited syndromes are suspected
- Bone density evaluations every 2–3 years after age 50
Preventive strategies also include lifestyle coaching to maintain optimal bone health. This dual approach — regular check-ups and risk reduction — is the most effective way to act before any malignancy arises.
Throughout all these strategies, understanding broader cancer dynamics helps. In fact, some of the insights drawn from how Colon Cancer Symptoms manifest have influenced screening protocols across different cancer types, including in bones.
Understanding the Role of Genetics in Bone Cancer Risk
Genetic predisposition plays a vital role in the development of primary bone cancers like osteosarcoma and Ewing sarcoma. Mutations in genes such as TP53, RB1, and RECQL4 have been linked to an increased risk of malignancies in bone tissue.
Conditions like Li-Fraumeni syndrome, Paget’s disease of bone, and hereditary retinoblastoma are strongly associated with bone tumors. Genetic counseling and testing can be essential for individuals with a strong family history of these disorders.
Here’s a table illustrating common genetic factors and their associated syndromes:
| Gene or Syndrome | Associated Cancer Risk | Recommended Action |
| TP53 mutation (Li-Fraumeni) | Osteosarcoma, soft tissue cancer | Genetic counseling, yearly MRI |
| RB1 mutation | Retinoblastoma, bone tumors | Early screening, pediatric follow-up |
| Paget’s Disease | Secondary osteosarcoma | Bone scans after age 50 |
Knowing your family’s medical history is more than helpful—it may be lifesaving if proactive monitoring is put in place.
Dietary Strategies to Support Bone Integrity

Nutrition is foundational in cancer prevention. Bones require adequate levels of calcium, vitamin D, magnesium, zinc, and vitamin K2 to stay dense and structurally stable.
Low intake of these nutrients can weaken bones, disrupt remodeling, and impair the body’s ability to repair cellular damage.
While diet alone cannot prevent malignancies, deficiencies can contribute to bone vulnerability. For instance, individuals following strict vegan diets or suffering from malabsorption syndromes are more likely to experience micronutrient deficits.
In addition, studies in veterinary medicine, including Bone Cancer in Dogs, show that nutrition also impacts tumor growth in skeletal systems, a parallel worth noting.
Lifestyle Adjustments That Reduce Overall Cancer Risk
Preventing bone cancer also involves adjusting broader lifestyle factors that influence systemic inflammation and DNA repair efficiency.
Tobacco use has been linked to poorer bone healing and increased cancer risk. Alcohol, particularly when consumed chronically, can weaken bones and alter hormonal balances.
Stress management is also essential. Chronic cortisol elevation can interfere with bone density, immunity, and cellular repair mechanisms. Incorporating mindfulness practices, ensuring restorative sleep, and staying socially connected all contribute to better health outcomes.
Even in the absence of bone-specific symptoms, these lifestyle shifts can make the body less hospitable to cancerous change across tissues.
Summary: A Holistic Blueprint for Bone Cancer Prevention
Bone cancer prevention is not a one-dimensional strategy. It requires a combination of personalized medical insight, lifestyle adjustments, and environmental awareness. Here’s a final summary in infographic format to consolidate what we’ve covered:
Infographic: Bone Cancer Prevention Layers
- Level 1: Genetic screening, personal and family history
- Level 2: Regular imaging and physical exams
- Level 3: Nutrition and supplementation
- Level 4: Physical activity and lifestyle hygiene
- Level 5: Environmental and occupational exposure control
Adopting these layers as part of daily and annual health routines empowers individuals, especially those at higher risk, to actively reduce their chance of developing malignant bone conditions.
15+ Frequently Asked Questions (FAQ)
1. Can bone cancer spread to other organs?
Yes, bone cancer can metastasize, particularly to the lungs and, less commonly, the liver or brain. The likelihood of metastasis depends on the cancer type, stage, and how early it is diagnosed. Osteosarcoma and Ewing sarcoma are known to spread through the bloodstream.
2. Is bone cancer more common in children or adults?
Bone cancer has a bimodal distribution. Primary bone cancers like Ewing sarcoma and osteosarcoma are more common in children and adolescents, while secondary bone cancers (metastases) occur more frequently in older adults due to other cancers spreading to the bones.
3. Are bone biopsies painful or risky?
Bone biopsies can be uncomfortable but are typically done under local or general anesthesia. While complications are rare, risks include infection, bleeding, or a fracture at the biopsy site.
4. Can benign bone tumors become cancerous?
Most benign bone tumors remain noncancerous. However, certain types like osteochondromas or enchondromas can very rarely evolve into malignancies, especially in people with genetic syndromes like multiple hereditary exostoses.
5. Do implants or prosthetics increase bone cancer risk?
There is no conclusive evidence that orthopedic implants or prosthetics cause bone cancer. However, older metal implants (used before regulatory advancements) may carry a slightly higher long-term risk due to wear particles.
6. Can supplements prevent bone cancer?
Supplements alone do not prevent cancer. However, adequate intake of calcium, vitamin D, and magnesium helps maintain bone structure, indirectly lowering risks related to chronic bone conditions that could evolve into malignancies.
7. How do radiation treatments for other cancers affect bones?
Radiation therapy can weaken bones in the treated area, potentially leading to radiation-induced sarcomas after several years. The risk is low but increases with high-dose exposure, especially in pediatric patients.
8. Can stress really impact bone health?
Yes, chronic stress elevates cortisol, which can reduce bone formation and increase resorption, potentially leading to osteoporosis. Although not a direct cancer risk, compromised bone health creates a less stable environment.
9. How often should someone at risk be screened?
There is no universal guideline, but individuals with genetic conditions or prior radiation exposure may require imaging every 1–2 years. Frequency should be tailored based on personal risk and doctor’s recommendation.
10. Are there any vaccines for bone cancer?
Currently, there are no vaccines specifically targeting bone cancer. However, research in cancer immunotherapy is evolving, and some trials focus on sarcoma-specific vaccine approaches.
11. Can physical trauma to a bone trigger cancer?
Trauma alone is not considered a direct cause of bone cancer. However, repeated injuries or abnormal healing in genetically predisposed individuals may increase localized mutation risk.
12. Are dogs or cats with bone cancer treated the same way as humans?
Veterinary approaches often include amputation or radiation. While the biology is different, studying Bone Cancer in Dogs and cats provides comparative insights for human medicine, especially in early detection and progression patterns.
13. What is the survival rate for bone cancer?
Survival depends heavily on the type and stage. Localized osteosarcoma has a 5-year survival rate of around 70%, while metastatic forms drop below 30%. Early detection is critical to improving prognosis.
14. Can anti-inflammatory diets help prevent cancer?
While not proven to directly prevent bone cancer, anti-inflammatory diets rich in whole foods, healthy fats, and antioxidants may reduce chronic inflammation — a contributing factor to many cancers.
15. Should athletes or physically active people worry more about bone cancer?
Not necessarily. While stress injuries are more common among athletes, they are usually benign. However, persistent pain or swelling should be examined to rule out any rare but serious conditions.












