Colon Cancer Stages
Colon Cancer Stages: What They Mean and Why They Matter
- What Is Staging in Colon Cancer and Why It Matters
- Understanding the TNM System: A Staging Framework
- Stage 0 (Carcinoma in Situ): The Earliest Warning
- Stage I: Tumor Grows but Hasn’t Spread to Lymph Nodes
- Stage II: Deeper Invasion, Still No Lymph Involvement
- Stage III: Lymph Node Spread Begins
- Stage IV: Metastatic Colon Cancer Explained
- Infographic: Progression of Colon Cancer Stages at a Glance
- How Staging Affects Treatment Planning
- Imaging Tools Used to Determine Stage
- What Happens After Surgery: Restaging and Pathology
- Survival Rates by Stage with Recent Data
- Understanding Recurrent Colon Cancer
- Role of Genetic Markers in Staging and Treatment
- How Colon Cancer Differs in Younger vs. Older Patients
- Emotional and Psychological Impact by Stage
- How to Talk to Your Doctor About Your Stage
- When a Second Opinion on Staging is Worthwhile
- Long-Term Monitoring After Initial Treatment
- Clinical Trials by Stage: What to Know
- Frequently Asked Questions (FAQ)
What Is Staging in Colon Cancer and Why It Matters
When colon cancer is diagnosed, one of the first questions asked is: “What stage is it?” The stage of cancer refers to how far the disease has spread, both within the colon and beyond. It provides essential information that guides treatment decisions and helps predict outcomes.
Staging is based on several factors:
- Tumor size and depth (how deeply it penetrates the colon wall)
- Lymph node involvement
- Spread to distant organs
Doctors use staging to:
- Choose the right therapy (surgery, chemo, etc.)
- Estimate prognosis
- Determine if clinical trials might be appropriate
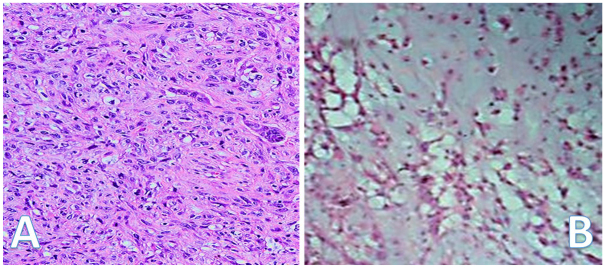
Accurate staging is achieved through pathology after biopsy or surgery, and often enhanced by imaging tests such as CT scans and Colonoscopy.
Understanding the TNM System: A Staging Framework
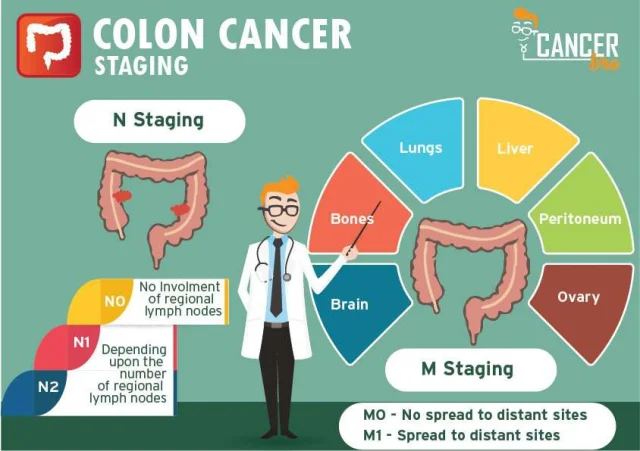
Colon cancer is most commonly staged using the TNM classification, developed by the American Joint Committee on Cancer (AJCC). It breaks down cancer characteristics into three categories:
| Component | Description | Example in Colon Cancer Context |
| T | Tumor – how deep it has grown into the colon wall | T1 = tumor in inner layers; T4 = penetrates surface |
| N | Nodes – whether nearby lymph nodes are involved | N0 = none; N1 = 1–3 nodes; N2 = 4+ nodes |
| M | Metastasis – whether it has spread to distant sites | M0 = no spread; M1 = distant spread present |
Combining T, N, and M gives the overall stage, from Stage 0 (very early) to Stage IV (advanced and metastatic). It’s a globally accepted system and allows consistency in treatment recommendations.
Stage 0 (Carcinoma in Situ): The Earliest Warning
Stage 0 is the earliest and most curable form of colon cancer. It is sometimes called carcinoma in situ, which means the cancer is still confined to the inner lining (mucosa) of the colon and has not spread beyond.
| Feature | Detail |
| Tumor penetration | Only mucosa (innermost layer) |
| Node involvement | None |
| Metastasis | None |
| Typical treatment | Local resection or polypectomy |
| Survival rate (5 years) | Close to 100% |
This stage is often discovered during a routine Colonoscopy, which can catch polyps before they evolve into invasive cancer. Because the tumor hasn’t invaded deeper tissue, surgical removal is usually curative without chemotherapy.
Stage I: Tumor Grows but Hasn’t Spread to Lymph Nodes
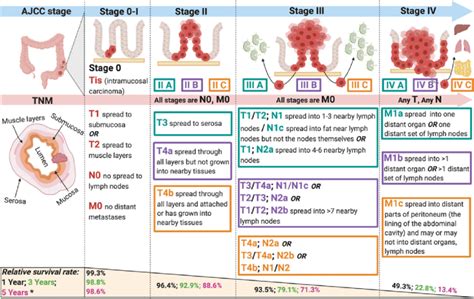
Stage I colon cancer involves tumor growth into the inner layers of the colon wall, but there is still no lymph node involvement or distant spread.
| Characteristic | Description |
| T classification | T1 or T2 (tumor invades submucosa or muscle layer) |
| Node classification | N0 (no lymph node spread) |
| Metastasis | M0 (no distant spread) |
| Typical treatment | Surgery alone (partial colectomy) |
| Prognosis | Excellent; over 90% 5-year survival |
At this stage, chemotherapy is usually not needed unless high-risk features are present (like aggressive tumor types). Stage I is often diagnosed after surgery for a polyp or suspicious mass found during screening.
Stage II: Deeper Invasion, Still No Lymph Involvement
Stage II colon cancer means the tumor has invaded the outer layers of the colon, possibly even reaching nearby tissues, but has not yet spread to the lymph nodes.
There are three substages:
| Feature | Value | ||
| Node involvement | N0 | ||
| Distant spread | M0 | ||
| Common treatment | Surgery ± adjuvant chemotherapy | ||
| Risk factor considerations | Poor differentiation, obstruction | ||
While surgery is still the primary treatment, chemotherapy may be recommended after surgery in high-risk cases (e.g., perforation, high-grade histology). The prognosis remains favorable, especially in Stage IIA.
Stage III: Lymph Node Spread Begins
Stage III colon cancer involves spread to regional lymph nodes, even if the tumor itself is small. This is a crucial turning point in staging because lymph node involvement strongly influences prognosis and treatment.
| Feature | Detail | ||
| Treatment | Surgery + adjuvant chemotherapy | ||
| Common chemo regimen | FOLFOX or CAPOX | ||
| 5-year survival range | 53–89%, depending on node count | ||
The number of lymph nodes involved (N1 vs N2) significantly impacts the risk of recurrence. Stage III is typically when systemic therapy becomes standard, not just local surgical excision.
Stage IV: Metastatic Colon Cancer Explained
Stage IV means the cancer has spread to distant organs such as the liver, lungs, peritoneum, or distant lymph nodes. It is the most advanced stage, but new treatments have improved survival significantly.
| Feature | Stage IVA | Stage IVB | Stage IVC |
| Distant metastases | 1 site (e.g., liver) | More than 1 organ site | Peritoneal + other organs |
| Node status | Any | Any | Any |
| Typical treatment | Chemo ± targeted therapy | May include surgery or ablation | Palliative + immunotherapy trials |
| Median survival (2024 data) | 30–36 months (if responsive) | 15–30 months | <12 months (without response) |
While Stage IV is not typically curable, a subset of patients with limited liver or lung metastases may achieve long-term remission with aggressive therapy. This is a key area of ongoing research and clinical trial focus.
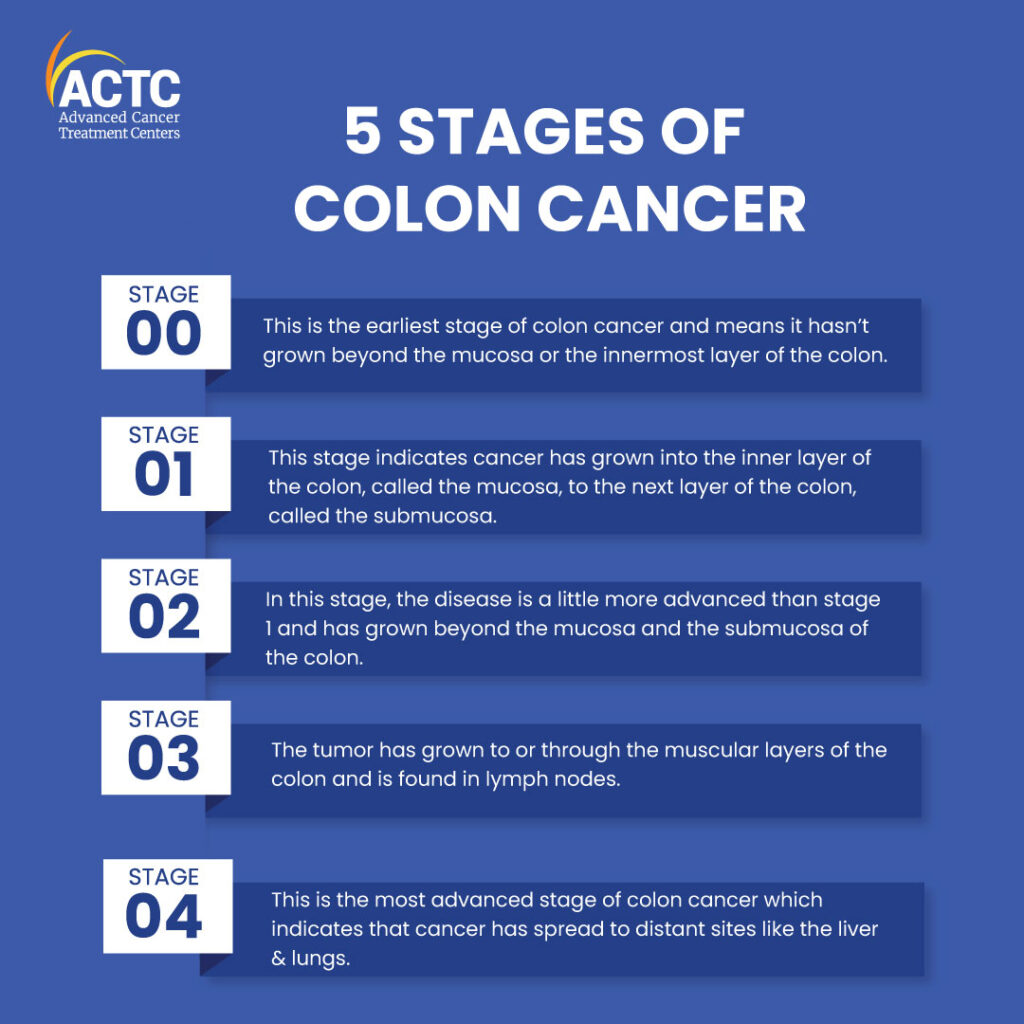
Infographic: Progression of Colon Cancer Stages at a Glance
Below is a simplified visual progression of how colon cancer evolves through stages
| Stage 0 | Mucosal layer only | No nodes | No spread |
| Stage I | Inner muscle layer | No nodes | No spread |
| Stage II | Deeper colon wall/layers | No nodes | No spread |
| Stage III| Any tumor + lymph nodes | Yes | No spread |
| Stage IV | Any tumor + distant spread | Yes/No | Yes |
This conceptual overview helps new patients understand how staging works and why each stage matters in guiding treatment and survival planning.
Further study is being conducted to understand how Colon Cancer in Women develops, taking into account differences in symptoms and diagnosis between the sexes.
How Staging Affects Treatment Planning
The stage of colon cancer not only predicts survival outcomes but also directly influences the treatment approach. Early-stage cancers often require surgery alone, while advanced stages necessitate chemotherapy, radiation, or targeted therapies.
| Stage | Standard Treatment | Additional Notes |
| Stage 0 | Polypectomy or local excision | No chemo needed |
| Stage I | Surgical resection | Adjuvant therapy rarely required |
| Stage II | Surgery ± chemotherapy | Based on risk factors (e.g., obstruction) |
| Stage III | Surgery + chemotherapy (FOLFOX/CAPOX) | Lymph node involvement dictates regimen strength |
| Stage IV | Chemo ± surgery ± biologics | Metastasis location defines treatment complexity |
Treatment decisions may also involve multidisciplinary tumor boards, combining insights from surgeons, oncologists, radiologists, and pathologists to tailor strategies.
Imaging Tools Used to Determine Stage
Accurate staging requires a combination of radiological and pathological tools. Before and after surgery, various imaging techniques help assess tumor size, lymph node involvement, and metastasis.
| Imaging Modality | Role in Staging | Common Use Case |
| CT scan (abdomen/pelvis) | Detect distant metastases, lymphadenopathy | Preoperative baseline scan |
| MRI | Evaluate rectal involvement, liver lesions | Detailed local and liver assessment |
| PET-CT | Assess active disease or recurrence | Advanced staging or unclear metastasis origin |
| Endoscopic ultrasound | Evaluate depth of tumor penetration | Limited to rectal cancer |
What Happens After Surgery: Restaging and Pathology
After colon cancer surgery, the removed tissue undergoes a thorough pathological analysis to confirm and sometimes adjust the original clinical stage. This process is called restaging.
| Surgical Outcome | Impact on Stage |
| More lymph nodes found | May upstage from N0 to N1/N2 |
| Unexpected invasion | May upgrade T classification |
| Clean margins | Confirms completeness of resection |
| Lymphovascular invasion | Indicates higher recurrence risk |
Pathologists also check for molecular markers such as microsatellite instability (MSI) or KRAS/NRAS mutations, which influence further treatment and prognosis.
Survival Rates by Stage with Recent Data
Survival rates are directly linked to the stage at diagnosis. Early-stage colon cancers have excellent outcomes, while late-stage survival is improving due to advancements in systemic therapy.
| Stage | 5-Year Survival Rate (U.S. SEER Data) |
| Stage 0 | ~99% |
| Stage I | ~90–95% |
| Stage II | ~75–87% |
| Stage III | ~53–89% (varies by lymph node count) |
| Stage IV | ~14% (but improving with therapy) |
Important factors like age, tumor genetics, surgical success, and access to modern treatment centers also affect survival. As research progresses, even Stage IV patients may live many years with appropriate care.
Understanding Recurrent Colon Cancer
Even after successful treatment, colon cancer can return — this is known as recurrent colon cancer. Recurrence may happen locally, in the lymph nodes, or in distant organs. Staging plays a major role in assessing recurrence risk.
| Recurrence Type | Description | Common Sites |
| Local recurrence | Cancer returns near the original tumor site | Surgical site in colon |
| Regional recurrence | Affects nearby lymph nodes | Mesenteric or pelvic lymph nodes |
| Distant recurrence | Metastasis appears in other organs | Liver, lungs, peritoneum |
Recurrent cancers are often restaged and evaluated for additional treatment, including repeat surgery, radiation, or systemic therapy. Surveillance protocols differ by stage, but high-risk patients often undergo imaging and colonoscopy every 6–12 months.
Role of Genetic Markers in Staging and Treatment

Modern colon cancer care integrates molecular profiling into staging and treatment decisions. Genetic mutations and markers don’t affect the TNM stage directly but refine prognosis and guide therapy.
| Genetic Marker | Implication in Colon Cancer | Therapeutic Relevance |
| MSI (Microsatellite Instability) | Predicts better prognosis in early stages | Indicates poor response to 5-FU |
| KRAS / NRAS mutation | Present in ~40% of tumors | Predicts non-response to EGFR inhibitors |
| BRAF mutation | Associated with poor outcomes | May guide use of combination therapy |
| p53 / APC loss | Common tumor suppressor mutations | Still under investigation |
Patients with Stage II tumors that have high microsatellite instability may safely skip chemo, while certain targeted agents are only given if specific mutations are present.
How Colon Cancer Differs in Younger vs. Older Patients
Though colon cancer is most common after age 50, cases in younger individuals (under 45) are rising. These younger patients often present at later stages and may have more aggressive tumors.
| Characteristic | Younger Patients (<45) | Older Patients (>65) |
| Presentation | Often late-stage, misdiagnosed initially | Usually early, due to routine screening |
| Tumor biology | More aggressive features (mucinous, signet ring) | Standard adenocarcinoma |
| Family history | More common | Less frequent |
| Access to screening | Limited due to age | Widely available (via Medicare, etc.) |
As a result, younger patients often require genetic counseling and tailored follow-up. Early signs like rectal bleeding or unexplained weight loss should never be ignored, regardless of age.
Emotional and Psychological Impact by Stage
Staging doesn’t just define medical strategy—it shapes how patients emotionally process their diagnosis. A Stage I diagnosis may bring relief and confidence, while Stage IV can lead to shock, anxiety, or despair.
| Stage | Common Emotional Responses | Support Resources |
| Stage I–II | Relief, fear of recurrence, confusion about follow-up | Survivorship clinics, peer support |
| Stage III | Anxiety, chemo-related distress, lifestyle changes | Oncology social workers, counseling |
| Stage IV | Grief, depression, hope in innovation | Palliative care, mental health support |
Patients and families benefit from early integration of psychological support, no matter the stage. Addressing mental health needs improves quality of life and treatment adherence.
How to Talk to Your Doctor About Your Stage
Understanding your colon cancer stage can be overwhelming. To make informed decisions, clear communication with your oncology team is essential. Knowing what to ask helps you gain clarity, understand risks, and feel more in control.
| Discussion Point | What to Ask or Clarify |
| Stage classification | “Can you explain what my stage means in plain terms?” |
| Imaging and biopsy results | “What tests confirmed this stage? Are more needed?” |
| Treatment goals | “Is the plan curative, preventive, or palliative?” |
| Need for second opinion | “Would another pathologist review the biopsy?” |
| Molecular testing | “Were my tumor genetics tested, and how does that affect treatment?” |
Doctors appreciate when patients come prepared. Keep a written list of concerns and bring a companion to appointments when possible to absorb more information and ask additional questions.
When a Second Opinion on Staging is Worthwhile
Staging errors are rare but can occur due to limited imaging, incomplete pathology, or discrepancies in tumor interpretation. A second opinion may uncover more precise staging or open up alternative treatments.
| Reason to Seek Second Opinion | Potential Benefit |
| Unclear imaging or conflicting reports | Better radiologic assessment |
| Rare or aggressive tumor subtypes | Access to specialized pathology review |
| Unusual molecular features | Referral to academic or clinical trial center |
| Patient hesitation or lack of trust | Rebuilding confidence and clarity |
Large cancer centers often offer second-opinion services remotely or through multidisciplinary teams. This is especially helpful for Stage II and Stage IV patients where nuances in staging affect treatment choice.
Long-Term Monitoring After Initial Treatment
After successful treatment, ongoing surveillance is critical to catch recurrence early and monitor for secondary tumors. The intensity of follow-up depends on the original stage.
| Stage at Diagnosis | Surveillance Frequency (Years 1–3) | Tools Used |
| Stage I | Every 6–12 months | Colonoscopy, bloodwork |
| Stage II–III | Every 3–6 months | CT scans, CEA tests, colonoscopy |
| Stage IV | Every 2–3 months | Imaging, tumor markers |
Beyond 3–5 years, intervals may widen, especially for Stage I or II survivors. However, patients with genetic syndromes or aggressive features may need lifelong monitoring.
Clinical Trials by Stage: What to Know
Clinical trials offer cutting-edge therapies not yet available to the public. Patients at nearly every stage can qualify — even those with Stage I (for prevention) or Stage IV (for experimental treatments).
| Stage | Common Trial Focus |
| Stage I–II | Chemoprevention, minimal adjuvant therapy |
| Stage III | New combinations of chemo or immunotherapy |
| Stage IV | Targeted agents, biologics, novel drug delivery |
You can search for trials at clinicaltrials.gov or ask your oncologist. Enrollment often depends on specific mutations, prior treatments, and overall health. For Stage IV patients, trials can be a lifeline offering improved survival and quality of life.
Frequently Asked Questions (FAQ)
1. Can colon cancer be completely cured if detected early?
Yes, colon cancer detected at Stage 0 or Stage I can often be completely cured through surgical removal alone, with long-term survival rates exceeding 90%. These early-stage tumors are confined to the inner lining or superficial layers of the colon and have not yet spread to lymph nodes or distant sites. However, continued surveillance is still essential to detect any future changes or new polyp formation.
2. What does a CEA blood test indicate in colon cancer?
CEA (carcinoembryonic antigen) is a protein that can be elevated in colon cancer patients, especially in more advanced stages. While it is not suitable for screening or diagnosis on its own, it is widely used in follow-up care to detect recurrence or monitor response to treatment. A rising CEA level after surgery or chemotherapy may warrant further imaging to investigate recurrence.
3. How long does it take for colon cancer to progress from Stage I to Stage IV?
The rate of progression varies widely between individuals, depending on tumor biology, genetics, immune response, and environmental factors. In general, it can take several years for early-stage colon cancer to progress to metastatic disease. This long latency underscores the importance of routine screening and prompt treatment when abnormalities are detected.
4. Can colon cancer spread without lymph node involvement?
Yes, although lymph node spread is the most common route of metastasis, colon cancer can sometimes spread directly through the bloodstream or invade adjacent organs without lymph node involvement. This is more likely in high-grade or aggressive tumors. For example, liver metastases may appear even in the absence of nodal disease, particularly in certain molecular subtypes.
5. What are the risks of recurrence after treatment?
Recurrence risk depends on the original stage, tumor grade, and completeness of surgery. For Stage I cancers, the risk is very low, often under 5%. In Stage III or IV, the risk can be 30–60%, depending on how many lymph nodes were involved and whether adjuvant therapy was used. Close surveillance helps detect recurrence early when it’s still manageable.
6. Is radiation therapy used for colon cancer?
Radiation therapy is not commonly used for colon cancer except in select cases such as locally advanced tumors that invade adjacent organs, or recurrent disease confined to a specific site. It is more routinely applied in rectal cancer due to anatomical differences. In colon cancer, systemic chemotherapy is generally more effective for disease control.
7. How does obesity affect colon cancer prognosis?
Obesity is a known risk factor for developing colon cancer and is also associated with worse outcomes in diagnosed patients. Increased body fat can affect drug metabolism, immune response, and tumor environment. Obese patients often have higher rates of postoperative complications and may respond differently to chemotherapy.
8. What are the symptoms of Stage IV colon cancer?
Stage IV colon cancer may present with systemic symptoms such as unexplained weight loss, chronic fatigue, abdominal distention, liver enlargement, or persistent pain. Depending on the organs affected, patients may also experience coughing (lung metastases), jaundice (liver metastases), or bowel obstruction. These signs often develop gradually and may be overlooked without imaging.
9. Can colon cancer come back after 10 years?
While most recurrences occur within 5 years after initial treatment, very late recurrences are possible, though rare. Patients with certain genetic mutations or hereditary colon cancer syndromes may remain at risk for life. This is why long-term surveillance, though less frequent after 5 years, still plays a role in high-risk populations.
10. Are there any vaccines for colon cancer prevention?
There is no approved vaccine specifically for colon cancer at this time, but research is underway. Some experimental vaccines target tumor-associated antigens or immune pathways to prevent recurrence or boost immune responses after treatment. Preventive vaccines are being explored in people with familial adenomatous polyposis (FAP) and Lynch syndrome.
11. Does stress increase the risk of colon cancer?
There is no direct link between emotional stress and colon cancer development. However, chronic stress may indirectly contribute by promoting unhealthy behaviors such as poor diet, lack of exercise, smoking, or delayed medical visits. Moreover, psychological distress may affect recovery and adherence to treatment in diagnosed patients.
12. Is colon cancer hereditary?
While most cases are sporadic, about 5–10% of colon cancers are hereditary. Conditions such as Lynch syndrome (HNPCC) and familial adenomatous polyposis (FAP) significantly increase lifetime risk. If a first-degree relative has been diagnosed, particularly before age 50, genetic counseling and early screening are strongly advised.
13. Can lifestyle changes prevent colon cancer recurrence?
Yes. Adopting a high-fiber, low-red-meat diet, maintaining a healthy weight, engaging in regular physical activity, and avoiding tobacco and excessive alcohol can help reduce recurrence risk. These changes also improve overall health, immune function, and tolerance to follow-up treatments like chemotherapy.
14. What is the difference between colon and rectal cancer?
Although they both fall under the category of colorectal cancer, colon and rectal cancers differ in anatomy, treatment strategies, and recurrence patterns. Rectal cancer often requires radiation due to its confined location in the pelvis, while colon cancer is more likely treated with surgery and systemic therapy. Surgical techniques also vary due to differences in access and lymphatic drainage.
15. Can colon cancer be detected in a routine blood test?
Routine blood tests such as CBC or liver function panels may show indirect signs (like anemia), but they cannot diagnose colon cancer. Specialized markers like CEA help in monitoring but are not diagnostic. The gold standards for detection are colonoscopy and imaging modalities, which provide direct visualization of the colon and any suspicious lesions.